Abstract
Primary B-cell lymphoma of the testis, breast and thyroid are rare and data concerning cytogenetic aberrations at these extranodal sites are scarce. We examined the presence of extranodal marginal zone lymphoma-associated translocations, t(11;18)(q21;q21), t(1;14)(p22;q32), t(14;18)(q32;q21), t(3;14)(p14.1;q32) and numerical aberrations of chromosomes 1, 3, 12 and 18 by fluorescence in situ hybridization in 6 extranodal marginal zone lymphomas and 24 diffuse large B-cell lymphomas with (n=9) or without (n=15) marginal zone lymphoma components, with primary localizations in the breast (n=15), testis (n=9) and thyroid (n=6). We found t(14;18)(q32;q21), with breakpoints in IGH and MALT1, in one testicular diffuse large B-cell lymphoma and in two diffuse large B-cell lymphomas of the breast. No other translocations, amplifications or deletions involving IGH, BCL-10, BCL-2, MALT1 and IAP2 were detected. Numerical aberrations occurred in 67% of the lymphomas, 67% of extranodal marginal zone lymphomas, 56% of diffuse large B-cell lymphomas with marginal zone lymphoma components and in 73% of ‘de novo’ diffuse large B-cell lymphomas. These included 78% of testis, 67% of thyroid and 60% of breast lymphomas, and included mainly trisomy 18 (n=16), trisomy 3 (n=8) and trisomy 1 (n=3). One testicular diffuse large B-cell lymphoma harbored both t(14;18)(q32;q21) and trisomy 3. Our results indicate that at least a few cases of diffuse large B-cell lymphoma of the testis and the breast belong to the spectrum of extranodal marginal zone lymphoma.
Similar content being viewed by others
Main
Primary B-cell lymphoma of the testis, breast and thyroid are rare, each accounting for between 0.5 and 2.5% of all non-Hodgkin’s lymphomas (NHLs).1, 2, 3, 4, 5, 6 Diffuse large B-cell lymphoma is the most common histological entity at these extranodal sites. Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue, commonly found in extranodal sites devoid of native lymphoid tissue, like the stomach, lung, salivary gland, thyroid and ocular adnexa, occur infrequently in the breast and testis. Although extranodal marginal zone lymphoma and diffuse large B-cell lymphoma are considered distinct clinicopathological entities in the World Health Organization (WHO) classification,7 many extranodal diffuse large B-cell lymphomas have derived from a background of extranodal marginal zone lymphoma.8, 9, 10, 11 We found that a large subgroup of primary testicular diffuse large B-cell lymphoma has marginal zone lymphoma components, including small cell components and lymphoepithelial lesions.12
Four mutually exclusive and apparently site-specific, chromosomal translocations have been implicated in the development and progression of extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue. These extranodal marginal zone lymphoma-associated translocations, t(11;18)(q21;q21),11, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 t(1;14)(p22;q32),13, 14, 23 t(14;18)(q32;q21)14, 15, 24, 25 and t(3;14)(p14.1;q32)26 show substantial differences in prevalence at specific extranodal localizations. In addition, several studies have reported the presence of various cytogenetic numerical aberrations, including trisomy 3, 7, 12 and 18, in extranodal marginal zone lymphoma at different extranodal sites.8, 15, 17, 27, 28, 29, 30, 31, 32, 33, 34, 35 One may wonder whether these extranodal marginal zone lymphoma-associated translocations and numerical aberrations occur in extranodal diffuse large B-cell lymphoma with marginal zone lymphoma components, which may belong to the extranodal marginal zone lymphoma spectrum.
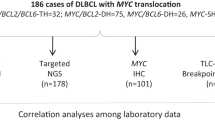
This study investigated for the presence of extranodal marginal zone lymphoma-associated translocations and numerical aberrations in diffuse large B-cell lymphoma with and without extranodal marginal zone lymphoma components and in extranodal marginal zone lymphoma of the breast, testis and thyroid, to test the hypothesis that also these lymphomas may belong to the spectrum of extranodal marginal zone lymphoma.
Materials and methods
Patients and Tissue Samples
Formalin-fixed paraffin-embedded tissue samples of biopsies or surgical resection specimens of 30 B-cell lymphoma cases of the thyroid (n=6), testis (n=9) and breast (n=15) were retrieved from the registries of the Comprehensive Cancer Centers South and West in the Netherlands. All cases were part of B-cell NHL series of three earlier publications,12, 36, 37 and these patients were diagnosed between January 1981 and January 1999.
Biopsies from 30 patients, including 6 extranodal marginal zone lymphoma and 24 diffuse large B-cell lymphoma cases, were available for this study. Nine diffuse large B-cell lymphomas harbored marginal zone lymphoma features, which we defined as a small cell component with or without lymphoepithelial lesions, and were classified as diffuse large B-cell lymphoma with marginal zone lymphoma component.
For the diagnosis of the thyroid, testicular or breast lymphoma an adequate tissue biopsy of this site was required. Haematoxylin and eosin sections were examined, and all cases were reclassified according the WHO classification.7 Prior immunophenotyping results were reviewed and, if necessary, additional staining was performed, including paraffin and frozen section immunohistochemistry. A variety of antibodies were used, including anti-CD3, CD5, CD10, CD20, CD45, CD79a, terminal deoxynucleotidyl transferase, cyclin D1 and anti-immunoglobulin heavy and light chains.
Fluorescence In Situ hybridization (FISH) Analysis
Sample preparation
Nuclei were isolated from the paraffin-embedded tissues as described previously.17 Briefly, 50-μm thick sections were de-waxed by xylene, disaggregated manually and digested with 0.1% protease in phosphate-buffered saline for 40 min at 37°C. To make the target DNA accessible to the probes, the nuclear suspension was spun onto slides and subsequently incubated in a solution of 1 mol/l NaSCN at 80°C for 30 min and in 0.1% pepsin (Sigma-Aldrich), pH 2.0 at 37°C for 5–30 min.
Probe selection
Differentially labeled sets of probes were selected for detection of breaks, amplifications or deletions in the selected chromosomal regions. For detection of t(11;18)(q21;q21), two YAC clones were pooled to enhance the signal, both spanning the IAP2 gene at 11q21 (YAC949B6 and YAC817C6) and the MALT1 gene at 18q21 (YAC906C5 and YAC892F3).29 For t(14;18)(q32;q21) detection, cosmid cosIg6 containing the IGH C3 gene and surrounding sequences of region 14q32, and YAC906C5 and YAC892F3 (for the MALT1 gene at 18q21) were used. For detection of t(1;14)(p22;q32) YAC 928EL spanning the BCL-10 gene at 1p22 and cosmid cosIg6 at 14q32 were chosen. For t(14;18)(q32;q21) involving IGH and BCL-2, we used LSI IGH and LSI BCL2 probes obtained from Vysis (Downers Gove, IL, USA). All YAC clones were obtained from Centre d’Étude du Polymorphisme Humain Paris, France. DOP-PCR products of cosmids and YAC clones were labeled either with biotin-11-dUTP or with digoxigenin-11-dUTP (Roche, Mannheim, Germany). For the detection of trisomies (peri-)centromeric repetitive α-satellite DNA probes specific for chromosomes 1, 3 (D3Z1, Oncor Gaithersburg, MD, USA), 12 (pα12H8) and 18 (L1.84) were selected.34 All probes were hybridized on metaphase spreads of lymphocytes to confirm chromosomal location and specificity.
FISH conditions and detection
FISH was performed as described previously.29 In short, the labeled DNA probes were diluted in hybridization mixture (50% formamide, 2 × standard saline citrate pH 7.0, 10% dextran sulfate (Pharmacia, Uppsala, Sweden), 0.2 μg/μl herring sperm DNA (Roche) and 10 μg/μl Cot1 DNA (Roche) to a final concentration of 20 μg/μl. A volume of 10 μl of hybridization mixture was added onto the slide; probe and target DNA were denatured for 8 min at 80°C. After overnight hybridization at 37°C, the slides were washed in 50% formamide/2 × SSC (2 × 10 min at 45°C) and 2 × 5 min in 0.1 × SSC/0.05% Tween-20 at 60°C. Probes were detected by fluorescein isothiocynate and Texas red isothiocynate-labeled antibodies as described previously.29 FISH conditions, washes and detection for LSI IGH/BCL2 probes were performed according to the manufacturer’s protocol (Vysis).
Normal controls
To determine the cutoff level in normal interphase nuclei, FISH was performed on cytospin preparations from eight reactive tonsils. At least 4 × 200 qualifying nuclei per slide were evaluated on a DMRB/E fluorescence microscope (Leica, Wetzlar, Germany). The cutoff levels were defined by the mean+3s.d. Only cases with a complete pattern of one separate red signal, two separate green signals and one co-localized or fused signal (1R2G1F) were considered consistent with t(1;14)(p22;q32) or t(14;18)(q32;q21), using the appropriate probe sets. Nuclei with an incomplete set of signals were omitted from the score. Signals were considered co-localized when their distance was equal to or smaller than the size of the hybridization signal. A pattern of 1R1G2F was indicative for the presence of t(11;18)(q21;q21). Criteria for trisomy detection were described previously.34 The cutoff levels determined for individual probe sets ranged from 2.1 to 2.7% for YAC and cosmid probes and between 5 and 7% for the various centromeric probes.
Results
We found t(14;18)(q32;q21), with breakpoints in IGH and MALT1, in three diffuse large B-cell lymphomas, including one testicular diffuse large B-cell lymphoma and two diffuse large B-cell lymphomas of the breast, one of which was a diffuse large B-cell lymphoma with marginal zone lymphoma component (Table 1). The t(14;18)(q32;q21)-positive lymphomas showed split signals for the MALT1 probe, confirming MALT1 involvement in the translocation, and co-localization to one IGH C region probe signal (Figure 1). Rearrangement of the IGH locus was confirmed by FISH with LSI IGH probes showing split signals, while the absence of IGH/BCL2 fusions pointed to a lack of BCL-2 involvement in the translocation. The number of nuclei with a translocation in t(14;18)(q32;q21)-bearing lymphomas ranged from 15 to 20%, well above the cutoff level of 2.1%. Other breaks, involving IGH, BCL-10, MALT1, BCL-2 and IAP2, amplification or deletion of chromosomal region 11q21, 18q21, 1p22 and 14q32, were not detected.
Fluorescence in situ hybridization (FISH) assay for detection of t(14;18)(q32;q21). (a) Illustrates the positions of the differentially labeled YAC and cosmid clones used as sets for detection of breaks t(14;18)(q32;q21) involving IG6/MALT1 or LSI IGH/ LSI BCL-2 Vysis (distances are not drawn to scale). (b) Probes were hybridized to normal metaphase lymphocyte nuclei (1) or interphase nuclei isolated from formalin-fixed paraffin-embedded tumor tissue (2, 3 and 4). 1 and 2 depict the signal pattern in translocation-negative nuclei. The translocation t(14;18)(q32;q21) results as a separate red (chromosome 14), two separate green signals (chromosome 18 and derivative chromosome 18) and one co-localized or fused red/green 1R2G1F (derivative chromosome 14) hybridized with IGH/MALT1 probes (3). LSI IGH and BCL-2 resulted in a 3G2R pattern in t(14;18)-positive lymphoma (4). Images were captured using quantix cooled CCD camera (Photometrics) attached to a DMRB/E fluorescence microscope (Leica) and IPlab Images acquire plus analysis software (IPlab) and were processed using Adobe Photoshop (version 5.5, Adobe Systems, CA, USA).
Numerical chromosomal aberrations occurred in 67% (4/6) of the extranodal marginal zone lymphomas, 73% (11/15) of the diffuse large B-cell lymphomas and 56% (5/9) of the diffuse large B-cell lymphomas with extranodal marginal zone lymphoma component (Table 2). Trisomy 18 was most commonly found (n=16), followed in decreasing order of frequency by trisomy 3 (n=8), trisomy 1 (n=3), trisomy 12 (n=1) and tetraploidy of chromosomes 18 (n=2) and 3 (n=1). Trisomies 3 and 18 were encountered in all three histological subtypes; trisomy 1 was exclusively found in diffuse large B-cell lymphomas with or without extranodal marginal zone lymphoma component, and trisomy 12 was found in one case of diffuse large B-cell lymphoma. Multiple chromosomal aberrations were more commonly found in testicular diffuse large B-cell lymphomas with and without extranodal marginal zone lymphoma component than in diffuse large B-cell lymphomas at other sites. One case, displaying three IAP2 probe signals, was confirmed with trisomy 11 using chromosome 11 specific centromeric probe (n=1). One t(14;18)(q32;q21)-positive testicular lymphoma in addition harbored trisomy 3.
Discussion
This is the first report showing the presence of an extranodal marginal zone lymphoma-associated translocation in diffuse large B-cell lymphomas of the breast and testis. Two of the three t(14;18)(q32;q21)-positive diffuse large B-cell lymphomas lacked extranodal marginal zone lymphoma components and this translocation might therefore not be specific for extranodal marginal zone lymphoma-associated lymphomas. Alternatively, lack of marginal zone lymphoma components is not proof of a ‘de novo’ diffuse large B-cell lymphoma, as the possibility of a marginal zone lymphoma component that is no longer apparent is more likely. We did not find any of the extranodal marginal zone lymphoma-associated translocations in extranodal marginal zone lymphoma of the breast and thyroid. Several studies have looked for extranodal marginal zone lymphoma-associated translocations in breast lymphomas.13, 14, 15, 27, 38, 39, 40 T(18q21), involving MALT1, has not been found in any of the 36 extranodal marginal zone lymphomas and 14 diffuse large B-cell lymphomas13, 14, 15, 27, 38, 39, 40 of the breast that have been reported to date. There are no reports of extranodal marginal zone lymphoma-associated translocations in testicular diffuse large B-cell lymphoma, as the presence of extranodal marginal zone lymphoma components in testicular diffuse large B-cell lymphoma has been described only recently.12 We did not find any structural aberrations in the thyroid lymphomas in our series. Other studies have confirmed the absence of t(14;18)(q32;q21) in thyroid lymphomas,13, 16, 27, 41 however, t(11;18) and t(3;14) have been reported in extranodal marginal zone lymphoma of the thyroid.14, 26, 32, 38 Several studies have confirmed differences in prevalence of extranodal marginal zone lymphoma-associated translocations at various anatomic sites and suggest that distinct molecular pathways are involved in the pathogenesis of extranodal marginal zone lymphoma.42, 43, 44
Interestingly, we found t(14;18)(q32;q21), a translocation previously reported to be associated with extranodal marginal zone lymphoma, in lymphomas, which were diagnosed as diffuse large B-cell lymphoma. One case had evidence of a concomitant extranodal marginal zone lymphoma component, but this component lacked in the other two t(14;18)(q32;q21)-positive cases. These two diffuse large B-cell lymphomas may have been derived from transformed t(14;18)(q32;q21)-positive extranodal marginal zone lymphomas in which all small lymphoid cells were overgrown by blasts after secondary tumor transformation. This hypothesis conflicts with data of previous research from our group on cutaneous extranodal marginal zone lymphoma that showed lack of blastic transformation in the cases that harbored the t(14;18)(q32;q21).29 Alternatively, t(14;18)(q32;q21) may also be present in ‘de novo’ diffuse large B-cell lymphoma, as previously reported in one case of cutaneous diffuse large B-cell lymphoma,45 and as was previously shown for another extranodal marginal zone lymphoma-associated translocation t(3;14)(p14.1;q32)) involving IGH or IGL and FOXP1.46, 47
We found breakpoints in the IGH JH region and noncoding region MALT1 or exon 1 MALT1, which is in agreement with previously reported data.25 By using an extensive panel of probes for all genes that have been associated with translocations in extranodal marginal zone lymphoma, we could exclude the presence of other extranodal marginal zone lymphoma-associated translocations, such as t(1;14)(p22;q32), t(11;18)(q21;q21), and in addition t(14;18)(q32;q21) involving IGH and BCL-2, which is characteristic of follicular lymphoma. Moreover, we did not detect t(3;14)(p14.1;q32)) involving IGH or IGL and FOXP1 found in extranodal marginal zone lymphoma and diffuse large B-cell lymphoma.26, 46, 47
We did not detect any new or recently described sporadic translocations, such as t(6;7)(q25;q11),48 t(X;14)(p11.4;q32),49 and translocations involving chromosomal regions on chromosome arms 1p, 1q, 5q and 9p.48 No loss or amplification of any of the studied regions was seen.
Similarly to other studies we found that trisomies 3 and 18 were the most common numerical aberrations in extranodal marginal zone lymphoma,14, 17, 24, 27, 31, 32, 35, 50, 51 and extranodal diffuse large B-cell lymphoma.33 We found a similar proportional distribution of the trisomies 18 and 3 in diffuse large B-cell lymphoma and extranodal marginal zone lymphoma at these extranodal sites. Patients with ‘de novo’ diffuse large B-cell lymphoma harbored more frequently two or more numerical aberrations compared with patients with extranodal marginal zone lymphoma and diffuse large B-cell lymphoma with extranodal marginal zone lymphoma component. One of our three cases with t(14;18)(q32;q21) had an additional trisomy 3.
In conclusion, our results indicate that t(14;18)(q32;q21) involving IGH-MALT1 is not restricted to extranodal marginal zone lymphoma but can occasionally be found in ‘de novo’ extranodal diffuse large B-cell lymphoma of the breast and testis. The presence of this translocation in a diffuse large B-cell lymphoma of the breast with extranodal marginal zone lymphoma features could indicate that at least some cases of diffuse large B-cell lymphoma of the breast may belong to the spectrum of extranodal marginal zone lymphoma.
References
Hasselblom S, Ridell B, Wedel H et al Testicular lymphoma—a retrospective, population-based, clinical and immunohistochemical study. Acta Oncol 2004;43:758–765.
Pedersen RK, Pedersen NT . Primary non-Hodgkin’s lymphoma of the thyroid gland: a population based study. Histopathology 1996;28:25–32.
Moller MB, d’Amore F, Christensen BE . Testicular lymphoma: a population-based study of incidence, clinicopathological correlations and prognosis. The Danish Lymphoma Study Group, LYFO. Eur J Cancer 1994;30A:1760–1764.
Hugh JC, Jackson FI, Hanson J et al Primary breast lymphoma. An immunohistologic study of 20 new cases. Cancer 1990;66:2602–2611.
Mizukami Y, Michigishi T, Nonomura A et al Primary lymphoma of the thyroid: a clinical, histological and immunohistochemical study of 20 cases. Histopathology 1990;17:201–209.
Freeman C, Berg JW, Cutler SJ . Occurrence and prognosis of extranodal lymphomas. Cancer 1972;29:252–260.
Swerdlow SH, Campo E, Harris NL et al World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Lyon, 2008, chapter 10 pp 214–233.
Barth TF, Bentz M, Dohner H et al Molecular aspects of B-cell lymphomas of the gastrointestinal tract. Clin Lymphoma 2001;2:57–64.
de Jong D, Boot H, van HP et al Histological grading in gastric lymphoma: pretreatment criteria and clinical relevance. Gastroenterology 1997;112:1466–1474.
Kuo SH, Yeh KH, Wu MS et al H. pylori eradication therapy is effective in the treatment of early-stage H. pylori-positive gastric diffuse large B-cell lymphomas. Blood 2012;119:4838–4844.
Huang X, Zhang Z, Liu H et al T(11;18)(q21;q21) in gastric MALT lymphoma and diffuse large B-cell lymphoma of Chinese patients. Hematol J 2003;4:342–345.
Kuper-Hommel MJ, Janssen-Heijnen ML, Vreugdenhil G et al Clinical and pathological features of testicular diffuse large B-cell lymphoma: a heterogeneous disease. Leuk Lymphoma 2011;53:242–246.
Sagaert X, Laurent M, Baens M et al MALT1 and BCL10 aberrations in MALT lymphomas and their effect on the expression of BCL10 in the tumour cells. Mod Pathol 2006;19:225–232.
Streubel B, Simonitsch-Klupp I, Mullauer L et al Variable frequencies of MALT lymphoma-associated genetic aberrations in MALT lymphomas of different sites. Leukemia 2004;18:1722–1726.
Murga Penas EM, Hinz K, Roser K et al Translocations t(11;18)(q21;q21) and t(14;18)(q32;q21) are the main chromosomal abnormalities involving MLT/MALT1 in MALT lymphomas. Leukemia 2003;17:2225–2229.
Ye H, Liu H, Attygalle A et al Variable frequencies of t(11;18)(q21;q21) in MALT lymphomas of different sites: significant association with CagA strains of H pylori in gastric MALT lymphoma. Blood 2003;102:1012–1018.
Schreuder MI, Hoeve MA, Hebeda KM et al Mutual exclusion of t(11;18)(q21;q21) and numerical chromosomal aberrations in the development of different types of primary gastric lymphomas. Br J Haematol 2003;123:590–599.
Remstein ED, James CD, Kurtin PJ . Incidence and subtype specificity of API2-MALT1 fusion translocations in extranodal, nodal, and splenic marginal zone lymphomas. Am J Pathol 2000;156:1183–1188.
Liu H, Ye H, Dogan A et al T(11;18)(q21;q21) is associated with advanced mucosa-associated lymphoid tissue lymphoma that expresses nuclear BCL10. Blood 2001;98:1182–1187.
Maes B, Baens M, Marynen P et al The product of the t(11;18), an API2-MLT fusion, is an almost exclusive finding in marginal zone cell lymphoma of extranodal MALT-type. Ann Oncol 2000;11:521–526.
Dierlamm J, Baens M, Stefanova-Ouzounova M et al Detection of t(11;18)(q21;q21) by interphase fluorescence in situ hybridization using API2 and MLT specific probes. Blood 2000;96:2215–2218.
Auer IA, Gascoyne RD, Connors JM et al t(11;18)(q21;q21) is the most common translocation in MALT lymphomas. Ann Oncol 1997;8:979–985.
Du MQ, Peng H, Liu H et al BCL10 gene mutation in lymphoma. Blood 2000;95:3885–3890.
Streubel B, Lamprecht A, Dierlamm J et al T(14;18)(q32;q21) involving IGH and MALT1 is a frequent chromosomal aberration in MALT lymphoma. Blood 2003;101:2335–2339.
Sanchez-Izquierdo D, Buchonnet G, Siebert R et al MALT1 is deregulated by both chromosomal translocation and amplification in B-cell non-Hodgkin lymphoma. Blood 2003;101:4539–4546.
Streubel B, Vinatzer U, Lamprecht A et al T(3;14)(p14.1;q32) involving IGH and FOXP1 is a novel recurrent chromosomal aberration in MALT lymphoma. Leukemia 2005;19:652–658.
Joao C, Farinha P, da Silva MG et al Cytogenetic abnormalities in MALT lymphomas and their precursor lesions from different organs. A fluorescence in situ hybridization (FISH) study. Histopathology 2007;50:217–224.
Remstein ED, Dogan A, Einerson RR et al The incidence and anatomic site specificity of chromosomal translocations in primary extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) in North America. Am J Surg Pathol 2006;30:1546–1553.
Schreuder MI, Hoefnagel JJ, Jansen PM et al FISH analysis of MALT lymphoma-specific translocations and aneuploidy in primary cutaneous marginal zone lymphoma. J Pathol 2005;205:302–310.
Streubel B, Huber D, Wohrer S et al Frequency of chromosomal aberrations involving MALT1 in mucosa-associated lymphoid tissue lymphoma in patients with Sjogren’s syndrome. Clin Cancer Res 2004;10:476–480.
Remstein ED, Kurtin PJ, Einerson RR et al Primary pulmonary MALT lymphomas show frequent and heterogeneous cytogenetic abnormalities, including aneuploidy and translocations involving API2 and MALT1 and IGH and MALT1. Leukemia 2004;18:156–160.
Remstein ED, Kurtin PJ, James CD et al Mucosa-associated lymphoid tissue lymphomas with t(11;18)(q21;q21) and mucosa-associated lymphoid tissue lymphomas with aneuploidy develop along different pathogenetic pathways. Am J Pathol 2002;161:63–71.
Starostik P, Patzner J, Greiner A et al Gastric marginal zone B-cell lymphomas of MALT type develop along 2 distinct pathogenetic pathways. Blood 2002;99:3–9.
Hoeve MA, Gisbertz IA, Schouten HC et al Gastric low-grade MALT lymphoma, high-grade MALT lymphoma and diffuse large B cell lymphoma show different frequencies of trisomy. Leukemia 1999;13:799–807.
Brynes RK, Almaguer PD, Leathery KE et al Numerical cytogenetic abnormalities of chromosomes 3, 7, and 12 in marginal zone B-cell lymphomas. Mod Pathol 1996;9:995–1000.
Kuper-Hommel MJ, Snijder S, Janssen-Heijnen ML et al Treatment and survival of 38 female breast lymphomas: a population-based study with clinical and pathological reviews. Ann Hematol 2003;82:397–404.
Kuper-Hommel MJ, Snijder S, Jansen-Heijnen ML et al Treatment and survival of patients with thyroid lymphoma: a population-based study with clinical and pathologic reviews. Clin Lymphoma Myeloma 2005;6:240–247.
Mulligan S, Hu P, Murphy A et al Variations in MALT1 gene disruptions detected by FISH in 109 MALT lymphomas occurring in different primary sites. J Assoc Genet Technol 2011;37:76–79.
Talwalkar SS, Valbuena JR, Abruzzo LV et al MALT1 gene rearrangements and NF-kappaB activation involving p65 and p50 are absent or rare in primary MALT lymphomas of the breast. Mod Pathol 2006;19:1402–1408.
Raderer M, Streubel B, Woehrer S et al High relapse rate in patients with MALT lymphoma warrants lifelong follow-up. Clin Cancer Res 2005;11:3349–3352.
Ye H, Gong L, Liu H et al MALT lymphoma with t(14;18)(q32;q21)/IGH-MALT1 is characterized by strong cytoplasmic MALT1 and BCL10 expression. J Pathol 2005;205:293–301.
Du MQ . MALT lymphoma: many roads lead to nuclear factor-kappab activation. Histopathology 2011;58:26–38.
Kuper-Hommel MJ, van Krieken JH . Molecular pathogenesis and histologic and clinical features of extranodal marginal zone lymphomas of mucosa-associated lymphoid tissue type. Leuk Lymphoma 2012;53:1032–1045.
Jost PJ, Ruland J . Aberrant NF-kappaB signaling in lymphoma: mechanisms, consequences, and therapeutic implications. Blood 2007;109:2700–2707.
Cook JR, Sherer M, Craig FE et al T(14;18)(q32;q21) involving MALT1 and IGH genes in an extranodal diffuse large B-cell lymphoma. Hum Pathol 2003;34:1212–1215.
Wlodarska I, Veyt E, De PP et al FOXP1, a gene highly expressed in a subset of diffuse large B-cell lymphoma, is recurrently targeted by genomic aberrations. Leukemia 2005;19:1299–1305.
Fenton JA, Schuuring E, Barrans SL et al t(3;14)(p14;q32) results in aberrant expression of FOXP1 in a case of diffuse large B-cell lymphoma. Genes Chromosomes Cancer 2006;45:164–168.
Vinatzer U, Gollinger M, Mullauer L et al Mucosa-associated lymphoid tissue lymphoma: novel translocations including rearrangements of ODZ2, JMJD2C, and CNN3. Clin Cancer Res 2008;14:6426–6431.
Novak A, Akasaka T, Manske M et al Elevated expression of GPR34 and its association with a novel translocation T(X;14)(p11;q32) involving IgHS and GPR34 in MALT lymphoma. ASH Annual Meeting Abstracts. Blood 2008;112 abstract 2251.
Wotherspoon AC, Finn TM, Isaacson PG . Trisomy 3 in low-grade B-cell lymphomas of mucosa-associated lymphoid tissue. Blood 1995;85:2000–2004.
Dierlamm J, Pittaluga S, Wlodarska I et al Marginal zone B-cell lymphomas of different sites share similar cytogenetic and morphologic features. Blood 1996;87:299–307.
Acknowledgements
We thank all hospitals and their clinicians participating in the registries of the Comprehensive Cancer Centres South and West for providing access to histological slides and blocks and medical records.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kuper-Hommel, M., Schreuder, M., Gemmink, A. et al. T(14;18)(q32;q21) involving MALT1 and IGH genes occurs in extranodal diffuse large B-cell lymphomas of the breast and testis. Mod Pathol 26, 421–427 (2013). https://doi.org/10.1038/modpathol.2012.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.170
Keywords
This article is cited by
-
Radiation therapy for primary breast lymphoma in male gynecomastia: a rare case report and review of the literature
International Journal of Hematology (2016)