Abstract
Epidermal growth factor receptor (EGFR) is frequently overexpressed in triple-negative breast cancer and is emerging as a therapeutic target. EGFR gene copy number alteration and mutation are highly variable and scientists have been challenged to define their prognostic significance in triple-negative breast cancer. We examined EGFR protein expression, EGFR gene copy number alteration and mutation of exon 18 to 21 in 151 cases of triple-negative breast cancer and correlated these findings with clinical outcomes. In addition, intratumoral agreement of EGFR protein overexpression and gene copy number alteration was evaluated. EGFR overexpression was found in 97 of 151 cases (64%) and high EGFR gene copy number was detected in 50 cases (33%), including 3 gene amplification (2%) and 47 high polysomy (31%). Five EGFR mutations were detected in 4 of 151 cases (3%) and included G719A in exon 18 (n=1), V786M in exon 20 (n=1), and L858R in exon 21 (n=3). One case had two mutations (G719A and L858R). High EGFR copy number, but not EGFR mutation, correlated with EGFR protein overexpression. Intratumoral heterogeneity of EGFR protein overexpression and EGFR copy number alteration was not significant. In survival analyses, high EGFR copy number was found to be an independent prognostic factor for poor disease-free survival in patients with triple-negative breast cancer. Our findings showed that EGFR mutation was a rare event, but high EGFR copy number was relatively frequent and correlated with EGFR overexpression in triple-negative breast cancer. Moreover, high EGFR copy number was associated with poor clinical outcome in triple-negative breast cancer, suggesting that evaluation of EGFR copy number may be useful for predicting outcomes in patients with triple-negative breast cancer and for selecting patients for anti-EGFR-targeted therapy.
Similar content being viewed by others
Introduction
Triple-negative breast cancer is a subtype of breast cancer characterized by the absence of expression of estrogen and progesterone receptors and human epidermal growth factor receptor 2 (HER2), accounting for 10–20% of all breast cancers.1, 2, 3 Histopathologically, the majority of triple-negative breast cancers are high-grade invasive carcinomas of no special type, metaplastic carcinomas, and medullary carcinomas.3 Triple-negative breast cancer carries a poorer prognosis than other subtypes of invasive breast cancer.1 It is relatively sensitive to chemotherapy, but early relapse and visceral metastases are common and overall survival remains poor.4, 5 In addition, current systemic therapeutic options for triple-negative breast cancer are limited to conventional cytotoxic chemotherapy, whereas non-triple-negative breast cancer, that is, hormone receptor-positive, or HER2-positive breast cancer may have benefit from anti-hormonal or HER2-targeted therapy. The search for specific molecular targets in triple-negative breast cancer and the development of therapeutics for these targets are ongoing.
Epidermal growth factor receptor (EGFR) alterations have been implicated in the pathogenesis and progression of many malignancies including non-small cell lung cancer6, 7 and glioblastoma.8 EGFR is a well-established treatment target for colorectal cancer, non-small cell lung cancer, and squamous cell carcinoma of the head and neck. In breast cancer, EGFR overexpression has been reported in up to 78% of triple-negative breast cancers,9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 more than in non-triple-negative breast cancers,12, 15 suggesting that EGFR is a potential therapeutic target for triple-negative breast cancer. EGFR tyrosine kinase inhibitors have yielded insignificant response rates in breast cancer,21, 22, 23 possibly due to the lack of patient selection in these studies; they were not restricted to breast cancers with EGFR overexpression or triple-negative breast cancers. Recently, however, EGFR-targeting monoclonal antibody, cetuximab, has improved outcomes in triple-negative breast cancers.24
EGFR gene amplification, one of the mechanisms of EGFR overexpression, is highly variable and found in up to 24% of triple-negative breast cancer.10, 11, 13, 14, 19, 25 EGFR gene mutation, another mechanism of EGFR overexpression, has been reported to be rare,11, 17, 19, 25, 26 although a recent study reported that it was present in 11% of triple-negative breast cancers.16 EGFR immunoreactivity has been presented as an independent indicator of poor prognosis in patients with triple-negative breast cancer.18, 20 However, there have been no reports on the prognostic impact of EGFR copy number alteration or mutation in triple-negative breast cancer. Intratumoral heterogeneity of EGFR protein overexpression and copy number alteration has also not been studied in triple-negative breast cancer, although it may be associated with responsiveness to EGFR-targeted therapy.
The primary goals of this study were to (1) evaluate the rates and prognostic significance of EGFR copy number alteration and mutation in triple-negative breast cancers and (2) assess intratumoral heterogeneity of EGFR protein overexpression and copy number alteration.
Materials and methods
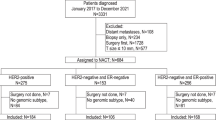
Patients and Tissue Samples
We retrospectively examined the records of the Department of Pathology, Seoul National University Bundang Hospital from 2003 to 2011 and searched for cases of invasive triple-negative breast cancer using immunohistochemical data for standard biomarkers. Estrogen and progesterone receptors were regarded as negative if there were <1% positive tumor nuclei.27 Expression of HER2 was scored according to 2007 American Society of Clinical Oncology/College of American Pathologist guidelines28 and immunohistochemical scores of 0 or 1+ were regarded as negative. For the equivocal (2+) cases, HER2 negative status was confirmed by fluorescence in situ hybridization (FISH). After excluding cases with initial metastases, we selected 151 invasive triple-negative breast cancers from cases of surgically resected primary breast cancer. Baseline patient characteristics are summarized in Table 1. Hematoxylin- and eosin-stained slides were reviewed for each case, and the following histopathologic variables were determined: histologic subtype, T stage, nodal status, Nottingham combined histologic grade, venous invasion, lymphatic invasion, tumor border, and presence or absence of ductal carcinoma in situ component. All cases were independently reviewed by two breast pathologists (SYP and HJL). The study was approved by the institutional review board of Seoul National University Bundang Hospital (IRB No. B-1005/100-303), which waived the requirement for informed consent.
Tissue Microarray Construction
We used tissue microarrays to evaluate EGFR protein expression and EGFR copy number alteration. All slides were reviewed and the most representative tumor section was selected for each case. Tissue microarrays were conducted in two different ways. At first, we constructed large core (4-mm diameter) tissue microarrays (Superbiochips Laboratories, Seoul, Korea) using 42 cases of triple-negative breast cancer to test EGFR protein overexpression and gene copy number. We then constructed tissue microarrays from three different representative tissue cores (2-mm diameter) of 109 triple-negative breast cancers to evaluate the heterogeneity of EGFR protein expression and copy number alteration.
Immunohistochemical Analyses and Scoring
Expression of standard biomarkers including estrogen receptor, progesterone receptor, HER2, p53, and Ki-67 was evaluated in full sections at the time of diagnosis or in tissue microarray sections for missing data during the study. EGFR and cytokeratin 5/6 were evaluated using tissue microarrays. Tissue sections (4 μm) were cut, dried, deparaffinized, and rehydrated following standard procedures. EGFR expression was detected by using EGFR pharmDxTM (Dako). Immunohistochemical staining for the other biomarkers was performed in a BenchMark XT autostainer (Ventana Medical Systems, Tucson, AZ) using an i-View detection kit (Ventana Medical Systems) for estrogen receptor (1:100; clone SP1; Labvision), progesterone receptor (1:70; PgR 636; Dako), HER2 (1:700; polyclonal; Dako), p53 (1:600; D07; Dako), Ki-67 (1:250; MIB-1; Dako), and cytokeratin 5/6 (1:50; clone D5/16 B4; Dako). EGFR expression was scored as follows: 0, no staining or weak membranous staining in <10% of the tumor cells; 1+, weak membranous staining in ≥10% of the tumor cells; 2+, moderate, membranous staining in ≥10% of the tumor cells; 3+, strong membranous staining in ≥10% of the tumor cells. Both complete and incomplete membranous staining was accepted, and 2+ or more staining was considered to represent EGFR overexpression. If the tissue microarray cores yielded a different score, the highest score for the case was used. For cytokeratin 5/6, cases with any positive membranous staining were defined as positive. For p53, cases with 10% or more positive staining were grouped as positive. For the Ki-67 proliferation index, cases with 50% or more positive tumor cells were regarded as having high indices.
FISH Assays for EGFR
To evaluate EGFR copy number alteration, we performed FISH on tissue microarray samples with commercially available locus-specific and chromosome enumeration probes (CEPs) (LSI EGFR SpectrumOrange probe (7p12) and CEP 7 SpectrumGreen probe (7p11.1-q11.1)) (Abbott Molecular, Des Plaines, IL).
FISH was performed as reported for HER2 amplification.29 Briefly, 4-μm deparaffinized tissue microarray sections were incubated in pretreatment solution (Abbott Molecular) at 80 °C for 30 min, then in protease solution (Abbott Molecular) for 25 min at 37 °C. Probes were diluted in tDen-Hyb-2 hybridization buffer (InSitus Biotechnologies, Albuquerque, NM). Co-denaturation of the probes and DNA was achieved by incubating at 75 °C for 5 min in a HYBriteTM (Abbott Molecular) followed by 16-h hybridization at 37 °C. Post-hybridization washes were performed according to supplier protocols. Slides were mounted in 4′,6-diamidino-2-phenylindole/anti-fade and viewed with a fluorescence microscope.
At least 50 non-overlapping tumor cells were evaluated for each tissue microarray core. EGFR copy number was classified into six categories, as described previously30, 31: disomy (≤2 copies in >90% of cells); low trisomy (≤2 copies in ≥40% of cells, three copies in 10–40% of cells, and ≥4 copies in <10% of cells); high trisomy (≤2 copies in ≥40% of cells, three copies in ≥40% of cells, and ≥4 copies in <10% of cells); low polysomy (≥4 copies in 10–40% of cells); high polysomy (≥4 copies in ≥40% of cells); and gene amplification (presence of tight EGFR gene clusters and a ratio of the EGFR gene to chromosome 7 of ≥2, or ≥15 copies of EGFR per cell in ≥10% of cells). For further analysis, the patients were divided into groups according to EGFR copy number as follows: low EGFR gene copy number (disomy, low trisomy, high trisomy, and low polysomy) and high EGFR gene copy number (high polysomy and gene amplification).
Analysis of EGFR Mutation
DNA was extracted from five formalin-fixed, paraffin-embedded tissue sections (10 μm) containing a representative portion of tumor tissue using the QIAamp DNA FFPE Tissue kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol. DNA (50 ng) was amplified in a 20-μl reaction containing 10 μl of 2 × HotStarTaq Master Mix (Qiagen), including PCR Buffer with 3 mM MgCl2, 400 μM each dNTP, and 0.3 μM of each primer (Exon 18F: 5′-CCA TGT CTG GCA CTG CTT T-3′, 18R: 5′-CAG CTT GCA AGG ACT CTG G-3′; Exon 19F: 5′-TGT GGC ACC ATC TCA CAA TTG-3′, 19R: 5′-GGA CCC CCA CAC AGC AA-3′; Exon 20F: 5′-GGT CCA TGT GCC CCT CCT-3′, 20R: 5′-TGG CTC CTT ATC TCC CCT CC-3′; Exon 21F: 5′-CCA TGA TGA TCT GTC CCT CA-3′, 21R: 5′-AAT GCT GGC TGA CCT AAA GC-3′). Amplifications of EGFR exons 18–21 were performed using a 15-min initial denaturation at 95 °C; followed by 35 cycles of 30 s at 94 °C, 30 s at 59 °C, and 30 s at 72 °C, and a 10-min final extension at 72 °C. PCR products were purified with a HiYieldTMGel/PCR DNA Extraction Kit (Real Biotech Corporation, Taiwan).
DNA templates were processed for sequencing with ABI-PRISM BigDye Terminator version 3.1 (Applied Biosystems, Foster, CA) with both forward and reverse sequence-specific primers. Purified PCR products (20 ng) were used in a 10-μl sequencing reaction containing 1 μl BigDye Terminator v3.1 and 0.1 μM PCR primer. Sequencing reactions were performed using 25 cycles of 10 s at 96 °C, 5 s at 50 °C, and 4 min at 60 °C. Sequence data were generated with the ABI PRISM 3730 DNA Analyzer (Applied Biosystems). Sequences were analyzed with Sequencing analysis 5.4. software (Applied Biosystems).
Statistical Analysis
Statistical significance was assessed using Statistical Package, SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL). Concordance of EGFR protein overexpression or EGFR copy number alteration in different tissue microarray cores of a tumor were analyzed by the kappa test. The associations of EGFR protein expression or copy number alteration with clinicopathologic tumor characteristics were analyzed by Fisher’s exact test or the Chi-square test, depending on test conditions. Survival curves were estimated using the Kaplan–Meier product-limit method, and the significance of differences between survival curves was determined using the log-rank test. Covariates that were statistically significant in the univariate analysis were then included in the multivariate analysis using the Cox proportional hazards regression model, and the hazard ratio and its 95% confidence interval were assessed for each factor. P-values <0.05 were considered statistically significant. All reported P-values are two-sided.
Results
EGFR Protein Expression, Copy Number Alteration, and mutation
Of the 151 triple-negative breast cancers, 41 cases (27%) were scored as 3+, 56 (37%) were scored as 2+, 24 (16%) were scored as 1+, and the remaining 30 (20%) were scored as 0 by EGFR immunohistochemistry (IHC) (Figure 1). EGFR FISH revealed gene amplification in 3 (2%) cases, high polysomy in 47 (31%) cases, low polysomy in 69 (46%) cases, high trisomy in 4 (3%) cases, low trisomy in 25 (17%) cases, and disomy in 3 (2%) cases (Figure 1). EGFR mutation was observed in 4 (3%) out of 151 triple-negative breast cancers (Table 2; Figure 2). Three cases had L858R mutation in EGFR exon 21, of which one harbored another mutation, G719A in EGFR exon 18. The remaining case had a V786M mutation in EGFR exon 20, along with EGFR high polysomy and strong (3+) EGFR overexpression.
Missense mutations of EGFR exon 20 and exon 21. (a) Substitution of G to A at mRNA coding nucleotide sequence 2356, resulting in valine to methionine substitution at amino acid codon position 786 (V786M). (b) Substitution of T to G at mRNA coding nucleotide sequence 2573, resulting in leucine to arginine substitution at amino acid 858 (L858R).
The results of EGFR IHC and EGFR FISH were compared in each tissue microarray core from 151 cases. EGFR protein overexpression correlated with EGFR gene amplification and high polysomy (P<0.001; Table 3). The sensitivity and specificity of EGFR overexpression (immunoreactivity of more than 2+) for high EGFR gene copy number were 83% and 48%, respectively. The sensitivity and specificity of EGFR IHC 3+ for EGFR gene amplification were 100% and 78%, respectively.
Intratumoral Comparison of EGFR Protein Expression and EGFR Copy Number
Of the 109 triple-negative breast cancers with three tissue microarray cores, 86 cases with three different cores and 19 cases with two different cores were available for comparison of EGFR protein expression within a tumor; the remainder was excluded owing to the loss of tissue microarray cores. For EGFR FISH, 94 cases with three tissue microarray cores and 9 cases with two tissue microarray cores were available; the remainder was excluded due to FISH failure or core detachment. Intratumoral agreement of EGFR protein overexpression or copy number alteration was analyzed in these cases. Overall, the concordance rate of intratumoral EGFR expression (0, 1+ vs 2+, 3+) was 90% (94/105) with a mean kappa value of 0.836 (P<0.001) (Table 4). The concordance rate of intratumoral EGFR copy number alteration (low gene copy number vs high gene copy number) was 86% (89/103) with a mean kappa value of 0.793 (P<0.001) (Table 5). Specifically, the three cases with EGFR gene amplification showed homogenous EGFR gene amplification and strong (3+) EGFR protein expression in all tissue microarray cores. There was no clinicopathologic difference between cases with intratumoral heterogeneity and those with homogeneity for EGFR protein expression or EGFR copy number alteration.
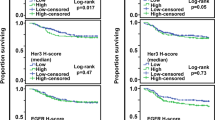
Clinicopathologic Features According to EGFR Protein Expression, Copy Number, and Mutation
We explored the relationship of EGFR protein expression, copy number gain, and mutation with the clinicopathologic variables of triple-negative breast cancer (Table 6). EGFR overexpression (2+ or 3+) was significantly associated with lower stage (P=0.018). However, EGFR copy number and mutation did not correlate with any clinicopathologic variable. We also investigated the prognostic utility of EGFR alteration. At the time of analysis, the median follow-up was 4.9 years (range, 0.1–9.0 years). There were 7 (5%) loco-regional recurrences, 12 (8%) distant metastases, and 1 (1%) cancer-related death as the first event. In Kaplan–Meier survival analyses, the patients with high EGFR copy number had shorter disease-free survival than those without it (P=0.027; Figure 3; Table 7). However, EGFR overexpression and EGFR mutation were not associated with disease-free survival (Table 7). In multivariate analysis including stage and EGFR copy number alteration, high stage (stage I and II vs stage III; hazard ratio, 2.815; 95% confidence interval, 1.022–7.751; P=0.045) and high EGFR gene copy number (low gene copy number vs high gene copy number; hazard ratio, 2.569; 95% confidence interval, 1.063–6.208; P=0.036) remained as independent prognostic indicators of poor disease-free survival.
Discussion
EGFR is frequently overexpressed in triple-negative breast cancer and clinical trials of EGFR-targeting agents are underway in patients with triple-negative breast cancer. However, the rate of EGFR copy number alteration and mutation, and the underlying mechanisms of EGFR overexpression are unclear, and their prognostic significance is poorly defined in triple-negative breast cancer. We evaluated the rates of EGFR gene alteration, their clinical implications in prognosis, and the intratumoral agreement of EGFR protein overexpression and gene copy number in triple-negative breast cancer.
EGFR gene amplification and high polysomy were reported in up to 24% and 27% of triple-negative breast cancer, respectively (Table 8).10, 11, 13, 14, 19, 25 However, the frequency of EGFR gene amplification is quite variable, even though most studies used the same, University of Colorado Cancer Center criteria.30, 31 We also assessed EGFR amplification by the University of Colorado Cancer Center criteria and found that EGFR amplification was quite rare, being present in only 2% of cases, which is consistent with some previous studies.10, 19, 25 However, EGFR high polysomy was found in 31% of cases, which is relatively higher than in previous studies. This result may be related to the heterogeneity of high polysomy in some cases, which will be discussed later. The frequency of EGFR gene copy number gain in the previous studies appears to be greater in a subset of triple-negative breast cancers, ie, metaplastic carcinoma and triple-negative breast cancer with basal-like feature. In this study, the rate of high EGFR gene copy tended to be higher in metaplastic carcinoma than the other tumors (58% vs 30%, P=0.063, data not shown); however, there were no significant differences in EGFR copy number gain between basal-like and non-basal-like, triple-negative breast cancers.
The correlation between EGFR protein expression by IHC and EGFR gene copy number gain is controversial. Several groups that used in situ hybridization technique reported significant correlations between EGFR protein overexpression and high gene copy in triple-negative breast cancer.10, 13, 14, 19 However, Martin et al11 and Toyama et al17 showed no correlation between EGFR immunoexpression and increased EGFR gene copy number. In this study, EGFR overexpression was generally correlated with high EGFR copy number. However, about half of the cases with low EGFR gene copy number showed EGFR overexpression. Of the 202 tumor cores showing EGFR overexpression, only 76 (38%) revealed high EGFR copy number. Even if EGFR overexpression was defined as IHC 3+, only 44 (55%) of 80 cores with EGFR IHC 3+ showed EGFR high polysomy or gene amplification. That is, the specificity and positive predictive value of EGFR overexpression for high EGFR gene copy number were relatively low. These findings are contrary to the close correlation between HER2 overexpression and HER2 amplification; HER2 overexpression is mostly attributable to HER2 gene amplification.28, 32 Moreover, eight cases (11 tumor cores) with no EGFR immunoreactivity had high EGFR polysomy. Therefore, EGFR IHC alone has limited value in defining the group of triple-negative breast cancer patients with increased EGFR gene copy number.
Most studies encompassing Caucasian, European, and Japanese patients report a lack of EGFR mutation in triple-negative breast cancer (Table 8).11, 17, 19, 25, 26 However, Teng et al reported the presence of EGFR mutation, specifically exon 19 deletions and exon 21 missense (L858R) mutations, in 11% (8/70) of triple-negative breast cancer samples from predominantly Chinese patients.16 In this study, EGFR mutation was found in 3% (4/151) of triple-negative breast cancer samples from Korean patients. As suggested by Lamy and Jacot,33 wide variations in the rate of EGFR mutation in different populations may reflect geographic or ethnic differences in the presence of EGFR mutation. However, most studies encompass small series; well-organized, large-scale studies are needed to determine the origin of EGFR mutation variation in triple-negative breast cancer. Of the four cases with EGFR mutation, three carried a missense mutation of exon 21 (L858R), one of which with a coexisting missense mutation of exon 18 (G719A), and remaining case carried a missense mutation of exon 20 (V786M). Missense mutations such as G719A/S and L858R and exon 19 deletions are well-known predictors of sensitivity to tyrosine kinase inhibitors in non-small cell lung cancer,34 so the presence of L858R and G719A mutations in this study population suggests gefitinib or erotinib therapy may be beneficial in these selected triple-negative breast cancer patients. In our study, there was disagreement between EGFR immunostaining and the presence of EGFR mutation, similar to the report of Teng and colleagues,16 suggesting that positivity in EGFR IHC cannot predict EGFR mutation in triple-negative breast cancer.
In this study, high EGFR copy number was significantly associated with poor disease-free survival and acted as an independent poor prognostic factor. Although EGFR overexpression has been presented as a poor prognostic indicator in triple-negative breast cancer,18, 20 high EGFR copy number has no reported prognostic impact in patients with triple-negative breast cancer. The mechanism by which high EGFR copy number contributes to the progression of triple-negative breast cancer is unclear. However, EGFR copy number gain might be one of the accumulating genetic alterations during tumor progression and EGFR activation induced by EGFR copy number gain may contribute to tumor aggressiveness in triple-negative breast cancer. It was suggested that EGFR activation drives migration and invasion of tumor cells through epithelial–mesenchymal transition and alters chemosensitivity by rewiring the apoptotic signaling network.35 However, the utility of high EGFR copy number as a predictive biomarker for EGFR-targeted therapy and as a prognostic factor for triple-negative breast cancer should be validated in large studies.
EGFR protein expression in triple-negative breast cancer is quite variable, ranging from 13 to 78% (Table 8).9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 In this study, we used EGFR pharmDxTM (Dako), which is an approved anti-EGFR antibody for identification of colorectal cancer patients eligible for treatment with cetuximab or panitumumab. Moderate to strong membranous staining in >10% of tumor cells was regarded as EGFR overexpression and was found in 97 (64%) of 151 triple-negative breast cancer cases, comparable to previous studies. However, in contrast to previous studies suggesting prognostic implications of EGFR overexpression in triple-negative breast cancer,18, 20 we did not observe a survival difference associated with EGFR protein expression. This conflicting result may be attributable to differences in the antibodies used and different definitions of EGFR overexpression.
We evaluated intratumoral concordance of EGFR protein expression and gene copy number alteration in triple-negative breast cancer using different tissue microarray cores within a tumor. EGFR protein overexpression and EGFR copy number alteration were highly concordant in different tumor areas within each triple-negative breast cancer. All tumors with EGFR gene amplification demonstrated homogeneous EGFR protein overexpression within a tumor, implying triple-negative breast cancer patients with EGFR gene amplification would be excellent candidates for EGFR-targeted therapy. On the other hand, 12 of 30 cases with high polysomy showed discordant copy number results in at least one core of three tumor cores. It appears that EGFR high polysomy is relatively heterogeneous within a tumor, possibly due to the chromosomal instability of triple-negative breast cancer.
In summary, EGFR mutation was a rare event in triple-negative breast cancers, but high EGFR copy number including EGFR amplification and high polysomy was relatively frequent and correlated with EGFR overexpression. Intratumoral heterogeneity of EGFR protein overexpression and EGFR copy number alteration was not significant. More importantly, high EGFR copy number was associated with poor clinical outcome of the patients with triple-negative breast cancer. Our results suggest that evaluation of EGFR copy number can be useful for predicting outcomes in patients with triple-negative breast cancer and selecting patients for anti-EGFR-targeted therapy.
References
Bauer KR, Brown M, Cress RD et al. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer 2007;109:1721–1728.
Dent R, Trudeau M, Pritchard KI et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 2007;13:4429–4434.
Reis-Filho JS, Tutt AN . Triple negative tumours: a critical review. Histopathology 2008;52:108–118.
Haffty BG, Yang Q, Reiss M et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol 2006;24:5652–5657.
Liedtke C, Mazouni C, Hess KR et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 2008;26:1275–1281.
Prudkin L, Wistuba II . Epidermal growth factor receptor abnormalities in lung cancer. Pathogenetic and clinical implications. Ann Diagn Pathol 2006;10:306–315.
Scagliotti GV, Selvaggi G, Novello S et al. The biology of epidermal growth factor receptor in lung cancer. Clin Cancer Res 2004;10:4227s–4232s.
Fuller GN, Bigner SH . Amplified cellular oncogenes in neoplasms of the human central nervous system. Mutat Res 1992;276:299–306.
Choi J, Jung WH, Koo JS . Clinicopathologic features of molecular subtypes of triple negative breast cancer based on immunohistochemical markers. Histol Histopathol 2012;27:1481–1493.
Gumuskaya B, Alper M, Hucumenoglu S et al. EGFR expression and gene copy number in triple-negative breast carcinoma. Cancer Genet Cytogenet 2010;203:222–229.
Martin V, Botta F, Zanellato E et al. Molecular characterization of EGFR and EGFR-downstream pathways in triple negative breast carcinomas with basal like features. Histol Histopathol 2012;27:785–792.
Rakha EA, El-Sayed ME, Green AR et al. Prognostic markers in triple-negative breast cancer. Cancer 2007;109:25–32.
Reis-Filho JS, Pinheiro C, Lambros MB et al. EGFR amplification and lack of activating mutations in metaplastic breast carcinomas. J Pathol 2006;209:445–453.
Shao MM, Zhang F, Meng G et al. Epidermal growth factor receptor gene amplification and protein overexpression in basal-like carcinoma of the breast. Histopathology 2011;59:264–273.
Tan DS, Marchio C, Jones RL et al. Triple negative breast cancer: molecular profiling and prognostic impact in adjuvant anthracycline-treated patients. Breast Cancer Res Treat 2008;111:27–44.
Teng YH, Tan WJ, Thike AA et al. Mutations in the epidermal growth factor receptor (EGFR) gene in triple negative breast cancer: possible implications for targeted therapy. Breast Cancer Res 2011;13:R35.
Toyama T, Yamashita H, Kondo N et al. Frequently increased epidermal growth factor receptor (EGFR) copy numbers and decreased BRCA1 mRNA expression in Japanese triple-negative breast cancers. BMC Cancer 2008;8:309.
Viale G, Rotmensz N, Maisonneuve P et al. Invasive ductal carcinoma of the breast with the ‘triple-negative’ phenotype: prognostic implications of EGFR immunoreactivity. Breast Cancer Res Treat 2009;116:317–328.
Nakajima H, Ishikawa Y, Furuya M et al. Protein expression, gene amplification, and mutational analysis of EGFR in triple-negative breast cancer. Breast Cancer 2014;21:66–74.
Liu D, He J, Yuan Z et al. EGFR expression correlates with decreased disease-free survival in triple-negative breast cancer: a retrospective analysis based on a tissue microarray. Med Oncol 2012;29:401–405.
von Minckwitz G, Jonat W, Fasching P et al. A multicentre phase II study on gefitinib in taxane- and anthracycline-pretreated metastatic breast cancer. Breast Cancer Res Treat 2005;89:165–172.
Baselga J, Albanell J, Ruiz A et al. Phase II and tumor pharmacodynamic study of gefitinib in patients with advanced breast cancer. J Clin Oncol 2005;23:5323–5333.
Dickler MN, Cobleigh MA, Miller KD et al. Efficacy and safety of erlotinib in patients with locally advanced or metastatic breast cancer. Breast Cancer Res Treat 2009;115:115–121.
Baselga J, Gomez P, Greil R et al. Randomized Phase II study of the anti-epidermal growth factor receptor monoclonal antibody Cetuximab with Cisplatin versus Cisplatin alone in patients with metastatic triple-negative breast cancer. J Clin Oncol 2013;31:2586–2592.
Grob TJ, Heilenkotter U, Geist S et al. Rare oncogenic mutations of predictive markers for targeted therapy in triple-negative breast cancer. Breast Cancer Res Treat 2012;134:561–567.
Jacot W, Lopez-Crapez E, Thezenas S et al. Lack of EGFR-activating mutations in European patients with triple-negative breast cancer could emphasise geographic and ethnic variations in breast cancer mutation profiles. Breast Cancer Res 2011;13:R133.
Hammond ME, Hayes DF, Dowsett M et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 2010;28:2784–2795.
Wolff AC, Hammond ME, Schwartz JN et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 2007;25:118–145.
Hyun CL, Lee HE, Kim KS et al. The effect of chromosome 17 polysomy on HER-2/neu status in breast cancer. J Clin Pathol 2008;61:317–321.
Cappuzzo F, Hirsch FR, Rossi E et al. Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst 2005;97:643–655.
Hirsch FR, Herbst RS, Olsen C et al. Increased EGFR gene copy number detected by fluorescent in situ hybridization predicts outcome in non-small-cell lung cancer patients treated with cetuximab and chemotherapy. J Clin Oncol 2008;26:3351–3357.
Lebeau A, Deimling D, Kaltz C et al. Her-2/neu analysis in archival tissue samples of human breast cancer: comparison of immunohistochemistry and fluorescence in situ hybridization. J Clin Oncol 2001;19:354–363.
Lamy PJ, Jacot W . Worldwide variations in EGFR somatic mutations: a challenge for personalized medicine. Diagn Pathol 2012;7:13.
Lynch TJ, Bell DW, Sordella R et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004;350:2129–2139.
Masuda H, Zhang D, Bartholomeusz C et al. Role of epidermal growth factor receptor in breast cancer. Breast Cancer Res Treat 2012;136:331–345.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (Grant No. 2012R1A1B4000557) and by a grant from Seoul National University Bundang Hospital, Republic of Korea (03-2012-007).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, H., Jang, M., Kim, E. et al. High EGFR gene copy number predicts poor outcome in triple-negative breast cancer. Mod Pathol 27, 1212–1222 (2014). https://doi.org/10.1038/modpathol.2013.251
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.251
Keywords
This article is cited by
-
Novel exosomal circEGFR facilitates triple negative breast cancer autophagy via promoting TFEB nuclear trafficking and modulating miR-224-5p/ATG13/ULK1 feedback loop
Oncogene (2024)
-
EGFR as a potent CAR T target in triple negative breast cancer brain metastases
Breast Cancer Research and Treatment (2023)
-
Structural characterization of a cytosine-rich potential quadruplex forming sequence in the EGFR promoter
Journal of Thermal Analysis and Calorimetry (2023)
-
Ketoprofen suppresses triple negative breast cancer cell growth by inducing apoptosis and inhibiting autophagy
Molecular Biology Reports (2023)
-
In vitro anti-cancer effects of gefitinib via EGF receptor-targeted delivery on triple-negative breast cancer cells
Macromolecular Research (2023)