Abstract
On the basis of morphological features, we subclassified 189 intrahepatic cholangiocarcinomas into two subtypes: bile duct and cholangiolar. The cholangiolar type is composed of cuboidal to low columnar tumor cells that contain scanty cytoplasm. The bile duct type is composed of tall columnar tumor cells arranged in a large glandular pattern. In this study, 77 (41%) tumors were classified as the cholangiolar type and 112 (59%) tumors were classified as the bile duct type. The cholangiolar-type intrahepatic cholangiocarcinoma was more frequently associated with viral hepatitis, whereas all but one intrahepatic cholangiocarcinoma associated with intrahepatic lithiasis were classified as the bile duct type. Biliary intraepithelial neoplasm or intraductal papillary neoplasm of the bile duct could be identified in 50 bile duct-type intrahepatic cholangiocarcinomas (45%), but in only 3 cholangiolar-type intrahepatic cholangiocarcinomas (4%). Cholangiolar-type intrahepatic cholangiocarcinomas frequently expressed N-cadherin, whereas bile duct intrahepatic cholangiocarcinomas were more likely to express S100P, Trefoil factor 1, and anterior gradient 2. KRAS is mutated in 23 of 98 (23%) bile duct-type intrahepatic cholangiocarcinomas and in only 1 of 76 (1%) cholangiolar-type intrahepatic cholangiocarcinomas. Cholangiolar-type intrahepatic cholangiocarcinomas had a higher frequency of IDH1 or 2 mutations than did the bile duct-type intrahepatic cholangiocarcinomas. The molecular features of the bile duct-type intrahepatic cholangiocarcinoma were similar to those of hilar cholangiocarcinoma. Patients with the cholangiolar-type intrahepatic cholangiocarcinoma had higher 5-year survival rates than those of patients with the bile duct-type intrahepatic cholangiocarcinoma. Our results indicated that intrahepatic cholangiocarcinoma was a heterogeneous tumor. Subclassification of intrahepatic cholangiocarcinomas based on cholangiocytic differentiation divides them into two groups with different etiologies, clinical manifestations, and molecular pathogeneses.
Similar content being viewed by others
Main
Intrahepatic cholangiocarcinoma is the second most common primary liver cancer after hepatocellular carcinoma. The incidence of intrahepatic cholangiocarcinoma varies widely worldwide and is more prevalent in East Asia than in Western countries,1 mainly because of infestation by the liver flukes Clonorchis sinensis and Opisthorchis viverrini.2, 3 Other known etiological factors for intrahepatic cholangiocarcinoma include hepatolithiasis, primary sclerosing cholangitis, exposure to the radiopaque medium thorium dioxide (Thorotrast), biliary tract anatomical anomalies, and hepatitis B and C infections.4, 5, 6, 7, 8, 9 However, most patients diagnosed with cholangiocarcinoma do not have a recognized risk factor. The molecular mechanisms for carcinogenesis and tumor progression of intrahepatic cholangiocarcinoma are still poorly characterized. Despite intensive research, managing this cancer remains challenging, because most patients are at an advanced stage at the time of diagnosis, and no effective therapy for unresectable tumors exists.10
On the basis of gross morphological features, intrahepatic cholangiocarcinoma can be classified into three subtypes: mass forming, periductal infiltrating, and intraductal.11 Mass forming is the most common type, in which a definite mass forms within liver parenchyma. The periductal infiltrating type is composed of tumor cells that grow longitudinally along large bile ducts. The intraductal type is characterized by tumor cells growing toward the lumina of large bile ducts in a papillary configuration.11 The different growth patterns suggest that intrahepatic cholangiocarcinomas are heterogeneous tumors possessing different cells of origin and different pathogeneses. It is likely that periductal and intraductal tumors arise from malignant transformation of epithelial cells lining the larger bile ducts, whereas the mass-forming type arises from smaller bile ducts or bipotential hepatic progenitor cells within portal areas.
In a previous study, we demonstrated that intrahepatic cholangiocarcinoma can be further subclassified into two groups based on the resemblance of tumor cells to large bile duct cells (bile duct type) or cholangiolar cells (cholangiolar type).12 We discovered that cholangiolar-type intrahepatic cholangiocarcinoma is strongly associated with viral hepatitis.12 However, the etiological, clinicopathological, and molecular significance of this classification system has not been fully explored. In this study, we analyzed a large cohort of patients diagnosed with intrahepatic cholangiocarcinoma to prove that intrahepatic cholangiocarcinoma can be subclassified according to morphology into two groups with different etiologies, clinical features, immunophenotypes, molecular alterations, and prognoses.
Materials and methods
Patients and Tissue Samples
For this study, we selected 189 intrahepatic cholangiocarcinoma patients and 40 patients diagnosed with hilar cholangiocarcinomas who had undergone surgical resection and had received detailed pathological assessment and regular follow-ups at National Taiwan University Hospital from 1993 to 2012. All specimens were meticulously examined by one pathologist to exclude combined hepatocellular and cholangiocarcinoma. The study was conducted according to the regulations of the Research Ethics Committee of National Taiwan University Hospital. The specimens were anonymous and analyzed using a blinded method.
Immunohistochemistry
Tissue sections (5 μm) were dewaxed and rehydrated. Antigen retrieval was performed by incubating slides in 0.01 M of a citric acid buffer at 100 °C for 10 min. After being blocked with 3% H2O2 and 5% fetal bovine serum, the slides were allowed to react with primary antibodies at 4 °C overnight. The slides were then incubated with a polymer-HRP reagent (BioGenex, San Ramon, CA, USA). The peroxidase activity was visualized using a diaminobenzidine tetrahydroxychloride solution (BioGenex). The sections were counterstained with hematoxylin. For the negative controls, the primary antibody was replaced with 5% fetal bovine serum. The primary antibodies used were directed against the following antigens: N-cadherin (clone IAR06, 1:100; Leica Microsystems, Wetzlar, Germany), S100P (goat polyclonal, 1:200; R&D Systems, Minneapolis, MN, USA), Trefoil factor 1 (TFF1) (clone EPR3972, 1:100; Epitomics, Burlingame, CA, USA), and anterior gradient 2 (AGR2) (rabbit polyclonal, 1:100; Abcam, Cambridge, MA, USA). N-cadherin had a membranous staining pattern. S100P had a nuclear and cytoplasmic staining pattern. TFF1 and AGR2 were stained in the cytoplasm. For each marker, positive staining in more than 5% of the tumor cells was considered positive.
Mutation Detection
Analyses of KRAS, IDH1, and IDH2 mutations were conducted using DNA extracted from formalin-fixed, paraffin-embedded tissues. In brief, 10-μm sections were cut from paraffin blocks, and the tumor parts were dissected and collected. Tumors with cancer cell density of <10% were excluded because they were below the detection threshold of direct sequencing. Genomic DNA was extracted using a QIAamp DNA FFPE Tissue Kit (Qiagen, Santa Clarita, CA, USA) according to the manufacturer’s protocol. Mutation hot spots of KRAS, IDH1, and IDH2 were amplified by polymerase chain reaction. The primers used were: KRAS-F (5′-GAATGGTCCTGCACC AGTAA-3′) and KRAS-R (5′-GTGTGACATGTTCTAATATAGTCA-3′); IDH1-F (5′-AAACAAATGTGGAAATCACC-3′) and IDH1-R (5′-TGCCAACATGACTTACTTGA-3′); IDH2-F (5′-AGAAGATGTGGAAAAGTCCC-3′) and IDH2-R (5′-CAGAGACAAGAGGATGGCTAGG-3′). After purification, direct sequencing was performed using an automated ABI 3770 sequencer (Applied BioSystems, Foster City, CA, USA).
Statistical Analysis
The data analyses were conducted using Epi Info (version 3.3.2; Centers for Disease Control and Prevention) or MedCalc (version 14.4.2.0; MedCalc Software, Mariakerke, Belgium). Comparisons of categorical variables were performed using the Pearson’s χ2 method. Continuous variables were analyzed using the Student’s t-test. The interobserver agreement was calculated using the online kappa calculator (http://justusrandolph.net/kappa/). The survival rates after tumor resection were calculated using the Kaplan–Meier method, and the difference in the survival curves was analyzed using the log-rank test. A multivariate survival analysis of all the parameters that were found to be significantly correlated with prognosis in the univariate analysis was performed using a Cox proportional-hazards regression model. All statistical results were considered significant if the P-value was <0.05.
Results
Histological Classification of Intrahepatic Cholangiocarcinoma
We subclassified intrahepatic cholangiocarcinoma according to histological features into two types: cholangiolar and bile duct. The cholangiolar type is composed of cuboidal to low columnar tumor cells that contain scanty eosinophilic or amphophilic cytoplasm and are typically arranged in small monotonous glands (Figure 1a). The cholangiolar type can also be arranged in anastomosing trabeculae, cribriform, micropapillary, or solid patterns (Figures 1b–d). Except for the central areas of some cases, the tumors usually exhibit high cellularity and scant stroma. The nuclei are usually low to intermediate grade, but some tumors with high-grade nuclei are also included in this group as long as the tumor cells are cuboidal and contain scanty cytoplasm (Figure 1e). In six cases, abundant lymphocytes infiltrate within tumors, which fulfill the criteria of lymphoepithelioma-like cholangiocarcinoma (Figure 1f).13
Morphology of cholangiolar-type intrahepatic cholangiocarcinoma. The tumors are composed of cuboidal to low columnar tumor cells that contain scanty eosinophilic or amphophilic cytoplasm. It can be arranged in glandular (a), micropapillary (b), solid (c), or cribriform (d) patterns. (e) A cholangiolar-type intrahepatic cholangiocarcinoma with high-grade nuclei. (f) A lymphoepithelioma-like cholangiocarcinoma. Original magnification: × 200.
The bile duct type is composed of tall columnar tumor cells arranged in a large glandular pattern. Compared with cholangiolar-type intrahepatic cholangiocarcinomas, bile duct-type intrahepatic cholangiocarcinomas usually exhibit lower cellularity and abundant desmoplastic stroma (Figure 2a). Bile duct-type tumor cells have a lower nuclear-to-cytoplasmic ratio compared with cholangiolar-type tumors, and contain abundant clear, eosinophilic, or mucinous cytoplasm (Figures 2b and c). Extracellular mucin can be seen in glandular spaces (Figure 2d).
Morphology of bile duct-type intrahepatic cholangiocarcinoma. (a) On low-power view, bile duct-type intrahepatic cholangiocarcinomas usually exhibit lower cellularity and abundant desmoplastic stroma. (b and c) The tumor cells are tall columnar and have abundant clear (b) or eosinophilic cytoplasm (c). (d) A bile duct-type intrahepatic cholangiocarcinoma with extracellular mucin. Original magnification, a: × 40; b–d: × 200.
On the basis on these criteria, three pathologists read the slides and independently classified the 189 intrahepatic cholangiocarcinomas into cholangiolar and bile duct types. The interobserver agreement in the subclassification was extremely high, at a κ of 0.81. The consensus tumor type was used for subsequent studies. Seventy-seven (41%) tumors were classified as the cholangiolar type and 112 (59%) were classified as the bile duct type.
Clinical and Etiological Features
As shown in Table 1, the age and sex distributions were similar for both types. Patients with bile duct-type intrahepatic cholangiocarcinoma were more likely than patients with cholangiolar-type intrahepatic cholangiocarcinoma to have jaundice as the presenting symptom with borderline statistical significance.
Viral hepatitis and intrahepatic lithiasis were two most important etiological factors of intrahepatic cholangiocarcinoma in Taiwan.12 In this cohort, 76 patients had chronic hepatitis B or C infection (40%) and 25 patients had intrahepatic lithiasis (13%). Viral hepatitis was more associated with the cholangiolar type than with the bile duct type (P=0.03). By contrast, all but one intrahepatic cholangiocarcinoma associated with intrahepatic lithiasis were classified as the bile duct type (P=0.00005). The six lymphoepithelioma-like carcinomas, which all belong to the cholangiolar-type intrahepatic cholangiocarcinoma in this classification, were positive for EBER-1 in situ hybridization.
Pathological Features
According to gross morphology, 35 intrahepatic cholangiocarcinomas were classified as the intraductal/periductal type and 154 intrahepatic cholangiocarcinomas were classified as the mass-forming type. All 35 intraductal/periductal intrahepatic cholangiocarcinomas were the bile duct type, whereas the mass-forming type were evenly divided into cholangiolar and bile duct types (P=10−7). The tumor size of the mass-forming type intrahepatic cholangiocarcinoma was similar for both histological subtypes.
There are two types of precursor lesions for intrahepatic cholangiocarcinoma: biliary intraepithelial neoplasm and intraductal papillary neoplasm of the bile duct.14 Reviewing the histological sections, we discovered 46 tumors had biliary intraepithelial neoplasm components and 7 tumors had intraductal papillary neoplasm of the bile duct components. Precursor lesions can be identified in 50 bile duct-type intrahepatic cholangiocarcinomas (45%), but in only 3 cholangiolar-type intrahepatic cholangiocarcinomas (4%) (P<10−7). All the precursors identified in cholangiolar-type intrahepatic cholangiocarcinomas were biliary intraepithelial neoplasms.
Bile duct-type intrahepatic cholangiocarcinomas were more likely to have lymph node metastasis at the time of surgery (P=0.0244).
Immunohistochemical Features
To prove the morphologic subtype correlates with immunophenotype of normal bile ducts, we analyzed the expression of N-cadherin, S100P, TFF1 and AGR2 in these tumors (Figure 3). N-cadherin is expressed in hepatocytes, ductules, and small bile ducts, but not in extrahepatic and large intrahepatic bile ducts.12 S100P, TFF1, and AGR2 were frequently expressed in pancreatic adenocarcinoma and, according to previous studies, have also been expressed in some cases of hilar and intrahepatic cholangiocarcinomas.15, 16, 17 Cholangiolar-type intrahepatic cholangiocarcinomas express N-cadherin more frequently than bile duct-type intrahepatic cholangiocarcinomas (P<10−7). However, bile duct-type intrahepatic cholangiocarcinomas exhibit much higher frequencies of expression of S100P, TFF1, and AGR2 (P<10−7, =0.00007, =10−7, respectively).
Immunophenotype of bile duct-type (a, c, e, g) and cholangiolar-type (b, d, f, h) intrahepatic cholangiocarcinomas. Bile duct-type intrahepatic cholangiocarcinomas were typically negative for N-cadherin (a) and positive for TFF1 (c), S100P (e), and AGR2 (g). Cholangiolar-type intrahepatic cholangiocarcinomas were typically positive for N-cadherin (b) and negative for TFF1 (d), S100P (f), and AGR2 (h).
Mutation Analysis
KRAS is the most frequently mutated oncogene in cholangiocarcinoma.18 Direct sequencing showed that 23 of 98 (23%) bile duct-type intrahepatic cholangiocarcinomas harbored KRAS mutation. By contrast, only 1 of 76 (1%) cholangiolar-type intrahepatic cholangiocarcinomas harbored KRAS mutation (P=0.00003).
IDH1 and 2 were recently discovered to be mutated in intrahepatic cholangiocarcinoma.19 Direct sequencing showed 14 and 4 of 171 intrahepatic cholangiocarcinomas harbored mutations of IDH1 and IDH2, respectively. The primary IDH1 mutations in intrahepatic cholangiocarcinomas resulted in the codon change p.R132C (n=9), followed by p.R132G (n=3) and p.R132L (n=2). The four IDH2 mutations in intrahepatic cholangiocarcinoma resulted in the codon change p.R172W (n=3) and p.R172K (n=1). It is interesting to note that cholangiolar-type intrahepatic cholangiocarcinomas revealed a higher frequency of IDH1 and 2 mutations than did bile duct-type intrahepatic cholangiocarcinomas (P=0.0121).
Comparison with Hilar Cholangiocarcinoma
Forty hilar cholangiocarcinomas were included for immunohistochemical and genetic studies. The results are shown in Table 2. Except for N-cadherin expression, which is rarely expressed in hilar cholangiocarcinoma, the expression frequency of S100P, TFF1, and AGR2, as well as the mutation frequency of KRAS and IDH1/2 of bile duct-type intrahepatic cholangiocarcinomas, were statistically indistinguishable from hilar cholangiocarcinoma. By contrast, the immunophenotype and molecular features of the cholangiolar-type intrahepatic cholangiocarcinomas were markedly different from those of hilar cholangiocarcinoma.
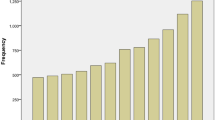
Patient Outcome
The patients received follow-up care to a maximum of 5 years after surgery. A total of 123 patients died within 5 years. The median follow-up period of the survivors was 4.2 years (range of 7 months–5 years). The Kaplan–Meier survival analysis showed that patients with a cholangiolar-type intrahepatic cholangiocarcinoma had a higher 5-year survival rate than those of patients with bile duct-type intrahepatic cholangiocarcinoma (P=0.005) (Figure 4).
Univariate analyses identified tumor subtype, presence of intrahepatic lithiasis, tumor grade, T stage, lymph node metastasis, and tumor size were prognostic factors, whereas patient age, sex, presence of jaundice, viral hepatitis status, and KRAS and IDH1/2 mutations were not related to patient prognosis. A multivariate analysis showed that the presence of intrahepatic lithiasis, tumor grade, T stage, lymph node metastasis, and tumor size were independent prognostic factors, but tumor subtype was not a significantly independent prognostic factor (data not shown).
Discussion
In this study, we classified intrahepatic cholangiocarcinomas based on histological features into two subtypes and discovered that the two subtypes were different in etiological, clinical, and molecular features. The cholangiolar-type intrahepatic cholangiocarcinoma was associated with viral hepatitis, expressed N-cadherin, and was more likely to have IDH1/2 mutations. In addition, patients diagnosed with cholangiolar-type intrahepatic cholangiocarcinoma had a better prognosis than those diagnosed with bile duct-type intrahepatic cholangiocarcinoma. By contrast, bile duct-type intrahepatic cholangiocarcinoma was associated with intrahepatic lithiasis, frequently exhibited precursor lesions, expressed markers of hilar cholangiocarcinoma and pancreatic cancer, and was more likely to have KRAS mutations.
The concept of subclassifying intrahepatic cholangiocarcinomas according to histological features is not entirely new. Sempoux et al20 divided intrahepatic cholangiocarcinoma into two groups: classical and nonclassical. Classical intrahepatic cholangiocarcinomas are characterized by a tubular, glandular, or nested growth pattern. Nonclassical intrahepatic cholangiocarcinomas consist of tumors exhibiting trabecular architecture, tumors that exhibited features of extrahepatic carcinomas, and carcinomas considered to be derived from hepatic progenitor cells.20 It seems to us that most bile duct-type intrahepatic cholangiocarcinomas belong to the classical-type intrahepatic cholangiocarcinoma and most cholangiolar-type intrahepatic cholangiocarcinomas belong to the nonclassical-type intrahepatic cholangiocarcinoma in their classification. However, the definition of nonclassical-type intrahepatic cholangiocarcinoma seems too vague and includes several different types of tumors. Komuta et al21 divided intrahepatic cholangiocarcinomas into mucinous and mixed subtypes based on their resemblance to cylindrical mucin-producing cholangiocytes located in large bile ducts and the cuboidal non-mucin-producing cholangiocytes located in ductules. Our bile duct-type intrahepatic cholangiocarcinoma and cholangiolar-type intrahepatic cholangiocarcinoma were similar to the mucinous-type intrahepatic cholangiocarcinoma and mixed-type intrahepatic cholangiocarcinoma, respectively, in their study. We did not adopt the mucinous/mixed terminology because many bile duct-type intrahepatic cholangiocarcinomas showed abundant eosinophilic cytoplasm and did not demonstrate mucin production. In their study, mucinous intrahepatic cholangiocarcinoma showed more frequent lymphovascular and perineural invasion. Consistent with this finding, we discovered that patients with a bile duct-type intrahepatic cholangiocarcinoma had a poorer prognosis than did those with a cholangiolar-type intrahepatic cholangiocarcinoma. In addition, S100P, which is a marker of bile duct-type intrahepatic cholangiocarcinoma in our study, was also a marker of hilar or mucinous intrahepatic cholangiocarcinoma in their study.
The different morphologies of bile duct-type intrahepatic cholangiocarcinomas and cholangiolar-type intrahepatic cholangiocarcinomas may reflect different histogenesis. The bile duct-type intrahepatic cholangiocarcinoma may derive from cholangiocytes that line large bile ducts, whereas the cholangiolar-type intrahepatic cholangiocarcinoma more likely derives from bipotential hepatic progenitor cells located within portal areas. The most direct evidence is that biliary intraepithelial neoplasm or intraductal papillary neoplasm of the bile duct can be identified in approximately 45% of bile duct-type intrahepatic cholangiocarcinomas but in only 4% of cholangiolar-type intrahepatic cholangiocarcinomas. The different etiological factors may also suggest distinct precursor cells. Intrahepatic lithiasis causes erosion and regeneration of biliary epithelial cells, resulting in biliary intraepithelial neoplasm, followed by bile duct-type intrahepatic cholangiocarcinomas. Viral hepatitis destroys liver parenchyma and causes activation of hepatic progenitor cells, leading to cholangiolar-type intrahepatic cholangiocarcinomas. It is likely that two main pathways of intrahepatic cholangiocarcinoma pathogenesis exist. Genetic change in bile duct epithelial cells result in biliary intraepithelial neoplasm or intraductal papillary neoplasm of the bile duct. Additional mutations created more aggressive phenotypes and, hence, bile duct-type intrahepatic cholangiocarcinomas. Mutations in hepatic progenitor cells, through currently unknown precursor lesions, resulted in cholangiolar-type intrahepatic cholangiocarcinomas.
The bile duct-type intrahepatic cholangiocarcinoma is similar to the hilar cholangiocarcinoma, extrahepatic bile duct adenocarcinoma, and pancreatic adenocarcinoma in morphology, immunophenotype, and genetic change. Currently, hilar cholangiocarcinoma is defined as tumors arising from the right and left hepatic ducts at or near their junction and is considered to be an extrahepatic lesion.22 However, because the bile duct is a continuous structure, it is likely that the more upstream portion of the bile duct is susceptible to similar diseases that the hilar bile duct is prone to. The finding of similar molecular features of bile duct-type intrahepatic cholangiocarcinoma to hilar cholangiocarcinoma, extrahepatic adenocarcinoma, and pancreatic adenocarcinoma suggests that these tumor groups may be treated using similar systemic therapy protocols. The intrahepatic cholangiocarcinoma subtype should be considered in future clinical trials.
The prototypical examples of cholangiolar-type intrahepatic cholangiocarcinoma were combined hepatocellular–cholangiocarcinoma with stem cell features, and the cholangiolocellular type, also known as cholangiolocarcinoma.23 Cholangiolocarcinoma is defined as composed of population of small cells with high nuclear-to-cytoplasmic ratios and hyperchromatic, oval nuclei, growing in a tubular, cord-like, or anastomosing pattern.23 Cholangiolocarcinoma was considered to be a very rare tumor type. The concept of cholangiolocarcinoma as a variant of combined hepatocellular–cholangiocarcinoma with stem cell features is still not universally accepted. Cholangiolocarcinoma does not show features of hepatocellular differentiation (personal observation, Jeng YM). In the World Health Organization classification, a typical example of cholangiolocarcinoma was shown as a well-differentiated tubular cholangiocarcinoma in the section of intrahepatic cholangiocarcinoma (p 220, Figure 10.48C). Our definition of the cholangiolar type includes tumors with different architectures as long as the tumors are small cuboidal cells with high nuclear-to-cytoplasmic ratios. This definition is not limited to those with tubular architectures. Tumors with high-grade nuclei are also included when they are composed of cuboidal or low columnar cells with high nuclear-to-cytoplasmic ratios. Our approach is justified by the similar clinical, immunophenotypical, and molecular features. Using these definitions, cholangiolar-type intrahepatic cholangiocarcinoma accounts for approximately 40% of intrahepatic cholangiocarcinoma in Taiwan, and therefore, is not a rare tumor type. The frequencies of occurrence of cholangiolar-type intrahepatic cholangiocarcinomas in other countries have yet to be determined.
We used an immunohistochemical panel rarely used by other researchers, based on the concept that bile duct-type intrahepatic cholangiocarcinomas shared the morphology and immunophenotype of pancreatic adenocarcinoma. S100P is a 95-amino-acid calcium-binding protein initially identified in human placenta.24 S100P is expressed in nearly all cases of pancreatic adenocarcinoma and perihilar cholangiocarcinoma.25, 26 TFFs are peptides secreted by mucin-producing epithelial cells of the gastrointestinal tract involved in restitution and repair of the mucosa.27 TFF1 is normally expressed in gastric mucosa and in the adenocarcinoma of many organs, including pancreatic adenocarcinoma.28 AGR2 is a secreted protein and a potential member of the endoplasmic reticulum-associated protein disulfide isomerase family, as evidenced by its structural similarity to other protein disulfide isomerase proteins.29 AGR2 promotes the initiation and progression of pancreatic intraepithelial neoplasia.30 Recently, AGR2 was reported to be frequently expressed in hilar cholangiocarcinoma and pancreatic ductal adenocarcinoma.31 Our observation that bile duct-type intrahepatic cholangiocarcinoma shared the immunophenotype of hilar cholangiocarcinoma and pancreatic adenocarcinoma suggests these tumors derived from similar precursor cells, especially the epithelial cells lining the pancreatobiliary tree. This hypothesis is supported by the clinical experience that bile duct-type intrahepatic cholangiocarcinomas are often indistinguishable from pancreatic adenocarcinomas based on morphology and immunostaining.
Cholangiolocarcinoma is considered to exhibit stem cell features and has been reported to express stem cell markers such as keratin 19, c-kit, NCAM, and EpCAM.23 However, preliminary tests showed that keratin 19 and EpCAM were expressed in both bile duct- and cholangiolar-type intrahepatic cholangiocarcinomas. NCAM and c-kit were rarely expressed in intrahepatic cholangiocarcinoma, even in typical cases of cholangiolocarcinoma (data not shown). Consistent with our observation, Akiba et al32 discovered that c-kit was weakly expressed in only 2 of 11 cholangiolocarcinomas. In their study, NCAM was expressed in 8 of 11 cholangiolocarcinomas, but most cases showed focal or scattered expression. On the basis on these observations, we concluded that stem cell markers cannot be used for subtyping intrahepatic cholangiocarcinomas and were not included in this study.
Similar to other novel classification systems, the dichotomic division of intrahepatic cholangiocarcinomas into cholangiolar and bile duct subtypes is still not a perfect method. Some intrahepatic cholangiocarcinomas possess morphological features intermediate between the two types, and some intrahepatic cholangiocarcinomas exhibit different morphologic patterns in different regions. However, based on our research, at least 80% of our intrahepatic cholangiocarcinoma cohort can be unequivocally assigned to the subtypes. Because of the differences in etiology, molecular mechanism, and clinical outcome, intrahepatic cholangiocarcinoma subtypes should be considered in the clinical management. It is also likely that different types of intrahepatic cholangiocarcinomas may respond differently to treatment. Additional molecular and genomic studies may refine the classification.
References
Okuda K, Nakanuma Y, Miyazaki M. . Cholangiocarcinoma: recent progress. Part 1: epidemiology and etiology. J Gastroenterol Hepatol 2002;17:1049–1055.
Kurathong S, Lerdverasirikul P, Wongpaitoon V et al. Opisthorchis viverrini infection and cholangiocarcinoma: a prospective, case-controlled study. Gastroenterology 1985;89:151–156.
Lim MK, Ju YH, Franceschi S et al. Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg 2006;75:93–96.
Ohta G, Nakanuma Y, Terada T. . Pathology of hepatolithiasis: cholangitis and cholangiocarcinoma. Prog Clin Biol Res 1984;152:91–113.
Tamir BM. . Risk factors for cholangiocarcinoma. Eur J Gastroenterol Hepatol 2007;19:615–617.
Lazaridis KN, Gores GJ. . Primary sclerosing cholangitis and cholangiocarcinoma. Semin Liver Dis 2006;26:42–51.
Lipshutz GS, Brennan TV, Warren RS. . Thorotrast-induced liver neoplasia: a collective review. J Am Coll Surg 2002;195:713–718.
Kobayashi M, Ikeda K, Saitoh S et al. Incidence of primary cholangiocellular carcinoma of the liver in Japanese patients with hepatitis C virus-related cirrhosis. Cancer 2000;88:2471–2477.
Lee TY, Lee SS, Jung SW et al. Hepatitis B virus infection and intrahepatic cholangiocarcinoma in Korea: a case–control study. Am J Gastroenterol 2008;103:1716–1720.
Anderson CD, Pinson CW, Berlin J, Chari RS. . Diagnosis and treatment of cholangiocarcinoma. Oncologist 2004;9:43–57.
Yamasaki S. . Intrahepatic cholangiocarcinoma: macroscopic type and stage classification. J Hepatobiliary Pancreat Surg 2003;10:288–291.
Yu TH, Yuan RH, Chen YL et al. Viral hepatitis is associated with intrahepatic cholangiocarcinoma with cholangiolar differentiation and N-cadherin expression. Mod Pathol 2011;24:810–819.
Jeng YM, Chen CL, Hsu HC . Lymphoepithelioma-like cholangiocarcinoma: an Epstein–Barr virus-associated tumor. Am J Surg Pathol 2001;25:516–520.
Klöppel G, Adsay V, Konukiewitz B et al. Precancerous lesions of the biliary tree. Best Pract Res Clin Gastroenterol 2013;27:285–297.
Tsai JH, Huang WC, Kuo KT et al. S100P immunostaining identifies a subset of peripheral-type intrahepatic cholangiocarcinomas with morphological and molecular features similar to those of perihilar and extrahepatic cholangiocarcinomas. Histopathology 2012;61:1106–1116.
Sasaki M, Tsuneyama K, Nakanuma Y. . Aberrant expression of trefoil factor family 1 in biliary epithelium in hepatolithiasis and cholangiocarcinoma. Lab Invest 2003;83:1403–1413.
Lepreux S, Bioulac-Sage P, Chevet E . Differential expression of the anterior gradient protein-2 is a conserved feature during morphogenesis and carcinogenesis of the biliary tree. Liver Int 2011;31:322–328.
Tada M, Omata M, Ohto M . High incidence of ras gene mutation in intrahepatic cholangiocarcinoma. Cancer 1992;69:1115–1118.
Borger DR, Tanabe KK, Fan KC et al. Frequent mutation of isocitrate dehydrogenase (IDH)1 and IDH2 in cholangiocarcinoma identified through broad-based tumor genotyping. Oncologist 2012;17:72–79.
Sempoux C, Jibara G, Ward SC et al. Intrahepatic cholangiocarcinoma: new insights in pathology. Semin Liver Dis 2011;31:49–60.
Komuta M, Govaere O, Vandecaveye V et al. Histological diversity in cholangiocellular carcinoma reflects the different cholangiocyte phenotypes. Hepatology 2012;55:1876–1888.
Nakanuma Y, Curado MP, Franceschi S et al. Intrahepatic cholangiocarcinoma In: Bosman FT, Carneiro F, Hruban RH, Theise ND, (eds). WHO Classification of Tumours of the Digestive System 4th edn. International Agency for Research on Cancer: Lyon, France, 2009, pp 217–224.
Theise ND, Nakashima O, Park YN, Nakanuma Y . Combined hepatocellular–cholangiocarcinoma In: Bosman FT, Carneiro F, Hruban RH, Theise ND, (eds). WHO Classification of Tumours of the Digestive System 4th edn. International Agency for Research on Cancer: Lyon, France, 2009, pp 225–227.
Becker T, Gerke V, Kube E, Weber K . S100P, a novel Ca2+-binding protein from human placenta. cDNA cloning, recombinant protein expression and Ca2+ binding properties. Eur J Biochem 1992;207:541–547.
Dowen SE, Crnogorac-Jurcevic T, Gangeswaran R et al. Expression of S100P and its novel binding partner S100PBPR in early pancreatic cancer. Am J Pathol 2005;166:81–92.
Aishima S, Fujita N, Mano Y et al. Different roles of S100P overexpression in intrahepatic cholangiocarcinoma: carcinogenesis of perihilar type and aggressive behavior of peripheral type. Am J Surg Pathol 2011;35:590–598.
Kjellev S . The trefoil factor family—small peptides with multiple functionalities. Cell Mol Life Sci 2009;66:1350–1369.
Arumugam T, Brandt W, Ramachandran V et al. Trefoil factor 1 stimulates both pancreatic cancer and stellate cells and increases metastasis. Pancreas 2011;40:815–822.
Park SW, Zhen G, Verhaeghe C et al. The protein disulfide isomerase AGR2 is essential for production of intestinal mucus. Proc Natl Acad Sci USA 2009;106:6950–6955.
Riener MO, Pilarsky C, Gerhardt J et al. Prognostic significance of AGR2 in pancreatic ductal adenocarcinoma. Histol Histopathol 2009;24:1121–1128.
Gandou C, Harada K, Sato Y et al. Hilar cholangiocarcinoma and pancreatic ductal adenocarcinoma share similar histopathologies, immunophenotypes, and development-related molecules. Hum Pathol 2013;44:811–821.
Akiba J, Nakashima O, Hattori S et al. Clinicopathologic analysis of combined hepatocellular–cholangiocarcinoma according to the latest WHO classification. Am J Surg Pathol 2013;37:496–505.
Acknowledgements
This work was supported by Grant 100-2320-B-002-011-MY3 from the National Science Council, Taiwan, Republic of China, and Grant NTUH-102-S2060 from the National Taiwan University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liau, JY., Tsai, JH., Yuan, RH. et al. Morphological subclassification of intrahepatic cholangiocarcinoma: etiological, clinicopathological, and molecular features. Mod Pathol 27, 1163–1173 (2014). https://doi.org/10.1038/modpathol.2013.241
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.241
Keywords
This article is cited by
-
Prognostic implications of tumor histology and microenvironment in surgically resected intrahepatic cholangiocarcinoma: a single institutional experience
Virchows Archiv (2024)
-
Preoperative subcategorization based on magnetic resonance imaging in intrahepatic cholangiocarcinoma
Cancer Imaging (2023)
-
Integrative analysis of multiple genomic data from intrahepatic cholangiocarcinoma organoids enables tumor subtyping
Nature Communications (2023)
-
Asbestos exposure as an additional risk factor for small duct intrahepatic cholangiocarcinoma: a pilot study
Scientific Reports (2023)
-
Epigenetic upregulation of TET2 is an independent poor prognostic factor for intrahepatic cholangiocarcinoma
Virchows Archiv (2022)