Abstract
This series of 113 sequential biopsies of full facial transplants provides findings of potential translational significance as well as biological insights that could prompt reexamination of conventional paradigms of effector pathways in skin allograft rejection. Serial biopsies before, during, and after rejection episodes were evaluated for clinicopathological assessment that in selected cases included specific biomarkers for donor-versus-recipient T cells. Histologic evidence of rejection included lymphocyte-associated injury to epidermal rete ridges, follicular infundibula, and dermal microvessels. Surprisingly, during active rejection, immune cells spatially associated with target cell injury consisted abundantly or predominantly of lymphocytes of donor origin with an immunophenotype typical of the resident memory T-cell subset. Current dogma assumes that skin allograft rejection is mediated by recipient T cells that attack epidermal targets, and the association of donor T cells with sites of target cell injury raises questions regarding the potential complexity of immune cell interactions in the rejection process. A more histopathologically refined and immune-based biomarker approach to assessment of rejection of facial transplants is now indicated.
Similar content being viewed by others
Main
Recent reports emphasizing the critical therapeutic importance of accurate diagnosis of transplant rejection1 have stressed the imminent need for more precise clinicopathologic criteria and complementary application of relevant biomarkers.2 The first systematic studies of any form of human allograft rejection were reported by Gibson and Medawar3 in their classic description of skin rejection involving wartime aviators.4 Early clues regarding the immunologic basis of skin graft rejection came from studies by Dvorak et al5 and Bhan et al6 that implicated both CD4+ and CD8+ T cells. These T-cell populations were presumed to be of recipient origin and considered to be primary effectors of epidermal and dermal microvascular target cell injury. With the recent advent of full-facial transplantation,7 detailed and sequential histopathologic surveillance for rejection in a manner seldom feasible for conventional skin allografts has become a necessity. However, existing schemas8 for histologic recognition and grading of rejection in vascular composite allotransplantation are based primarily on allografts that may express relevant structural and immunological differences from facial tissues, eg, extremities (hand) and abdominal wall transplantations. Moreover, precise understanding of immune cell phenotypes that participate in rejection phenomena in this emerging frontier remains incomplete. Here, we report a detailed sequential clinicopathological study in five full facial transplant recipients who were successfully treated for rejection. These studies are complemented by biomarker immunophenotyping of three patients who experienced most significant and specific histopathological changes. Serial biopsies in our study revealed lymphocyte-mediated injury of microvessels, stem cell-rich epidermal and follicular microcompartments, and associated target cell apoptosis in anagen follicles that persists after therapy-induced remission. Importantly, T cells with immunophenotypes consistent with donor cells resident to the facial transplants are identified as major constituents of the rejection response, a finding with potentially important diagnostic and therapeutic implications.
Materials and methods
Patients
A total of five patients receiving facial transplants at our institution between 2009 and 2013 were evaluated with serial skin biopsies (Table 1 and Figure 1). Pre-transplant protocols and standard of care measures to maintain immunosuppression and prevent rejection were employed, as previously described.7, 9 Biopsies were obtained weekly during the first month after the procedure, and then at 3, 6, 9, 12, 18, and 24 months post-operatively or when clinically indicated (Figure 1). One hundred and thirteen biopsies were evaluated for all five patients with clinical rejection, with a range of twelve to twenty-five biopsies per patient. Although some degree of relatively stable edema and redness was integral to the post-transplant setting, rejection was suspected when the following clinical signs became accentuated: erythema, swelling, induration, or mucosal ulceration. The clinical rejection was determined by physician global assessment for purposes of semi-quantitative comparison: 0=no rejection; 1=equivocal rejection; and 2=rejection strongly suspected (Figure 1). Histopathological assessment of rejection was rendered using the BANFF system for grading skin-containing composite tissue allografts8 as follows: grade 0=‘no or rare inflammatory infiltrates’; grade I (mild)=‘mild perivascular infiltration’ (with no epidermal involvement); grade II (moderate)=‘moderate-to-severe perivascular inflammation with or without mild epidermal and/or adnexal involvement’; grade III (severe)=‘dense inflammation and epidermal involvement with epithelial apoptosis, dyskeratosis, and/or keratinolysis’; grade IV (necrotizing acute rejection)=‘frank necrosis of epidermis or other skin structures’. All of the five transplanted patients had clinical and histopathological evidence of rejection; of these, three (patients 2, 3, and 5) exhibited confirmatory evidence of effector cell-mediated apoptosis of target cells within grafts (Banff grade III), and these were further evaluated by detailed biomarker profiling. As assessed by pre-transplant panel-reactive antibody testing, a screening test for reactivity against human leukocyte antigen (HLA) epitopes expressed in the general population, patients 2 and 5 were sensitized against >70% of the general population. Patient 5 was furthermore positive for specific HLA epitopes express by the selected donor, as determined by donor-specific antibody testing. All patients had negative CDC T-cell cross-matches before transplantation. Rejection episodes in two patients (patients 2 and 3) were preceded by self-initiated decrease in immunosuppression. Serial biopsies obtained during rejection episodes were evaluated by conventional hematoxylin and eosin histopathology as well as by single and dual biomarker labeling approaches. The phenotypes of rejection were compared among patients as well as to pre-rejection specimens and samples taken after therapy-induced remission. Therapy consisted of a pulse of steroids followed by increase in maintenance immunosuppression.7 Two instances of refractory cellular rejection were treated with steroids, and steroid resistance with thymoglobulin (rabbit ATG, Genzyme).
Serum levels of immunosuppressant tacrolimus, Banff scores, and clinical rejection scores of three full facial transplant patients. Immunosuppressant tacrolimus levels (ng/ml; black circle) of patients 2, 3, and 5 are shown in top panel. Banff scores (solid lines) by histopathological diagnosis and the clinical rejection scores (dotted lines) are shown in bottom panel. x-Axis indicates post-transplant days.
Immunohistochemistry and Immunofluorescence
All specimens were evaluated by conventional histopathology, and then further selected for biomarker evaluation. Immunohistochemistry was performed with pressure cooker heat-induced epitope retrieval on 5-μm-thick sections prepared from formalin-fixed, paraffin-embedded tissues. Antibodies used included those directed against: T-cell epitopes CD3 (Abcam, Cambridge, MA, USA), CD4 (Invitrogen, Camarallo, CA, USA), CD8 (Abcam), FoxP3 for regulatory T cells (BioLegend, San Diego, CA, USA);10, 11 and skin homing molecule cutaneous lymphocyte-associated antigen (CLA) (BioLegend), CD69 (Novus Biologicals, Littleton, CO, USA), and CD103 (Abcam) for resident memory T (Trm) cells.12, 13, 14 In addition to detection of biomarker antibodies by use of chromogen vector NovaRed peroxidase substrate (Vector laboratory, Burlingame, CA, USA), selected samples were evaluated by a dual labeling approach by combining NovaRed with a blue chromogen vector Blue AP substrate (Vector laboratory). Positive and negative tissue controls and isotype-specific irrelevant antibody controls were used to ensure specificity. To discriminate between donor and recipient T cells, antibodies were obtained to HLA mismatch antigens between donor and recipient, as determined before transplantation. For two patients, anti-Bw4 antibody (Biorbyt, Cambridgeshire, UK) was used to detect HLA-B allele antigen Bw4 expressed by donors, and anti-B7 antibody (Abcam) was used to detect HLA-B allele antigen B7 expressed by recipients. Patient 3 expressed HLA-B antigen Bw4 and donor cells were defined as Bw4-negative T cells, as assessed by dual labeling. The HLA antigens evaluated are of established sensitivity in detecting lymphocytes, is opposed to non-lymphoid skin cells that show variable expression particularly in formalin-fixed, paraffin-embedded tissues. Specificity was established in control tissues of known HLA type (Supplementary Figure 1).
Dual-labeling immunoflourescence was performed to complement immunohistochemistry as a means of two-channel identification of epitopes co-expressed in similar or overlapping sub-cellular locations (eg, where both are expressed by the cell membrane). Briefly, 5-μm-thick paraffin sections were incubated with two primary antibodies generated in mouse and rabbit (detailed above) that recognize the target epitopes at 4 °C overnight and then incubated with Alexa Fluor 594-conjugated anti-mouse IgG and Alexa Fluor 488-conjugated anti-rabbit IgG (Invitrogen) at room temperature for 1 h. The sections were cover slipped with ProLong Gold anti-fade with DAPI (Invitrogen). Sections were analyzed with a BX51/BX52 microscope (Olympus America, Melville, NY, USA), and images were captured using the CytoVision 3·6 software (Applied Imaging, San Jose, CA, USA). Single label immunofluorescence was also performed using isotype-specific irrelevant primary antibodies and with switching of the secondary antibodies to ensure specificity and exclude cross-reactivity. FoxP3/CD8 ratios were generated via cell counting using an ocular grid micrometer over at least five high-power fields, and differences were statistically assessed using the one-way ANOVA analysis.
Results
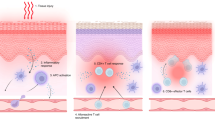
Before clinical rejection episodes, all patients exhibited minimal perivascular and perifollicular lymphoid infiltrates in the absence of lymphoid migration into epithelium and evidence of epithelial apoptosis, and therefore were defined as grade 0 or I (of IV) based on Banff criteria.8 Rejection in all patients coincided with development of clinical signs and shared the following histopathologic features: perivascular lymphoid infiltrates with evidence of endothelial injury that included cell sloughing into vessel lumens (‘lymphocytic vasculitis’); lymphocyte migration into the epidermis and into pilosebaceous structures; and epithelial apoptosis spatially associated with infiltrating lymphocytes (this latter feature qualifying for Banff grade III (Figure 2 and Supplementary Figure 2)). The lymphocytic vasculitis documented during clinical rejection episodes was distinct from neutrophil-mediated (‘leukocytoclastic’) vasculitis that typically shows fibrinoid necrosis of vessel walls associated with degenerating and fragmented neutrophils. The presence of pre-transplant positivity for panel-reactive antibody or donor-specific antibodies did not correlate with the time of onset of rejection post transplant or with the nature of the histopathologic findings, and did not coincide with thrombotic- or neutrophil-associated necrotizing vasculitis. Evidence of early epidermal involvement consisted of lymphocyte aggregation and infiltration at the tips of epithelial stem cell-rich rete ridges (Figure 2 and Supplementary Figure 2) and the bulge regions of pilosebaceous units (Figure 2a). Biomarkers directed against donor and recipient histocompatability antigens were remarkable in that the majority (>90%) of lymphoid cells infiltrating the epidermis and pilosebaceous epithelium were donor derived in all three patients so studied (Bw4 positive and B7 negative in patients 2 and 5, and Bw4 negative in patient 3; Figures 2 and 3). Donor T cells were the predominant phenotype to be spatially associated with sites of intra-epidermal and intra-follicular target cell injury, where they often surrounded epithelial cells in a satellitosis pattern typical of cytotoxic cutaneous immune reactions, such as acute graft-versus-host disease; Figure 2). There was an approximately 50:50 admixture of donor/ recipient cells surrounding damaged vessels and within the surrounding dermis, although donor cells were consistently more intimately associated with luminal endothelium undergoing degenerative alterations (Figure 2). Donor cells in the epidermal compartment proved by dual labeling to be exclusively dendritic-appearing CD8+ T cells, with an admixture of donor and recipient CD8+ and CD4+ T cells in pilosebaceous and perivascular compartments (Figures 2 and 3). Although T cells were strongly reactive for either donor or host histocompatibility antigens, the background staining of non-immune skin cells was variable, as has been previously described.15, 16, 17, 18 Moreover, this trend was further influenced by use of formalin-fixed, paraffin-embedded tissue and the highly specific antibodies to selected HLA-B epitopes.19 However, rigorous controls for specificity were possible by correlative identification of antibody staining with appropriate donor and recipient skin cell subpopulations (Supplementary Figure 1).
Histopathological and histocompatibility antigen profiles in facial allograft rejection (patient 5). The panels characterize lymphocytic vasculitis, epidermal rete ridge targeting, and follicular targeting, respectively. By conventional histology (top row, H&E), lymphocytes surround and infiltrate vessel walls associated with endothelial cell sloughing (arrow), and resulting in lymphocytic vasculitis. Early epidermal involvement is seen in the form of rete targeting where lymphocytes accumulate at the tips of the rete ridges (arrows) in association with early epithelial apoptosis (inset). Follicular targeting is characterized by follicular (F) infiltration by lymphocytes in association with epithelial apoptosis (arrow). Corresponding immunohistochemical panels show donor (d) histocompatibility marker (Bw4, middle row) and recipient (r) histocompatibility marker (B7, bottom row). Note prominent donor component associated with lymphocytic vasculitis, and dominant donor component associated with rete ridge and follicular targeting (*=rete tip; dashed line=basement membrane; c=follicular canal).
(a) Spatial associations of lymphoid cells with target cell injury in facial allografts (patient 5). Lymphocytes at tips of epidermal rete ridges surrounded target cells (arrows, top row H&E staining) to form ‘satellitosis’. Donor (Bw4) and CD8+ T cells precisely corresponded to these patterns of satellitosis (bottom row). Sites of follicular targeting in the bulge region, as well as microvascular targeting, also correlated with the presence of donor T cells that often were located within vessel lumens (intraluminal donor T cell in apposition to degenerating endothelial cells within square; intrafollicular apoptotic target cell encircled). Dotted line=dermal–epidermal and dermal–follicular junctions). (b) Dual labeling for donor/recipient histocompatibility antigens and T-cell phenotype (color of font=fluorochrome used; patient 5). The majority of cells in epidermal infiltrates (top and middle rows, far left) and follicular infiltrates (top and middle rows, middle) were CD3-positive (green) T cells of donor origin (Bw4, red; co-expression=yellow–orange). Cells expressing resident memory T-cell markers (CD69, green) co-expressed donor (Bw4, red) but not recipient (B7) antigen markers (top and middle rows, far right) consistent with their origin in the facial allograft. Donor resident memory T cells (CD69- or CD103-positive cells, red) were predominantly CD8 positive (green) in the epidermis and CD4 positive (green) in hair follicles (bottom row). Color mixing of red and green epitopes=yellow or yellow–orange; blue=DAPI nuclear stain.
In view of the recent discovery of abundant T cells indigenous to human skin and subcutis that express a Trm-cell phenotype,20 we next sought to determine whether donor T cells present in facial allograft rejection expressed the Trm markers CD69 and CD103, as well as the skin homing receptor, CLA.12, 13, 14 Unlike central memory T cells that circulate in the peripheral blood, donor T cells in rejecting allografts were predominantly (>90%) of the Trm phenotype (CD69+, CD103+, CLA+). The majority of intraepidermal Trm cells also expressed CD8, a recently defined subclass of dendritic Trm that physiologically patrol the epidermal microenvironment for foreign antigens (Figure 3).20 The ability to co-localize the donor MHC with the Trm phenotype (indicating a resident T memory phenotype) provided additional confirmation of donor origin (Figure 3). It also has been recognized recently that skin immunity regulated by Trm may be suppressed by the influx of recipient circulating FoxP3+ regulatory T cells that express skin homing receptors.10 Therefore, we next evaluated FoxP3:CD8 ratios before, during, and after rejection (Figure 4). Although significance was not achieved in all patients, the individual experiencing most pronounced transitions from baseline to severe rejection to remission (patient 5) showed a statistically significant lesional decrease of the FoxP3:CD8 ratio during rejection that reverted to pre-rejection values following therapy (P<0.01; Figure 4). FoxP3-positive T cells, as expected, predominately expressed recipient histocompatability markers (Figure 4).
Histopathological and immunophenotypic findings of pre-rejection, active rejection, and remission after immunosuppressive therapy. Conventional hematoxylin and eosin (H&E) histopathology before and after resolution of rejection (top row) reveals only scattered lymphocytes in the dermis without evidence of epithelial infiltration; in contrast, rejection is characterized by the accumulation of lymphocytes around vessels (lower right of top middle panel) and epidermal infiltration (follicular infiltration not shown). Persistent follicular injury characterized by two follicular epithelial apoptotic cells is highlighted by a circle in the post-rejection biopsy (inset). By immunofluorescence (middle row), epidermal injury during rejection is associated with CD8-positive donor T cells (CD8=green, Bw4=red, co-expression=yellow–orange), whereas pre- and post-rejection samples show only rare intraepithelial donor CD8-positive cells (blue=DAPI). Rejection was also associated with a statistically significant decline in the FoxP3/CD8 ratio (patient 5), as indicated qualitatively by dual labeling immunohistochemistry (bottom row; CD8=brown, FoxP3=blue) and quantitatively via cell counting (graph). Dual labeling immunohistochemistry (HLA-B7=brown and FoxP3=blue) indicates that the FoxP3 positive (blue nuclear stain) are recipient (HLA-7 positive) cells (brown membranous stain).
All five patients showed similar alterations during rejection with respect to epithelial and vascular targeting; the three patients evaluated immunohistochemically all demonstrated similar distribution and relative numbers of donor-versus-recipient T cells in lesions as well as T-cell phenotype with regard to CD8/CD4 ratios and Trm-like phenotype (Figure 2 and Supplementary Figure 2). Of note, apoptosis in anagen follicles persisted after therapy-induced reversal of T-cell infiltration, epidermal and vascular injury, and clinical signs of rejection (Supplementary Figure 2), such that use of the apoptosis criterion in the setting of anagen follicular involvement for grade III rejection according to the Banff schema8 produced false-positive interpretation of disease activity.
Discussion
As the first partial face transplantation was successfully completed in 2005, over 25 facial allografts have been performed globally. This innovation has already proven to be a valuable and feasible reconstructive procedure for social and functional rehabilitation in severely disfigured patients.21 However, clinical assessment, histopathological diagnosis, and immunological mechanisms of facial composite allograft rejection remain incompletely studied, albeit being critical to further refinement of this new treatment option. Although a number of important studies have begun to address the issue of biomarkers and related immunopathology in vascular composite allotransplantation22, 23, 24, 25, 26, 27, 28, 29 (particularly in hand transplantation), our study represents a detailed and sequential histopathologic and immunophenotypic assessment of full facial transplant rejection. Facial allografts represent a unique setting where rejection can be evaluated for cutaneous biomarker expression in multiple and sequential biopsies not required in routine skin allograft transplantation. Clinical manifestations of facial allograft rejection including skin redness, swelling, induration, or mucosal ulcerations may be difficult to assess because of changes inherent to the surgical procedure itself.30 Moreover, ancillary markers for dysfunction of the transplanted tissue such as systemic monitoring of parameters for renal function are lacking in skin transplantation. Thus, serial histopathologic and biomarker assessment of transplanted tissue is of critical importance in rendering a timely diagnosis of early rejection as well as to guide proper immunotherapeutic intervention and adjustment over time.30 In this regard, the pathology community represents a pivotal component of this new and exciting technology.
Currently, the Banff 2007 skin-containing composite tissue allograft working classification is largely accepted and used for grading of facial transplantation.8 The Banff working classification is also used for diagnosis and grading of renal allograft pathology, where recently cited limitations include lack of formal incorporation of morphology, molecular, and genomic approaches.31 For skin and soft tissue vascular composite allotransplantation, the Banff classification focuses primarily on extremity and abdominal allografts that are not entirely relevant to the microanatomical, immunologic, and dermatitic milieu of facial skin and soft tissue. To explore such issues, we have studied over 100 serial skin biopsies from five full facial transplantation patients with allograft rejection episodes, with the most prominent changes comprehensively evaluated by using relevant biomarkers. Our findings prompt a re-examination of the Banff 2007 criteria when applied to facial transplantation. The face as a unique anatomic site is often subjected to extensive sun-exposure and prone to a variety of conditions that may persist in allografts, such as rosacea,32 seborrheic dermatitis, or other dermatoses that may confound application of Banff criteria. This is particularly germane to Banff grades I and II rejection that require only lymphocytic inflammation. Moreover, facial skin is structurally different from non-facial sites. This includes (a) increased density and distinctive microanatomy of pilosebaceous structures involved in rejection-related targeting; (b) frequent presence of excessive elastosis because of UV damage; (c) altered migration and function of dendritic immune cells (eg, Langerhans cells) as a result of chronic UVB irradiation;33 and (d) potential presence of draining skin-associated lymph nodes in peri-parotid and subcutaneous tissues. Because skin and subcutis recently have been recognized to represent vast reservoirs for Trm cells that may elicit local immune responses,20, 34, 35, 36 donor T-cell-driven predisposition to various dermatoses in transplanted facial allografts also must now be considered when establishing criteria for the diagnosis and grading of rejection.30
It is noteworthy that lymphocytic vasculitis was a prominent feature of facial transplant rejection in our study and one in keeping with early descriptions of skin allograft rejection by Dvorak et al, where the dermal microvasculature was proposed to be a primary target.5 This feature so prominently observed in rejecting facial skin is not included in the current Banff criteria for application to face transplant rejection.8 Although lymphocytic vasculitis is associated with reproducible endothelial degenerative alterations, including cell sloughing, it is important not to confuse it with neutrophil-mediated vasculitis because of immune complex deposition, where fibrinoid vessel wall necrosis and nuclear fragmentation typically occurs. Accordingly, further refinements in grading schemas for facial transplant rejection should consider the microvasculature as a potentially informative indicator of disease activity. We also found that anagen follicular apoptosis, in contrast to epidermal apoptosis, persists in the remission phase following rejection (Figure 3 and Supplementary Figure 2). This finding after rejection could confound assessment of active disease in the setting of follicular inflammation unrelated to persistent rejection (Banff grade III requires apoptosis and inflammation, as an indicator of severe rejection).8 This point is particularly emphasized by predisposition of facial skin to show sparse perifollicular lymphoid infiltrates, and the documented occurrence of rosacea in donor skin of a previous transplant at our institution.32 Mechanistically, it is likely that residual follicular apoptosis in anagen follicles post rejection relates kinetically to inability of follicular turnover to eradicate such cells as efficiently as the surface epidermis.37 A preliminary schema for the histopathologic evaluation of full facial transplants that encapsulates the above concerns is offered in Table 2.
The finding of abundant skin-resident T cells of donor origin as a major immune biomarker associated with vascular, pilosebaceous, and epidermal sites of injury in rejecting facial allografts was unexpected and represents a potential paradigm shift from the conventional view implicating recipient T cells as effectors. Streilein first drew attention to skin as an immunologic organ with the term ‘skin-associated lymphoid tissue’.38 Today, skin is recognized as a rich repository of resident lymphocytes that provide protection by patrolling for pathogens and other noxious antigens.20, 39 In 2001, Hayday et al rekindled interest in T cells resident to the skin.40 In 2003, Curry et al for the first time established the replicative potential of resident T cells exposed to variety of immunologic stimuli in healthy-appearing ‘normal’ human skin.41 Finally, Clark, Kupper, and co-workers recently have shown that non-circulating pools of resident CD8+ T cells are abundant in human skin and are capable of cytotoxic responses against vaccinia.20 Such Trm cells also may respond to HSV infection, where the CD8+ phenotype mediates epidermal involvement, and the CD4+ subset is engaged in deeper dermal interactions.39 The donor cells noted in the present study of facial allograft rejection express CD69, CD103 and CLA biomarkers, defining them as Trm cells.35, 42, 43, 44 Their spatial association with sites of epithelial and endothelial injury strongly implicates donor T cells in the pathogenesis of rejection. The finding of donor Trm cells in facial allograft rejection occurring as much as 23 months after transplantation is consistent with the current belief that such cells remain in skin for long periods of time and are capable of immune responses many months after their initial recruitment. Although functional studies are now required elucidating the role of donor resident T cells in facial allograft rejection, it is unlikely that syngeneic donor keratinocytes and endothelial cells are their primary targets. The possibility that recipient epithelial or endothelial chimerism may provide targets for donor Trm cells was also considered, although this phenomenon was only infrequently encountered. Although it remains possible that proliferation of donor Trm may be unrelated to allo-antigenic stimulation, we hypothesize that allo-stimulated recipient lymphocytes and mononuclear cells that characteristically home to the dermal vascular compartment, epidermis, and pilosebaceous microenvironments may provide MHC targets for alloreactivity mediated by donor Trm cells. Cytotoxic interactions between donor and recipient immune cells may thus contribute to conventional target cell injury via collateral damage implicit to immune cell warfare within these restricted microenvironmental niches. To date, graft-versus-host disease has not been reported in facial allograft transplant patients,30 as may occur rarely when passenger leukocytes in organ transplants attack recipient tissues. However, we propose that our data, although descriptive and requiring functional validation, raises the possibility that facial allograft rejection involves a localized (intra-graft) graft-versus-host disease-like donor T-cell-mediated immune response directed against recipient leukocytes infiltrating the engrafted tissues.
Our study has several significant limitations. Although the donor origin of T cells was determined at the levels of reactivity with a donor-specific class I epitope, absence of reactivity of recipient-class I epitope, and co-localization with three donor resident T-cell markers, it would be useful in future studies to further confirm these findings at the mRNA/DNA levels. However, such an approach would require immuno-guided laser capture microdissection in frozen tissue that was not available in the present study. In addition, expansion of immunophenotyping to include detailed analysis of dendritic cells of established importance in alloreactivity is now also indicated.45 Site variation in determining in diagnosing and grading rejection must also be further explored, particularly in light of the robust study by Bergfeld et al, where examination of a large number of cutaneous and mucosal biopsies from a single face transplant patient indicated greater diagnostic sensitivity at the latter site.29 Moreover, functional validation of the phenotypic findings presented herein will be required to more definitively understand the role of donor T cells in the rejection process. Finally, more comprehensive studies correlating detailed biomarker analysis of skin samples with systemic parameters of rejection are now indicated.
The finding of donor T cells as a major constituent of facial allograft rejection has several potentially important clinical implications. Although donor T cells are likely to participate in ‘passenger dermatoses’ inherit to the transplant procedure, their abundance in conjunction with onset of clinical signs of rejection coupled with their spatial association with specific target sites may have biomarker value in the diagnosis of facial allograft rejection. Moreover, antigenic stimuli at variable times after transplantation that may activate memory or cognate responses in donor cells resident within the facial allografts now must be considered, in addition to changes in immunosuppressive therapy, as possible provocative events for rejection-like phenomena. Whether pre-transplant manipulation of donor resident T cells in facial grafts will influence rejection remains to be examined. Resident T cells within tracheal allografts have been shown to be radiation sensitive,46 raising the possibility that pre-transplant irradiation or other means of purging donor T cells from grafts might influence the clinical course of rejection post-transplant. Major strides have already been accomplished in understanding vascular composite allotransplantation rejection and biology,22, 23, 24, 25, 26, 27, 28, 29 and the Banff system is clearly useful in assessing allograft rejection. However, our findings underscore the critical role for further refinements in histopathology and biomarker application to the accurate diagnosis, therapeutic monitoring, and mechanistic understanding of vascular composite tissue transplantation.
References
Lefaucheur C, Loupy A, Vernerey D et al. Antibody-mediated vascular rejection of kidney allografts: a population-based study. Lancet 2013;381:313–319.
Bagnasco S, Kraus E, Sis B . Diagnostic criteria for kidney transplant rejection: a call to action. Lancet 2013;381:1458.
Gibson T, Medawar PB . The fate of skin homografts in man. J Anat 1943;77:299310 4.
Hancock WW, Murphy GF . Skin Grafts and their Rejections in the Pathology of Organ Transplantation. Butterworths: Boston, MA, 1990.
Dvorak HF, Mihm MC Jr, Dvorak AM et al. Rejection of first-set skin allografts in man. the microvasculature is the critical target of the immune response. J Exp Med 1979;150:322–337.
Bhan AK, Mihm MC Jr, Dvorak HF . T cell subsets in allograft rejection. In situ characterization of T cell subsets in human skin allografts by the use of monoclonal antibodies. J Immunol 1982;129:1578–1583.
Pomahac B, Pribaz J, Eriksson E et al. Three patients with full facial transplantation. N Engl J Med 2012;366:715–722.
Cendales LC, Kanitakis J, Schneeberger S et al. The Banff 2007 working classification of skin-containing composite tissue allograft pathology. Am J Transplant 2008;8:1396–1400.
Bueno EM, Diaz-Siso JR, Pomahac B . A multidisciplinary protocol for face transplantation at Brigham and Women’s Hospital. J Plast Reconstr Aesthet Surg 2011;64:1572–1579.
Hirahara K, Liu L, Clark RA et al. The majority of human peripheral blood CD4+CD25highFoxp3+ regulatory T cells bear functional skin-homing receptors. J Immunol 2006;177:4488–4494.
Lim HW, Broxmeyer HE, Kim CH . Regulation of trafficking receptor expression in human forkhead box P3+ regulatory T cells. J Immunol 2006;177:840–851.
Ariotti S, Beltman JB, Chodaczek G et al. Tissue-resident memory CD8+ T cells continuously patrol skin epithelia to quickly recognize local antigen. Proc Natl Acad Sci USA 2012;109:19739–19744.
Mackay LK, Stock AT, Ma JZ et al. Long-lived epithelial immunity by tissue-resident memory T (TRM) cells in the absence of persisting local antigen presentation. Proc Natl Acad Sci USA 2012;109:7037–7042.
Mizukawa Y, Yamazaki Y, Teraki Y et al. Direct evidence for interferon-gamma production by effector-memory-type intraepidermal T cells residing at an effector site of immunopathology in fixed drug eruption. Am J Pathol 2002;161:1337–1347.
Bronstein BR, Murphy GF, Harrist TJ et al. Location of HLA-A,B,C antigens in dendritic cells of normal human skin: an immunoelectron microscopic study. J Invest Dermatol 1983;80:481–484.
Natali PG, Bigotti A, Nicotra MR et al. Distribution of human Class I (HLA-A,B,C) histocompatibility antigens in normal and malignant tissues of nonlymphoid origin. Cancer Res 1984;44:4679–4687.
Caughman SW, Sharrow SO, Shimada S et al. Ia+ murine epidermal Langerhans cells are deficient in surface expression of the class I major histocompatibility complex. Proc Natl Acad Sci USA 1986;83:7438–7442.
Ruckert R, Hofmann U, van der Veen C et al. MHC class I expression in murine skin: developmentally controlled and strikingly restricted intraepithelial expression during hair follicle morphogenesis and cycling, and response to cytokine treatment in vivo. J Invest Dermatol 1998;111:25–30.
Wang X, Campoli M, Cho HS et al. A method to generate antigen-specific mAb capable of staining formalin-fixed, paraffin-embedded tissue sections. J Immunol Methods 2005;299:139–151.
Jiang X, Clark RA, Liu L et al. Skin infection generates non-migratory memory CD8+ T(RM) cells providing global skin immunity. Nature 2012;483:227–231.
Carty MJ, Bueno EM, Lehmann LS et al. A position paper in support of face transplantation in the blind. Plast Reconstr Surg 2012;130:319–324.
Hautz T, Zelger B, Brandacher G et al. Histopathologic characterization of mild rejection (grade I) in skin biopsies of human hand allografts. Transpl Int 2012;25:56–63.
Morelon E, Kanitakis J, Petruzzo P . Immunological issues in clinical composite tissue allotransplantation: where do we stand today? Transplantation 2012;93:855–859.
Kanitakis J, Jullien D, Petruzzo P et al. Clinicopathologic features of graft rejection of the first human hand allograft. Transplantation 2003;76:688–693.
Kanitakis J, Badet L, Petruzzo P et al. Clinicopathologic monitoring of the skin and oral mucosa of the first human face allograft: Report on the first eight months. Transplantation 2006;82:1610–1615.
Eljaafari A, Badet L, Kanitakis J et al. Isolation of regulatory T cells in the skin of a human hand-allograft, up to six years posttransplantation. Transplantation 2006;82:1764–1768.
Petruzzo P, Testelin S, Kanitakis J et al. First human face transplantation: 5 years outcomes. Transplantation 2012;93:236–240.
Hautz T, Zelger B, Grahammer J et al. Molecular markers and targeted therapy of skin rejection in composite tissue allotransplantation. Am J Transplant 2010;10:1200–1209.
Bergfeld W, Klimczak A, Stratton JS et al. A 4-year pathology review of the near total face transplant. Am J Transplant 2013;13:2750–2764.
Siemionow M, Ozturk C . Face transplantation: outcomes, concerns, controversies, and future directions. J Craniofac Surg 2012;23:254–259.
Solez K, Racusen LC . The Banff classification revisited. Kidney Int 2013;83:201–206.
Saavedra AP, Bueno EM, Granter SR et al. Transmission of donor-specific skin condition from donor to recipient of facial allograft. Am J Transplant 2011;11:1340.
Kolgen W, Both H, van Weelden H et al. Epidermal langerhans cell depletion after artificial ultraviolet B irradiation of human skin in vivo: apoptosis versus migration. J Invest Dermatol 2002;118:812–817.
Gebhardt T, Whitney PG, Zaid A et al. Different patterns of peripheral migration by memory CD4+ and CD8+ T cells. Nature 2011;477:216–219.
Clark RA, Chong B, Mirchandani N et al. The vast majority of CLA+ T cells are resident in normal skin. J Immunol 2006;176:4431–4439.
Clark RA, Chong BF, Mirchandani N et al. A novel method for the isolation of skin resident T cells from normal and diseased human skin. J Invest Dermatol 2006;126:1059–1070.
Halprin KM . Epidermal ‘turnover time’—a re-examination. Br J Dermatol 1972;86:14–19.
Streilein JW . Skin-associated lymphoid tissues (SALT): origins and functions. J Invest Dermatol 1983;80 (Suppl):12s–16ss.
Zhu J, Peng T, Johnston C et al. Immune surveillance by CD8alphaalpha+ skin-resident T cells in human herpes virus infection. Nature 2013;497:494–497.
Hayday A, Theodoridis E, Ramsburg E et al. Intraepithelial lymphocytes: exploring the Third Way in immunology. Nat Immunol 2001;2:997–1003.
Curry JL, Qin JZ, Robinson J et al. Reactivity of resident immunocytes in normal and prepsoriatic skin using an ex vivo skin-explant model system. Arch Pathol Lab Med 2003;127:289–296.
Clark RA . Skin-resident T cells: the ups and downs of on site immunity. J Invest Dermatol 2010;130:362–370.
Gebhardt T, Mackay LK . Local immunity by tissue-resident CD8(+) memory T cells. Front Immunol 2012;3:340.
Mueller SN, Gebhardt T, Carbone FR et al. Memory T cell subsets, migration patterns, and tissue residence. Annu Rev Immunol 2013;31:137–161.
Nestle FO, Di Meglio P, Qin JZ et al. Skin immune sentinels in health and disease. Nat Rev Immunol 2009;9:679–691.
Yokomise H, Inui K, Wada H et al. High-dose irradiation prevents rejection of canine tracheal allografts. J Thorac Cardiovasc Surg 1994;107:1391–1397.
Acknowledgements
This study is supported in part by R01 HL084815 (GFM), R01 CA158467 (GFM), R01 AG039449 (SGT), and research contract #W911QY-09-C-2016 and W81XWH-12-2-0037 between the United States Department of Defense and The Brigham and Women's Hospital (EB, SGT and BP). GFM receives funding from Bristol-Meyer Squibb for a project on melanoma biomarker research that is unrelated to the present study. We thank Dr Travis Hollmann for his participation of the diagnoses of several biopsy specimens described in this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Rights and permissions
About this article
Cite this article
Lian, C., Bueno, E., Granter, S. et al. Biomarker evaluation of face transplant rejection: association of donor T cells with target cell injury. Mod Pathol 27, 788–799 (2014). https://doi.org/10.1038/modpathol.2013.249
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.249
Keywords
This article is cited by
-
Unique properties of tissue-resident memory T cells in the lungs: implications for COVID-19 and other respiratory diseases
Nature Reviews Immunology (2023)
-
Human circulating and tissue-resident memory CD8+ T cells
Nature Immunology (2023)
-
Human mucosal tissue-resident memory T cells in health and disease
Mucosal Immunology (2022)
-
Local heroes or villains: tissue-resident memory T cells in human health and disease
Cellular & Molecular Immunology (2020)
-
Skin Immunology and Rejection in VCA and Organ Transplantation
Current Transplantation Reports (2020)