Abstract
Distant breast cancer metastases are nowadays routinely biopsied to reassess receptor status and to isolate DNA for sequencing of druggable targets. Bone metastases are the most frequent subgroup. Decalcification procedures may negatively affect antigenicity and DNA quality. We therefore evaluated the effect of several decalcification procedures on receptor status and DNA/RNA quality. In 23 prospectively collected breast tumors, we compared ERα, PR and HER2 status by immunohistochemistry in (non-decalcified) tissue routinely processed for diagnostic purposes and in parallel tissue decalcified in Christensen’s buffer with and without microwave, EDTA and Formical-4. Furthermore, HER2 fluorescence in situ hybridization and DNA/RNA quantity and quality were assessed. We found that the percentage of ERα-positive cells were on average lower in EDTA (P=0.049) and Formical-4 (P=0.047) treated cases, compared with controls, and PR expression showed decreased antigenicity after Christensen’s buffer treatment (P=0.041). Overall, a good concordance (weighted kappa) was seen for ERα, PR and HER2 immunohistochemistry when comparing the non-decalcified control tissues with the decalcified tissues. For two patients (9%), there was a potential influence on therapeutic decision making with regard to hormonal therapy or HER2-targeted therapy. HER2 fluorescence in situ hybridization interpretation was seriously hampered by Christensen’s buffer and Formical-4, and DNA/RNA quantity and quality were decreased after all four decalcification procedures. Validation on paired primary breast tumor specimens and EDTA-treated bone metastases showed that immunohistochemistry and fluorescence in situ hybridization were well assessable and DNA and RNA yield and quality were sufficient. With this, we conclude that common decalcification procedures have only a modest negative influence on hormone and HER2 receptor immunohistochemistry in breast cancer. However, they may seriously affect DNA/RNA-based diagnostic procedures. Overall, EDTA-based decalcification is therefore to be preferred as it best allows fluorescence in situ hybridization and DNA/RNA isolation.
Similar content being viewed by others
Main
Multiple studies have shown that the expression of predictive tissue markers, such as estrogen receptor alpha (ERα), progesterone receptor (PR) and human epidermal growth factor receptor-2 (HER2) may differ between the primary tumor and distant metastases (‘receptor conversion’) in a significant proportion of breast cancer patients.1, 2, 3 Therefore, several guidelines nowadays advice to biopsy distant metastases to reassess hormone and HER2 receptor status by immunohistochemistry whenever possible.4, 5 However, in bone metastases this could potentially lead to inappropriate systemic treatment, as antigenicity may be altered by decalcifying agents that enable sectioning of bone.6, 7 On the other hand, some studies report that decalcifying methods can be applied without significant loss of immunoreactivity.8, 9 The same contradictory results about influence of decalcifying buffers have been seen when RNA or DNA integrity and interpretation of in situ hybridization were taken into account.10, 11, 12, 13, 14
These inconsistencies may be explained by usage of different decalcifying agents. Strong acids such as hydrochloric and nitric acid are traditionally widely used for their rapid decalcifying properties, but they are known to have a detrimental influence on immunoreactivity and DNA integrity.15 Therefore, weak(er) acidic buffers, containing formic or trichloracetic acid, are now more popular. EDTA, a chelating agent with neutral pH, requires longer time periods for the complete removal of calcium salts but produces the best morphological results.8 Singh et al11 recently tested 10 commercially available decalcifying agents and concluded that the best preservation of nucleic acids is achieved with decalcifying agents that contain either EDTA or formic acid or a combination of both.
As bone is a frequent metastatic site among breast cancer patients,16, 17 we set out to evaluate the influence of three routinely used decalcifying agents (containing formic acid and/or EDTA) on assessment of hormone and HER2 receptor status and DNA/RNA quality in breast cancer.
Materials and methods
Materials
Prospectively, tissue from 23 breast tumors was collected and processed according to routine procedures at the Department of Pathology of the University Medical Center Utrecht, The Netherlands. Original diagnoses were made between August 2012 and July 2015. Clinicopathological characteristics are shown in Table 1 (test cohort).
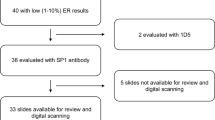
Four tumor biopsies (0.4–0.8 cm3 in size) were removed from each breast tumor (Figure 1). All tissue samples were fixed in 4% buffered formaldehyde for 24–48 h. After fixation, breast cancer tissue collected for diagnostic purposes was processed according to a standard protocol and embedded in paraffin. The additional biopsies of the tumors were processed in Christensen’s buffer (containing formic acid and sodium formate), EDTA disodium salt dehydrate (EDTA) or Formical-4 (containing formic acid, formaldehyde and methanol). Tissue was placed in Christensen’s buffer or Formical-4 overnight in a microwave (Christensen’s buffer with microwave) at 37 °C and in EDTA overnight at room temperature on a shaker. To assess the influence of the microwave, one of the biopsies was treated with Christensen’s buffer but withheld from the microwave. Hereafter, all the tissue fragments were washed thoroughly in running tap water, placed in 70% EtOH and routinely processed to paraffin. For each formalin-fixed paraffin-embedded fragment, a 4-μm hematoxylin and eosin-stained slide was reviewed by a single pathologist (PvD) to confirm the presence of malignancy. Because biopsies were taken macroscopically, tumor was not always present (indicated by empty spaces in Tables 2 and 4 and Supplementary Table S1). Tumor-negative biopsies were excluded.
Overview of material and methods. Four tumor-containing biopsies were taken from breast tumor resection specimens (n=23). Each biopsy was placed in a different decalcifying agent, including EDTA, Christensen’s buffer with microwave (CBM), Christensen’s buffer without microwave (CB) and Formical-4 (F4). The original non-decalcified tumor was used as a control. Specimens were formalin fixed and paraffin embedded after which sections were cut for immunohistochemistry (IHC), fluorescence in situ hybridization (ISH) and DNA/RNA isolation.
The use of left-over material requires no ethical approval according to (‘opt-out’) Dutch legislation. Use of anonymous or coded left-over material for scientific purposes is part of the standard treatment contract with patients and therefore informed consent was not required.18
Immunohistochemistry
Immunohistochemistry for ERα, PR and HER2 was carried out on full 4-μm sections with the Ventana autostainer (Roche, Tucson, USA) according to the manufacturer’s instructions. Rabbit monoclonal antibodies used were against ERα (RTU, SP1; Roche), PR (RTU, 1E2; Roche) and HER2 (1:50, SP3; ThermoFisher Scientific, Bleiswijk, The Netherlands). Appropriate controls were used throughout.
Scoring
Scoring of immunohistochemically stained slides was performed by mutual agreement of two observers (PvD and WS) in random order, blinded to other data in the paired samples. For ERα and PR, the percentage of positively stained nuclei was assessed. The adequacy of staining was checked by also evaluating the normal breast parenchyma. Samples with ≥10% immune-positive malignant cells were classified as ERα or PR positive. In order to also comply with the ASCO guidelines, we also used the 1% threshold that is now widely used in the United States of America. HER2 expression was scored using the DAKO scoring system as 0, 1+, 2+ and 3+. HER2 expression was considered positive when 3+.
Immunohistochemically assessed surrogate molecular subtypes of breast tumors were assigned as follows: Luminal A (ER+/PR+, HER2−, Ki-67<15), luminal B (ER+/PR+, HER2−, Ki-67>15 or ER+/PR+, HER2+), triple-negative or basal type (ER−/PR−, HER2−), and HER2 enriched (ER−/PR−, HER2+).
Morphology was judged visually based on the hematoxylin and eosin-stained slide, with special emphasis on visibility of mitoses, nuclear morphology and staining intensity of stroma and epithelium.
In Situ Hybridization
According to routine diagnostic procedures, cases with HER2 expression of 2+ or 3+ (patients #4, #5, #6 and #16) were subjected to fluorescence in situ hybridization using a HER2/CEP17 dual FISH probe (Cytocell) on 4-μm slides. Analysis was performed on a Leica DM5500 B microscope system with the Application Suite Advanced Fluorescence Software (Leica Microsystems, Rijswijk, The Netherlands).
In short, formalin-fixed paraffin-embedded slides were deparaffinized and pretreated with citrate and protease buffers. Next they were dehydrated and hybridized with 10-μl fluorescence in situ hybridization probe in a ThermoBrite (Abbott Laboratories, Chicago, IL, USA) at 37 °C overnight. The next day, slides were washed in saline-sodium citrate buffers, counterstained with DAPI, dehydrated and mounted with Vectashield Mounting Medium (Vector Laboratories, Burlingame, CA, USA). One hundred tumor cell nuclei per tumor were assessed for HER2 gene and CEP17 probe signals at × 100 magnification. The HER2/CEP17 ratio was calculated as well. A ratio <1.8 was defined as a normal copy number, a ratio of 1.8–2.2 as an equivocal copy number and a ratio >2.2 as gene amplification, as described in the ASCO and CAP guidelines.19
DNA and RNA Extraction
The hematoxylin and eosin-stained section from each formalin-fixed paraffin-embedded tissue block was used to guide macro-dissection for DNA and RNA extraction and to estimate tumor percentage. On average, 10 and 5 10-μm-thick slides were cut for DNA and RNA isolation, respectively (number depending on tumor percentage and size). Because the different biopsies and tumor samples differ in cellularity and size, normalization of input for DNA/RNA isolation was performed by correcting for tumor area and percentage.
After deparaffinization in xylene, tumor areas were macro-dissected using a scalpel, and areas with necrosis, dense lymphocytic infiltrates and preinvasive lesions were intentionally avoided. For DNA isolation, the dissected tissue was placed in 1 M NaSCN overnight, after which proteinase K-based extraction was performed according to the QIAamp DNA FFPE Tissue Kit (Qiagen). RNA extraction was performed according to the miRNeasy FFPE Kit (Qiagen). Total DNA and RNA concentration were measured by a spectrophotometer (Nanodrop ND-1000, Thermo Scientific Wilmington, DE, USA) and a fluorometer (Qubit 2.0 Fluorometer, Life Technologies, Bleiswijk, The Netherlands), the latter using the Qubit dsDNA HS Assay Kit and RNA Assay Kit. Absorbance at 230, 260 and 280 nm was evaluated (Nanodrop) and the RNA Integrity Number was determined using the Agilent RNA 6000 Nano Kit on the Bioanalyzer (Agilent).
DNA Quality
To assess DNA quality and the presence of inhibitors, the QuantideX qPCR DNA QC Assay (Asuragen, Austin, USA) was used. This is a multiplex qPCR assay with one channel (FAM) that detects an 82-bp amplicon from the TBP gene, which assesses DNA quality and quantity, and with another channel (VIC/HEX) that detects a non-human amplicon spiked into each sample, to evaluate the presence of inhibitors. To determine the target copy number in a tested sample, a standard curve was established in every run using DNA standards at 50, 10, 2 and 0.4 ng/μl in duplicate.
The QuantideX assay determines the functional quality of sample DNA using the Quantitative Functional Index (QFI) Score, which is the fraction of total genomic DNA copies that can be PCR amplified,20 and the quality using the amplifiable copy number.
Size Ladder PCR
To determine DNA fragmentation, a size ladder PCR was performed using the Specimen Control Size Ladder Kit (In Vivo Scribe, Huissen, The Netherlands) on the Veriti Thermal Cycler (Applied Biosystems, Bleiswijk, The Netherlands) with a 35 cycle PCR reaction. DNA input was corrected for the amplifiable copy number measured with the QuantideX assay. The PCR product was mixed with Hi-Di Formamide and ROX500 and analyzed on the 3730 DNA Analyzer (ThermoFisher Scientific). Results were processed with the Genescan software (ThermoFisher Scientific).
Validation in Paired Breast Tumors and Bone Metastases
To validate these findings on real metastases, we retrospectively selected formalin-fixed paraffin-embedded material of bone metastases from eight patients from our diagnostic pathology archives. Original diagnoses of the primary tumors were made between January 2002 and January 2015 and of the bone metastases between September 2013 and May 2015. All obtained bone metastases were biopsies taken from vertebrae or pelvis, and pathological records disclosed decalcification in EDTA for 5 h to overnight according to routine procedures. Matching primary tumor material was available for four of these patients to allow comparison of receptor staining between primary tumors and bone metastases. Patient characteristics are listed in Table 1 (validation cohort). These samples were subjected to immunohistochemistry, fluorescence in situ hybridization and DNA/RNA quality and quantity assessment as mentioned before.
Statistics
Results obtained by immunohistochemistry were compared by cross tables, and the concordance percentages and linear weighted kappa-scores were calculated. Concordance was categorized as follows: (almost) perfect (kappa: 0.8–1), substantial (kappa: 0.6–0.8), moderate (kappa: 0.4–0.6), and poor concordance (kappa 0–0.4). In addition, median percentages, 260/280 ratios and RNA Integrity Number were compared using the Wilcoxon signed-rank test. P-values >0.05 were considered significant. All statistical calculations were carried out with IBM SPSS Statistics 21 and visualized with GraphPad Prism 6.
Results
Immunohistochemistry
Table 2 shows immunohistochemical expression of ERα, PR and HER2 in the 23 breast tumors per preanalytic condition (control/no treatment, Christensen’s buffer (with and without microwave), Formical-4 and EDTA). ERα positivity was seen in 87 or 95.7% of the controls and PR positivity in 69.6 or 82.6%, using a 10 or 1% threshold for positivity, respectively. HER2 positivity was seen in 13% of controls.
For ERα, exact staining percentages tended to be lower in EDTA (P=0.049) and Formical-4 (P=0.047) treated cases, compared with the control. For PR expression, only Christensen’s buffer-treated tissue showed decreased antigenicity (P=0.041). However, as conversion from positive in the control to negative in the decalcified tissue is clinically most important, concordance of relative expression was checked with linear weighted kappa. Overall, a substantial to perfect concordance was seen for ERα, PR and HER2 when comparing the controls with all decalcified tissues, with some variation between 1 and 10% thresholds for positivity (2/23 differing cases for ERα and 5/23 for PR) (Tables 2 and 3 and Supplementary Tables S1 and S2; Figure 2). Especially, some drop in antigenicity was seen in the Christensen’s buffer-treated tissue for PR (kappa 0.571; 1% threshold) and HER2 (0.493; exact DAKO scores) in the EDTA-treated tissue for ERα (kappa 0.462; 1% threshold) and in the Formical-4-treated group for PR (no concordance at all).
Clinically relevant changes (from positive to negative) occurred for ERα in one patient (4%; with Christensen’s buffer with microwave and EDTA) when the 1% threshold for positivity was used, but none was seen for the 10% threshold. For PR, a change from positive to negative appeared in two patients with the 10% threshold (in patient #1 for Christensen’s buffer with and without microwave and EDTA and in patient #18 for Christensen’s buffer only) and in two patients with the 1% threshold (in patient #2 and #3 for Christensen’s buffer with and without microwave and EDTA). Furthermore, the Formical-4-treated tissue showed a serious discordance in PR antigenicity. However, two cases out of this group of nine (patient #16 and #17) showed a change from negative in the control to positive with Formical-4.
Nuclear, stromal and epithelial morphology and staining intensity did not seem to differ between samples treated with different buffers (Figure 2).
In Situ Hybridization
Four control tissues showed a 2+ or 3+ HER2 expression by immunohistochemistry and were subjected to fluorescence in situ hybridization. Comparison of HER2 status by immunohistochemistry and fluorescence in situ hybridization in control tissue compared with decalcified tissues is shown in Supplementary Table S3. Three HER2 immunohistochemistry-positive cases appeared fluorescence in situ hybridization negative in the control and the decalcified samples. In all cases, cell morphology and signal interpretation were severely affected by Christensen’s buffer with microwave and Formical-4 buffers, as depicted in Figure 3. Interpretation of the fluorescence in situ hybridization slides was least hampered by EDTA treatment.
RNA and DNA Integrity
Because the biopsies and original tumor samples differ in cellularity and size, we tried to approximate equal tumor input. Paired differences between DNA and RNA yield obtained from tissue treated with different decalcifying agents resembled in pattern between Qubit, Nanodrop and Bioanalyzer (Supplementary Figure S1 and Supplementary Table S4). For both DNA and RNA, highest yields were seen for control tissue, followed by EDTA-treated tissue.
For RNA, 260/280 ratios were significantly higher in the control and the EDTA-treated samples compared with the other decalcifying agents (Figure 4a). The RNA Integrity Number did not vary much, although EDTA-treated material showed significantly higher values compared with control samples (P=0.019; Figure 4b).
Quality and quantity of RNA and DNA isolated from tissue pretreated with EDTA, Christensen’s buffer with (CBM) and without microwave (CB) and Formical-4 (F4; n=23). (a) 260/280 ratios for RNA, measured by Nanodrop. (b) Bioanalyzer RNA Integrity Number (RIN) values. (c) 260/280 ratios for DNA, measured by Nanodrop. (d) QFI (Quantitative Functional Index) in percentages (actual copy number/expected copy number, based on quantity of DNA measured by Nanodrop). (e) Average DNA fragment length in base pairs, measured with size ladder PCR. DNA input is corrected for amplifiable copy number, measured with the QuantideX qPCR assay. *P<0.05; **P<0.01; ***P<0.001.
Also for DNA, 260/280 ratios were significantly higher in the control and EDTA-treated samples, compared with the other decalcified tissues (Figure 4c). With the QuantideX assay, inhibition was only seen in Formical-4-treated samples (5/9 samples). DNA quality based on amplifiable copies was severely affected by all three decalcifying agents, with the largest drop in copy number for Formical-4, Christensen’s buffer with and without microwave, respectively (Supplementary Figure S2A). When this number was corrected for expected copy number (based on Nanodrop measurements), the same pattern was observed (QFI; Figure 4d). The size ladder PCR (with input corrected for amplifiable copies) showed a decreased DNA fragment length in Christensen’s buffer with and without microwave-treated samples compared with the control (Figure 4e). This average decrease seemed to be caused mainly by loss of 90-, 200- and 300-bp fragments (Supplementary Figure S2B). Samples decalcified with Formical-4 showed hardly any amplifiable copies, leading to uninterpretable size ladder PCR data.
Validation in Paired Breast Tumors and Bone Metastases
All primary tumors and bone metastases were ERα positive and no significant differences were perceived between absolute ERα staining percentages. Also, no significant differences were seen in PR staining percentages, although patient #1 had a PR-negative primary tumor and a PR-positive metastasis. No discordance was observed between HER2 immunohistochemistry and fluorescence in situ hybridization (Table 4; Supplementary Figure S3). Furthermore, nuclear, stromal and epithelial morphology and staining intensity did not differ between primary tumors and EDTA-treated bone metastases.
Paired analyses of DNA and RNA quality and quantity as measured with Nanodrop, Qubit and Bioanalyzer (corrected for tumor percentage) between primary tumors and metastases did not point to significant differences (Figure 5). When DNA fragmentation was compared, two primary tumor samples showed a smaller fragment length. Both samples originated from 2002, while all others were diagnosed between 2011 and 2015.
Yield of RNA and DNA, isolated from tissue from paired primary tumors and paired EDTA-treated bone metastases (n=8) measured with Nanodrop, Qubit and Bioanalyzer. Tumor areas were normalized and RNA and DNA yield corrected for tumor percentage. Paired differences were calculated with Wilcoxon signed-rank test. (a) RNA yield, measured by Nanodrop, Qubit and Bioanalyzer; (b) DNA yield measured by Nanodrop, Qubit and size ladder PCR.
Discussion
The occurrence of receptor conversion between the primary breast carcinoma and corresponding distant metastases has been widely accepted.21 Therefore, most guidelines now advise to biopsy a distant metastasis at presentation of metastatic disease.4, 5 This is challenging when metastasis is located in the bone, as the decalcification process could potentially compromise antigenicity and may, as such, hamper interpretation of (molecular) diagnostics. With an incidence of 6–22% in 5.4–8.4 years of follow-up,16, 17 bone is one of the most common metastatic sites among breast cancer patients, which emphasizes the relevance of this subject.
In the present study, we demonstrate that immunohistochemistry of ERα, PR and HER2 is not much affected by tissue decalcification with agents containing formic acid or EDTA. However, quantity and quality of isolated DNA and RNA is affected by all three decalcification buffers tested, although EDTA can be used when results are interpreted with caution. In line with this, HER2 fluorescence in situ hybridization could only be interpreted in EDTA-treated tissue. We validated these findings in eight patients with paired primary breast tumors and EDTA-treated bone metastases. Immunohistochemistry, fluorescence in situ hybridization and DNA/RNA quality and quantity were comparable in paired cases, validating the EDTA protocol in real life.
To our knowledge, this is the first study to describe the influence of multiple decalcifying agents on both immunohistochemistry, fluorescence in situ hybridization and DNA/RNA integrity in the same breast cancer patients in a relative large cohort. A previous study based on 10 decalcified breast cancer samples reported an overall negative impact on ERα and PR staining intensity, which affected the staining detectability and therefore proportion of tumor cell staining.22 However, time of decalcification was merely 1 h in contrast to our protocol of overnight decalcification, which approximates the normal diagnostic situation in our clinic. Additionally, Gertych et al23 performed decalcification of breast cancer tissue (n=9) during several periods of time and saw the largest decrease in antigenicity in the first 6 h. Likewise, we observed an absolute decrease in staining percentages for ERα (EDTA- and Formical-4-treated tissues) and PR (Christensen’s buffer-treated tissue). However, this decrease is only clinically relevant when it affects potential treatment decision making; in other words, when a change is achieved from positive to negative. In our study, this was the case for ERα in one patient (4% of cases) when the 1% threshold for positivity was used. Therefore, we advise to use the 10% threshold, as this leads to fewer falsely stratified patients for hormonal therapy, especially in decalcified tissue. For PR, a change from positive to negative appeared in two patients with the 10% threshold and in two patients with the 1% threshold. However, in three of these cases ERα was still positive, so no influence on treatment decision making was imposed. Furthermore, the Formical-4-treated tissue showed a serious discordance in PR antigenicity. However, two cases showed a change from negative in the control to positive with Formical-4, which can hardly be due to the influence of the decalcifying agent. This was also seen in patient #1 of the paired primary tumor and bone metastases samples. Tumor heterogeneity is the most likely option here. Indeed, PR discordance between biopsies and full resection specimens, also largely to be explained by tumor heterogeneity, is relatively common (15%).24
Moreover, immunohistochemistry showed three HER2 3+ scored cases (out of 23), although only one fluorescence in situ hybridization amplified case was observed. Discordance between immunohistochemistry and fluorescence in situ hybridization has been described before but is relatively rare in 3+ samples (9%).25 However, this discordance was seen both in the decalcified samples and the control sample, so no influence of the decalcification process could explain this discrepancy. And no discordance was perceived in the validation cohort, though this group was small.
Furthermore, the interpretation of the Christensen’s buffer with and without microwave- and Formical-4-treated fluorescence in situ hybridization slides was seriously impeded, which was confirmed by the absence of signal in the one HER2 amplified case. This is in line with the findings of Brown et al12 who reported a failure of their fluorescence in situ hybridization protocol when formic acid was used. Future research should address whether adjustments in the standard ISH protocol could overcome these problems.
DNA quality was affected by decalcification as well; all decalcified tissues showed significantly less amplifiable copies than the controls. Christensen’s buffer with microwave- and Formical-4-treated tissue showed the largest drop and the highest fragmentation of DNA, compatible with common knowledge that acidic agents fragment the DNA.12 Singh et al11 compared multiple acidic decalcifying agents on bone biopsies from six patients but found no differences in DNA and RNA integrity (measured by qPCR) between tissue treated with formic acid-based buffers and EDTA. However, time of decalcification was again very short (2 h), which may explain these differences.
As expected, Christensen’s buffer only showed higher DNA quality than Christensen’s buffer with microwave-treated tissue, which can be explained by the acceleration of decalcification by the microwave.26 In immunohistochemistry, however, hardly any differences were seen, although one HER2 2+ case converted to 1+. HER2 fluorescence in situ hybridization results for Christensen’s buffer with and without microwave-treated tissue were equally affected.
In contrast to DNA, no major differences in RNA quality were found between buffers when we compared the RNA Integrity Number. In line with our findings, Singh et al11 also did not find any dissimilarities in RNA quality by qPCR. However, we observed large differences in RNA purity measured by 260/280 ratios. The ratio of the absorbance at 260 and 280 nm (A260/A230 ratios) is commonly used to assess nucleic acid contamination with proteins, organic and phenol,27, 28 although studies of Wilfinger et al29 have revealed that changes in both the pH and ionic strength can have an influence on these ratios. The latter may thus be an alternative explanation for the observed poor outcome of the acidic buffers compared with EDTA and the control.
A first limitation of this study is that we do not have samples of all four conditions (EDTA, Christensen’s buffer with and without microwave and Formical-4) of all patients, because biopsies were taken macroscopically and afterwards tumor was not always present. However, we included sufficient numbers of patients to make subgroups still comparable. Second, we did not subject the biopsies to different decalcifying time periods but overnight decalcification similar to the situation in the daily clinical practice. Nevertheless, differences in outcome between studies are probably caused by different decalcifying periods,11, 22, 23 so it would be worthwhile to further elucidate this aspect. Furthermore, by taking biopsies of the tumor to enable different decalcification conditions, we probably introduced some heterogeneity in samples. We are aware of this side issue of our study design and tried to mark cases suspected of heterogeneity in Supplementary Table S1.
In conclusion, decalcification procedures based on Christensen’s buffer, EDTA and Formical-4 in general seem to have relatively little influence on ERα, PR and HER2 analysis by immunohistochemistry, while EDTA performs best. When regarding exact percentages, we advise to use a 10% threshold for positivity of ERα and PR to prevent patients to be falsely stratified for hormonal therapy. For molecular diagnostics, EDTA seems to be the best choice.
References
Hoefnagel LD, van de Vijver MJ, van Slooten HJ et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res 2010;12:R75.
van Diest PJ, Hoefnagel LD, van der Wall E . Testing for discordance at metastatic relapse of breast cancer matters. J Clin Oncol 2012;30:3031; author reply 3031,2, 3032–3033.
Vignot S, Besse B, Andre F et al. Discrepancies between primary tumor and metastasis: a literature review on clinically established biomarkers. Crit Rev Oncol Hematol 2012;84:301–313.
Hammond ME, Hayes DF, Wolff AC et al. American Society of Clinical Oncology/College of American Pathologists Guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 2010;6:195–197.
Carlson RW, Allred DC, Anderson BO et al. Metastatic breast cancer, version 1.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2012;10:821–829.
Bussolati G, Leonardo E . Technical pitfalls potentially affecting diagnoses in immunohistochemistry. J Clin Pathol 2008;61:1184–1192.
Gruchy JR, Barnes PJ, Dakin Hache KA . CytoLyt(R) fixation and decalcification pretreatments alter antigenicity in normal tissues compared with standard formalin fixation. Appl Immunohistochem Mol Morphol 2015;23:297–302.
Neves Jdos S, Omar NF, Narvaes EA et al. Influence of different decalcifying agents on EGF and EGFR immunostaining. Acta Histochem 2011;113:484–488.
Adegboyega PA, Gokhale S . Effect of decalcification on the immunohistochemical expression of ABH blood group isoantigens. Appl Immunohistochem Mol Morphol 2003;11:194–197.
Reineke T, Jenni B, Abdou MT et al. Ultrasonic decalcification offers new perspectives for rapid FISH, DNA, and RT-PCR analysis in bone marrow trephines. Am J Surg Pathol 2006;30:892–896.
Singh VM, Salunga RC, Huang VJ et al. Analysis of the effect of various decalcification agents on the quantity and quality of nucleic acid (DNA and RNA) recovered from bone biopsies. Ann Diagn Pathol 2013;17:322–326.
Brown RS, Edwards J, Bartlett JW et al. Routine acid decalcification of bone marrow samples can preserve DNA for FISH and CGH studies in metastatic prostate cancer. J Histochem Cytochem 2002;50:113–115.
Wickham CL, Sarsfield P, Joyner MV et al. Formic acid decalcification of bone marrow trephines degrades DNA: alternative use of EDTA allows the amplification and sequencing of relatively long PCR products. Mol Pathol 2000;53:336.
Alers JC, Krijtenburg PJ, Vissers KJ et al. Effect of bone decalcification procedures on DNA in situ hybridization and comparative genomic hybridization. EDTA is highly preferable to a routinely used acid decalcifier. J Histochem Cytochem 1999;47:703–710.
Matthews JB, Mason GI . Influence of decalcifying agents on immunoreactivity of formalin-fixed, paraffin-embedded tissue. Histochem J 1984;16:771–787.
Hagberg KW, Taylor A, Hernandez RK et al. Incidence of bone metastases in breast cancer patients in the united kingdom: results of a multi-database linkage study using the general practice research database. Cancer Epidemiol 2013;37:240–246.
Harries M, Taylor A, Holmberg L et al. Incidence of bone metastases and survival after a diagnosis of bone metastases in breast cancer patients. Cancer Epidemiol 2014;38:427–434.
van Diest PJ . No consent should be needed for using leftover body material for scientific purposes. for. BMJ 2002;325:648–651.
Wolff AC, Hammond ME, Hicks DG et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline update. J Clin Oncol 2013;31:3997–4013.
Sah S, Chen L, Houghton J et al. Functional DNA quantification guides accurate next-generation sequencing mutation detection in formalin-fixed, paraffin-embedded tumor biopsies. Genome Med 2013;5:77.
Van Poznak C, Somerfield MR, Bast RC et al. Use of biomarkers to guide decisions on systemic therapy for women with metastatic breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2015;33:2695–2704.
Darvishian F, Singh B, Krauter S et al. Impact of decalcification on receptor status in breast cancer. Breast J 2011;17:689–691.
Gertych A, Mohan S, Maclary S et al. Effects of tissue decalcification on the quantification of breast cancer biomarkers by digital image analysis. Diagn Pathol 2014;9:213.
Arnedos M, Nerurkar A, Osin P et al. Discordance between core needle biopsy (CNB) and excisional biopsy (EB) for estrogen receptor (ER), progesterone receptor (PgR) and HER2 status in early breast cancer (EBC). Ann Oncol 2009;20:1948–1952.
Bahreini F, Soltanian AR, Mehdipour P . A meta-analysis on concordance between immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) to detect HER2 gene overexpression in breast cancer. Breast Cancer 2015;22:615–625.
Pitol DL, Caetano FH, Lunardi LO . Microwave-induced fast decalcification of rat bone for electron microscopic analysis: an ultrastructural and cytochemical study. Braz Dent J 2007;18:153–157.
Di Bernardo G, Del Gaudio S, Galderisi U et al. Comparative evaluation of different DNA extraction procedures from food samples. Biotechnol Prog 2007;23:297–301.
Johnson MT, Carpenter EJ, Tian Z et al. Evaluating methods for isolating total RNA and predicting the success of sequencing phylogenetically diverse plant transcriptomes. PLoS One 2012;7:e50226.
Wilfinger WW, Mackey K, Chomczynski P . Effect of pH and ionic strength on the spectrophotometric assessment of nucleic acid purity. Biotechniques 1997;22: 474–476, 478–481.
Acknowledgements
We thank Annette Gijsbers-Bruggink for collecting and processing the tissues and our colleagues from the immunopathology laboratory of the University Medical Center Utrecht for performing the routine ERα, PR and HER2 immunohistochemical stainings. This work was supported by Dutch Cancer Society grant UU 2011-5195 and Philips Consumer Lifestyle. The study sponsors had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
This manuscript has neither been published nor is currently under revision elsewhere.
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Schrijver, W., van der Groep, P., Hoefnagel, L. et al. Influence of decalcification procedures on immunohistochemistry and molecular pathology in breast cancer. Mod Pathol 29, 1460–1470 (2016). https://doi.org/10.1038/modpathol.2016.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.116
This article is cited by
-
18F-Fluoroestradiol (FES) PET/CT: review of current practice and future directions
Clinical and Translational Imaging (2022)
-
MDM2 Gene Amplification and Expression of MDM2 and CDK4 are Rare in Ossifying Fibroma of Craniofacial Bones
Head and Neck Pathology (2022)
-
A call to action: molecular pathology in Brazil
Surgical and Experimental Pathology (2021)
-
Effect of decalcification protocols on immunohistochemistry and molecular analyses of bone samples
Modern Pathology (2020)
-
Frequent overexpression of klotho in fusion-negative phosphaturic mesenchymal tumors with tumorigenic implications
Modern Pathology (2020)