Abstract
Previous studies have demonstrated that androgen receptor is expressed in many breast cancers, but its expression in relation to the various breast cancer subtypes as defined by molecular profiling has not been studied in detail. We constructed tissue microarrays from 3093 breast cancers that developed in women enrolled in the Nurses' Health Study. Tissue microarray sections were immunostained for estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), cytokeratin 5/6, epidermal growth factor receptor (EGFR) and androgen receptor (ER). Immunostain results were used to categorize each cancer as luminal A or B, HER2 and basal like. The relationships between androgen receptor expression and molecular subtype were analyzed. Overall, 77% of the invasive breast carcinomas were androgen receptor positive. Among 2171 invasive cancers, 64% were luminal A, 15% luminal B, 6% HER2 and 11% basal like. The frequency of androgen receptor expression varied significantly across the molecular phenotypes (P<0.0001). In particular, androgen receptor expression was commonly observed in luminal A (91%) and B (68%) cancers, but was less frequently seen in HER2 cancers (59%). Despite being defined by the absence of ER and PR expression and being considered hormonally unresponsive, 32% of basal-like cancers expressed androgen receptor. Among 246 cases of ductal carcinoma in situ, 86% were androgen receptor positive, but the frequency of androgen receptor expression differed significantly across the molecular phenotypes (P=0.001), and high nuclear grade lesions were less likely to be androgen receptor positive compared with lower-grade lesions. Androgen receptor expression is most commonly seen in luminal A and B invasive breast cancers. However, expression of androgen receptor is also seen in approximately one-third of basal-like cancers, providing further evidence that basal-like cancers represent a heterogeneous group. Our findings raise the possibility that targeting the androgen receptor pathway may represent a novel therapeutic approach to the management of patients with basal-like cancers.
Similar content being viewed by others
Main
Recent gene expression profiling studies using microarrays and unsupervised cluster analysis have provided new insights into the classification of invasive breast cancers.1, 2, 3, 4 The breast cancer subgroups that have been the most reproducibly identified by these studies are luminal subtypes A and B, both of which are estrogen receptor (ER) positive and/or progesterone receptor (PR) positive; the human epidermal growth factor receptor 2 (HER2) subtype; and the basal-like group.1, 2, 3, 4 The clinical relevance of these molecular subgroups is supported by studies that have demonstrated differences in outcome and response to various adjuvant and neoadjuvant therapies according to molecular subtype.3, 4, 5, 6 Furthermore, molecular profiling has verified that expression of ER, PR and related genes is the major determinant in the subclassification of breast cancers.
ER is known to play an important role in endocrine-mediated tumor development and has been shown to influence breast cancer development and progression.7 Although ER and PR have been studied extensively, relatively little is known about the role of androgens and androgen receptor in breast cancer. Previous studies have shown that androgen receptor is expressed in 60–85% of breast cancers, and in some cases it is more highly expressed than ER or PR.8, 9, 10, 11, 12, 13 Additionally, epidemiologic studies have found that high circulating androgen levels are associated with an increased risk of developing breast cancer, particularly among postmenopausal women.14, 15, 16, 17, 18 The biologic roles of androgens in the breast are incompletely understood, as it is unclear whether the effects of androgens on breast cells are predominantly proliferative or antiproliferative. Recently, the effect of androgens on breast cancer cell lines and the potential role of the androgen receptor pathway in breast cancer have been explored.19, 20, 21 Results suggest a possible antiproliferative effect of androgen receptor stimulation and pathway activation in breast cancer.19, 20, 21
There has been recent interest in evaluating the expression of androgen receptor among the molecularly defined categories of invasive breast cancer, particularly among the triple-negative (or basal like) and the HER2 groups that are considered to be hormone receptor negative.11, 22, 23 However, large population-based studies investigating expression of androgen receptor in relation to molecular phenotype or among women with ductal carcinoma in situ are lacking. Therefore, the objective of this study was to examine the expression of androgen receptor in relation to tumor stage, pathologic features and molecular phenotype using a large, well-characterized population of women with breast cancer.
Materials and methods
Study Population
Study design and population
The Nurses' Health Study was initiated in 1976, when 121 700 US registered nurses aged 30–55 years returned an initial questionnaire. The cohort has been followed by mailed questionnaires biennially to update exposure information and ascertain nonfatal incident diseases. Information on body mass index, reproductive history, age at menopause and postmenopausal hormone use as well as diagnosis of cancer and other diseases are updated every 2 years through questionnaires. The follow-up rate among this cohort was over 90% through 1996.
Breast Cancer Case Confirmation
All women reporting incident diagnoses of cancer were asked for permission to review their medical records to confirm the diagnosis and to classify cancers as in situ or invasive, by histologic type, size and presence or absence of metastases. To identify cases of cancer in nonrespondents who died, death certificates for all deceased participants and medical records for the incident cancers were obtained. Following medical record review, 99% of self-reported breast cancers were confirmed.
Breast Cancer Tissue Block Collection
In 1993, we began collecting archived formalin-fixed paraffin-embedded breast cancer blocks for participants with primary incident breast cancers over 20 years of follow-up (1976–1996). Cases who reported a prevalent cancer including breast cancer at baseline were excluded from collection. Of the 5610 breast cancers that were eligible for block collection, we were unable to obtain any pathology material for 1858 cases. The primary reason was because they had been destroyed by the hospital (45%). Because the majority of hospitals archive tissue blocks for only 5–10 years, we were more successful in obtaining more recent blocks. Because year of diagnosis and age at diagnosis are highly correlated (Spearman's correlation=0.49; P<0.0001), the temporal effect on our collections is evident not only in the differences in age at diagnosis, but also in the frequency of premenopausal breast cancers when comparing the women from whom we obtained specimens with those for whom we did not. However, these two groups of women were very similar regarding a number of other breast cancer risk factors and tumor characteristics (data published previously24). After taking into account the age and year of diagnosis, the participants whose tumors were included in the tissue microarrays were very similar to those for whom we were unable to obtain tissue blocks.
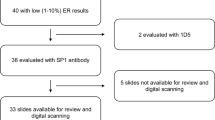
We obtained pathology material for 3752 participants. Of these, 390 specimens were hematoxylin and eosin (H&E)-stained slides only and 45 tissue blocks had to be returned to the lending hospital before construction of the tissue microarrays and thus could not be included. H&E sections of the corresponding 3317 paraffin-embedded tissue blocks were reviewed by a single pathologist to confirm the cancer diagnosis, classify the cancer according to histologic type and grade (Nottingham), and circle the area from which the cores for the tissue microarrays would be taken. Pathology review identified 420 tumor blocks as unusable for tissue microarray construction. The majority of exclusions were because the block did not contain residual tumor (60%) or there was insufficient tumor for the tissue microarrays (26%). Tissue microarrays were constructed in the Dana Farber Harvard Cancer Center Tissue Microarray Core Facility (Boston, MA). From each breast cancer, three 0.6-mm cores were obtained and inserted into the recipient tissue microarray blocks. In total, 23 tissue microarray blocks were constructed from 3093 cancers and positive lymph nodes from 2897 participants. We excluded from the current analysis participants with positive lymph nodes only (n=25), rare tumor types including malignant phyllodes tumors, neuroendocrine carcinoma and angiosarcoma (n=10), lobular carcinoma in situ (n=31), in situ carcinomas with both ductal and lobular features (n=13) and missing information on androgen receptor status (n=287). Among 2258 invasive breast cancers and 273 women with ductal carcinoma in situ with androgen receptor data, 2171 and 246 women also had complete information on immunophenotype, respectively.
Immunohistochemical Analysis
We performed immunohistochemical staining for ER-α, PR, HER2, cytokeratin (CK)5/6, and epidermal growth factor receptor (EGFR) on 5-μm paraffin sections cut from the tissue microarray blocks. Immunostains for each marker were performed in a single staining run on a Dako Autostainer (Dako Corporation, Carpinteria, CA, USA). These particular biomarkers were selected for analysis because they have been commonly used as a surrogate to classify invasive breast cancers according to their molecular phenotypes.4, 25, 26, 27, 28 The sources and dilutions of the primary antibodies used in this study are listed in Table 1. The immunostaining protocols for ER, PR, HER2, CK5/6 and EGFR have been previously described in detail.24 Immunostaining for androgen receptor was performed on tissue sections following deparaffinization in two 5-min changes of xylene and rehydration through graded alcohols to distilled water. After blocking endogenous peroxidase activity, sections were subjected to heat-induced epitope retrieval by heating in a vegetable steamer in citrate buffer (pH 6.1) for 20 min. Following heat-induced epitope retrieval, the primary monoclonal antibody AR441 (DAKO) was applied to the sections in a dilution of 1:200 and the slides were incubated at room temperature for 30 min followed by incubation with the biotinylated universal secondary antibody and the avidin-biotin complex. Visualization was performed with liquid DAB as the chromogen-substrate. Tissue sections from samples of prostate carcinoma were used as both positive and negative controls and were included in all staining runs.
Immunostained tissue microarray slides were evaluated for ER, PR and androgen receptor expression, HER2 protein overexpression, and expression of CK5/6 and EGFR in each core. Tumor cells that showed nuclear staining for ER, PR or androgen receptor were considered ER positive, PR positive or androgen receptor positive, respectively, whereas all ER-negative, PR-negative and androgen receptor-negative cases showed complete absence of tumor cell staining in all three tissue cores. Of note, low positive ER, PR or androgen receptor (1–10% of tumor cell nuclei staining) and positive ER, PR or androgen receptor (>10% of tumor cell nuclei staining) were collapsed into a single ER, PR or androgen receptor ‘positive’ category for the purposes of this analysis. Tumor cells were considered positive for HER2 protein overexpression when >10% of the cells showed moderate or strong membrane staining (2+ and 3+). The results of analyses in which HER2 positivity was defined as 3+ were very similar to those with a definition of 2+ and 3+.24 Cases were considered basal CK positive or EGFR positive if any cytoplasmic and/or membranous staining was detected in the tumor cells, even if focal. These latter criteria are similar to those previously used for scoring these markers in invasive basal-like cancers.4, 25, 26
Classification of Molecular Phenotype
Immunostained tissue microarray sections were reviewed under a microscope and visually scored for each individual tissue core as described above. We classified a case as positive if there was staining in any of the three cores from that case and negative if there was no immunostaining present. Cases that were ER positive and/or PR positive, HER2 negative and histologic grade 1 or 2 were classified as luminal A cancers; cases that were ER positive and/or PR positive and HER2 positive or ER positive and/or PR positive and HER2 negative but histologic grade 3 were classified as luminal B cancers; cases that were ER negative, PR negative and HER2 positive were classified as HER2 type; and cases that were negative for ER, PR and HER2 and positive for CK5/6 and/or EGFR were categorized as basal like. Cases that lacked expression of all five markers were considered ‘unclassified’.
Statistical Analysis
The χ2 tests were used to evaluate the independence of selected variables under the null hypothesis. All statistical tests were two sided and P-values <0.05 were considered statistically significant.
Results
The population for this analysis consisted of breast cancers that developed in women in the Nurses' Health Study after the baseline questionnaire (1976) through the 1996 follow-up cycle that could be classified into one of the four molecular phenotypes and that had evaluable androgen receptor-stained tissue microarray cores (2171 invasive cancers; 246 DCIS). Based on immunostaining data for the five markers used (ER, PR, HER2, EGFR and CK5/6), 1380 invasive tumors were classified as luminal A (64%); 326 were luminal B (15%); 126 were HER2 (6%); and 237 were basal like (11%). There were also 102 invasive tumors that were considered unclassifiable (ER–/PR–/HER2–/EGFR–/CK5/6–) for which androgen receptor staining was available (Table 2).
Overall, 77% of the invasive cancers were androgen receptor positive. The frequency of androgen receptor expression varied significantly across the molecular phenotypes (P<0.0001). In particular, androgen receptor expression was present in 91% of luminal A cancers, 68% of luminal B cancers and 59% of HER2-type cancers. Of note, despite their being defined by the absence of ER and PR expression and being considered hormonally unresponsive, 32% of basal-like cancers showed expression of androgen receptor. Also, 46% of the unclassified cases expressed androgen receptor.
There were 246 cases of ductal carcinoma in situ with complete immunophenotypic data: 50% were luminal A, 28% luminal B, 13% HER2, 7% basal like and 2% unclassified. Overall, 86% of ductal carcinoma in situ cases were androgen receptor positive, but the frequency of androgen receptor expression differed significantly across the molecular phenotypes (P=0.001). Androgen receptor expression was commonly observed in ductal carcinoma in situ with luminal A and luminal B phenotypes (93 and 84% of cases, respectively), but was less frequently seen in the HER2 subtype (78% of cases). Again, despite their being defined by absence of ER and PR expression, 71% of basal-like ductal carcinoma in situ showed expression of androgen receptor.
The frequency of androgen receptor according to histologic type of invasive cancer is shown in Figure 1. Androgen receptor expression was seen in most types, including 71.0% of invasive ductal carcinomas, 96.3% of invasive lobular carcinomas, 80.5% of mucinous carcinomas and 100% of tubular carcinomas. Overall, androgen receptor-positive tumors at presentation were smaller (P<0.0001), more often node negative (P=0.003), lower grade (P<0.0001) and lower stage than androgen receptor-negative tumors (P=0.001; Table 3). Among ductal carcinoma in situ cases, high nuclear grade lesions were less likely to be androgen receptor positive compared with low- or intermediate-grade lesions (Table 4).
Discussion
In this large population-based study, 77% of invasive breast cancers were androgen receptor positive. The frequency of androgen receptor expression among breast cancers in this series is similar to that reported in previous smaller studies that also used immunohistochemical methods for androgen receptor detection (range 74.8–80%).8, 9, 10, 11, 12, 13 As reported in previous studies, we found that the majority of ER-positive tumors also express androgen receptor. Of interest, we also found that androgen receptor expression was frequent even in molecular subtypes of invasive cancer that are ER negative. Specifically, we found androgen receptor expression in 59% of cancers in the HER2 group, 32% of those in the basal-like group and in 46% of unclassified carcinomas (those that were ER, PR, HER2, CK5/6 and EGFR negative). Results from a recent publication by Niemeier et al11 found a similarly high proportion of HER2-type breast cancers to coexpress androgen receptor (5/8 cases, 63%), although it should be noted that these authors utilized a different classification system for the luminal B group than we did and that resulted in all HER2-positive cancers being classified as HER2 type. In that study, only 10% (3/30) of triple-negative breast cancer cases coexpressed androgen receptor, compared with 32% (75/237) in this study.
The effects of androgens on the breast are still incompletely understood. Evidence suggests that estrogens and androgens have opposing effects and that androgens may play a protective role with regard to breast tumor development.29 In support of this argument, we, like others, found that androgen receptor-negative tumors were more likely to be larger in size, higher grade, and have more extensive lymph node involvement.11, 12, 13, 22, 30 Moreover, androgen receptor expression has been shown to be an independent prognostic factor for better outcome, even among women with ER-positive breast cancers.30, 31
Although androgens and androgen receptor and the association with breast cancer have been studied previously, their potential role in the development of breast cancer remains inconclusive.14, 15, 16, 17, 18, 32, 33 Hanley et al34 investigated the potential role of androgen receptor in relation to breast tumor progression and showed that 93% of 43 high-grade ductal carcinoma in situ cases expressed androgen receptor, whereas only 55% of 44 high-grade invasive ductal carcinomas showed androgen receptor expression. The authors argue that this may suggest a role for androgen receptor in progression to invasion in high-grade breast carcinomas. A study by Meijnen et al35 also evaluated the expression of androgen receptor in 163 cases of ductal carcinoma in situ. In that study, androgen receptor expression was seen in 36, 51 and 26% of cases of low-, intermediate- and high-grade ductal carcinoma in situ, a distribution similar to that seen in this study. Paradoxically, a higher cutoff of 10% nuclear staining was used to define androgen receptor positivity in both previous studies that would not account for the higher proportion of positive cases in the Hanley series.34, 35 Further work is needed to define a role for androgen receptor in the transformation of in situ to invasive carcinoma.
In this study, androgen receptor expression was observed in each of the molecularly defined phenotypes of invasive breast cancer, although the proportion of cases showing androgen receptor expression was highest in the luminal subtypes. Furthermore, approximately one-third of basal-like cancers, which are defined by the absence of ER and PR expression and are considered to be hormonally unresponsive, showed expression of androgen receptor. This finding raises the possibility that targeting the androgen receptor pathway may represent a novel therapeutic approach to the management of patients with androgen receptor-positive basal-like cancers.36 In addition, almost 60% of invasive cancers in the HER2-type molecular group (also characterized by lack of ER and PR expression) showed expression of androgen receptor. Given experimental data that have shown cross-talk between androgen receptor and ERBB2 pathways in ER-negative breast cancer cell lines,37 combining androgen receptor antagonists with drugs that block the HER2 pathway may provide an additional therapeutic strategy for patients with ER-negative, HER2-positive breast cancers that express androgen receptor.
The role of androgen receptor-targeted therapy in ER-negative breast cancers has been explored in experimental models.19, 20, 38 For example, Garreau et al38 used dehydroepiandrosterone sulfate (DHEA-S) and an aromatase inhibitor to treat an ER/PR/androgen receptor-negative breast cancer cell line transfected with androgen receptor and were able to demonstrate cell death with that treatment. The results of that experiment and others like it19, 20, 21 suggest that androgen receptor is responsible for this effect and validates the concept that ER/PR-negative breast cancers may respond to appropriate hormonal therapy provided that they are androgen receptor positive.19, 38 Of interest, androgen receptor antagonists, such as DHEA-S, have the opposite effect in ER-positive, androgen receptor-positive cell lines in which proliferation is induced.20 Thus, it would appear that in the presence of both ER and androgen receptor, the estrogenic effect of DHEA-S predominates.20 It should be emphasized that to fully exploit the growth inhibitory effects of DHEA-S on the androgen receptor pathway, it appears to be necessary to coadminister an aromatase inhibitor to prevent conversion of DHEA-S to estrogen and other hormones by aromatase.19, 38
Our study has several potential limitations. First, we were unable to obtain tissue blocks from all breast cancers arising in this cohort. Our success in doing so was highly correlated with time between diagnosis and initiation of our tissue block collection. After taking into account the effect of age and year of diagnosis, the women for whom we were able to obtain tumor specimens were very similar to those for whom we were unable to obtain specimens (for expanded discussion, see Tamimi et al24). Moreover, the frequency of androgen receptor positivity among invasive tumors was very similar to that observed in other populations, which suggests that samples included in this study are representative of the overall US population. Second, we utilized immunohistochemical markers as a surrogate to classify breast cancers into the molecular phenotypes defined by expression profiling. Although the antibody panel that we used in this study has been shown to be a reliable proxy for classification of invasive breast cancers categorized by gene expression,4, 25, 26, 27, 28 the correlation is not perfect and there will be some misclassification of these phenotypes. The categories as defined by the immunohistochemical markers have been shown to be associated with prognostic markers and survival consistent with what has been seen with classification based on RNA expression assays, suggesting that both methods are capturing distinct subgroups.1, 2, 39, 40, 41 More recently, it has been shown that the distinction between luminal A and B tumors can be refined by adding the proliferation marker Ki67 to ER, PR and HER2.42 As Ki67 data were not available for our cases, we used histologic grade as a surrogate for proliferation rate, given the close correlation between proliferation rate and histologic grade. Thus, our definitions for luminal A and B are different from those used in our previous studies, but more in keeping with the most recently proposed classification scheme.42
In summary, in this large population-based study, androgen receptor expression was commonly seen in luminal A and B types of invasive breast cancer. Furthermore, expression of androgen receptor was also seen in a subset of HER2-type and basal-like cancers that are considered to be hormone receptor-negative breast cancers. The role of androgen receptor in the development and progression of invasive breast cancers merits further investigation. The potential for targeting the androgen signaling pathway in breast cancers defined by lack of expression of ER and PR raises the possibility of new therapeutic options for some patients with tumors previously considered to be hormone independent.
References
Perou CM, Jeffrey SS, van de Rijn M, et al. Distinctive gene expression patterns in human mammary epithelial cells and breast cancers. Proc Natl Acad Sci USA 1999;96:9212–9217.
Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 2001;98:10869–10874.
Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 2003;100:8418–8423.
Brenton JD, Carey LA, Ahmed AA, et al. Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol 2005;23:7350–7360.
Millar EK, Graham PH, O′Toole SA, et al. Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol 2009;27:4701–4708.
Hugh J, Hanson J, Cheang MC, et al. Breast cancer subtypes and response to docetaxel in node-positive breast cancer: use of an immunohistochemical definition in the BCIRG 001 trial. J Clin Oncol 2009;27:1168–1176.
Althuis MD, Fergenbaum JH, Garcia-Closas M, et al. Etiology of hormone receptor-defined breast cancer: a systematic review of the literature. Cancer Epidemiol Biomarkers Prev 2004;13:1558–1568.
Gonzalez LO, Corte MD, Vazquez J, et al. Androgen receptor expression in breast cancer: relationship with clinicopathological characteristics of the tumors, prognosis, and expression of metalloproteases and their inhibitors. BMC Cancer 2008;8:149.
Isola JJ . Immunohistochemical demonstration of androgen receptor in breast cancer and its relationship to other prognostic factors. J Pathol 1993;170:31–35.
Kuenen-Boumeester V, Van der Kwast TH, van Putten WL, et al. Immunohistochemical determination of androgen receptors in relation to oestrogen and progesterone receptors in female breast cancer. Int J Cancer 1992;52:581–584.
Niemeier LA, Dabbs DJ, Beriwal S, et al. Androgen receptor in breast cancer: expression in estrogen receptor-positive tumors and in estrogen receptor-negative tumors with apocrine differentiation. Mod Pathol 2010;23:205–212.
Moinfar F, Okcu M, Tsybrovskyy O, et al. Androgen receptors frequently are expressed in breast carcinomas: potential relevance to new therapeutic strategies. Cancer 2003;98:703–711.
Ogawa Y, Hai E, Matsumoto K, et al. Androgen receptor expression in breast cancer: relationship with clinicopathological factors and biomarkers. Int J Clin Oncol 2008;13:431–435.
Baglietto L, Severi G, English DR, et al. Circulating steroid hormone levels and risk of breast cancer for postmenopausal women. Cancer Epidemiol Biomarkers Prev 2010;19:492–502.
Kaaks R, Berrino F, Key T, et al. Serum sex steroids in premenopausal women and breast cancer risk within the European Prospective Investigation into Cancer and Nutrition (EPIC). J Natl Cancer Inst 2005;97:755–765.
Lillie EO, Bernstein L, Ursin G . The role of androgens and polymorphisms in the androgen receptor in the epidemiology of breast cancer. Breast Cancer Res 2003;5:164–173.
Sieri S, Krogh V, Bolelli G, et al. Sex hormone levels, breast cancer risk, and cancer receptor status in postmenopausal women: the ORDET cohort. Cancer Epidemiol Biomarkers Prev 2009;18:169–176.
Missmer SA, Eliassen AH, Barbieri RL, et al. Endogenous estrogen, androgen, and progesterone concentrations and breast cancer risk among postmenopausal women. J Natl Cancer Inst 2004;96:1856–1865.
Hardin C, Pommier R, Calhoun K, et al. A new hormonal therapy for estrogen receptor-negative breast cancer. World J Surg 2007;31:1041–1046.
Toth-Fejel S, Cheek J, Calhoun K, et al. Estrogen and androgen receptors as comediators of breast cancer cell proliferation: providing a new therapeutic tool. Arch Surg 2004;139:50–54.
Macedo LF, Guo Z, Tilghman SL, et al. Role of androgens on MCF-7 breast cancer cell growth and on the inhibitory effect of letrozole. Cancer Res 2006;66:7775–7782.
Rakha EA, El-Sayed ME, Green AR, et al. Prognostic markers in triple-negative breast cancer. Cancer 2007;109:25–32.
Farmer P, Bonnefoi H, Becette V, et al. Identification of molecular apocrine breast tumours by microarray analysis. Oncogene 2005;24:4660–4671.
Tamimi RM, Baer HJ, Marotti J, et al. Comparison of molecular phenotypes of ductal carcinoma in situ and invasive breast cancer. Breast Cancer Res 2008;10:R67.
Nielsen TO, Hsu FD, Jensen K, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 2004;10:5367–5374.
Abd El-Rehim DM, Ball G, Pinder SE, et al. High-throughput protein expression analysis using tissue microarray technology of a large well-characterised series identifies biologically distinct classes of breast cancer confirming recent cDNA expression analyses. Int J Cancer 2005;116:340–350.
Abd El-Rehim DM, Pinder SE, Paish CE, et al. Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 2004;203:661–671.
van de Rijn M, Perou CM, Tibshirani R, et al. Expression of cytokeratins 17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol 2002;161:1991–1996.
Labrie F, Luu-The V, Labrie C, et al. Endocrine and intracrine sources of androgens in women: inhibition of breast cancer and other roles of androgens and their precursor dehydroepiandrosterone. Endocr Rev 2003;24:152–182.
Castellano I, Allia E, Accortanzo V, et al. Androgen receptor expression is a significant prognostic factor in estrogen receptor positive breast cancers. Breast Cancer Res Treat 2010;124:607–617.
Agoff SN, Swanson PE, Linden H, et al. Androgen receptor expression in estrogen receptor-negative breast cancer. Immunohistochemical, clinical, and prognostic associations. Am J Clin Pathol 2003;120:725–731.
Key T, Appleby P, Barnes I, et al. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 2002;94:606–616.
Wysowski DK, Comstock GW, Helsing KJ, et al. Sex hormone levels in serum in relation to the development of breast cancer. Am J Epidemiol 1987;125:791–799.
Hanley K, Wang J, Bourne P, et al. Lack of expression of androgen receptor may play a critical role in transformation from in situ to invasive basal subtype of high-grade ductal carcinoma of the breast. Hum Pathol 2008;39:386–392.
Meijnen P, Peterse JL, Antonini N, et al. Immunohistochemical categorisation of ductal carcinoma in situ of the breast. Br J Cancer 2008;98:137–142.
Gucalp A, Traina TA . Triple-negative breast cancer: role of the androgen receptor. Cancer J 2010;16:62–65.
Naderi A, Hughes-Davies L . A functionally significant cross-talk between androgen receptor and ErbB2 pathways in estrogen receptor negative breast cancer. Neoplasia 2008;10:542–548.
Garreau JR, Muller P, Pommier R, et al. Transgenic introduction of androgen receptor into estrogen-receptor-, progesterone-receptor-, and androgen-receptor-negative breast cancer cells renders them responsive to hormonal manipulation. Am J Surg 2006;191:576–580.
Nielsen TO, Parker JS, Leung S, et al. A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor-positive breast cancer. Clin Cancer Res 2010;16:5222–5232.
Voduc KD, Cheang MC, Tyldesley S, et al. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 2010;28:1684–1691.
Blows FM, Driver KE, Schmidt MK, et al. Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med 2010;7:e1000279.
Cheang MCU, Chia SK, Voduc D, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 2009;101:736–750.
Acknowledgements
This study was supported by GlaxoSmithKline (WE234 (EP140307)); Public Health Service Grants CA087969, and SPORE in Breast Cancer CA089393, from the National Cancer Institute, National Institutes of Health, Department of Health and Human Services and Breast Cancer Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Collins, L., Cole, K., Marotti, J. et al. Androgen receptor expression in breast cancer in relation to molecular phenotype: results from the Nurses' Health Study. Mod Pathol 24, 924–931 (2011). https://doi.org/10.1038/modpathol.2011.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.54
Keywords
This article is cited by
-
Expression of hormone receptors is associated with specific immunological profiles of the breast cancer microenvironment
Breast Cancer Research (2023)
-
Molecular features of androgen-receptor low, estrogen receptor-negative breast cancers in the Carolina breast cancer study
Breast Cancer Research and Treatment (2023)
-
Determination of the androgen receptor status of disseminated tumor cells in primary breast cancer patients
Archives of Gynecology and Obstetrics (2023)
-
Correlation between androgen receptor expression and pathological response rate in pre-operative HER2-positive breast cancer patients
Journal of Cancer Research and Clinical Oncology (2023)
-
Clinical-pathologic characteristics and response to neoadjuvant chemotherapy in triple-negative low Ki-67 proliferation (TNLP) breast cancers
npj Breast Cancer (2022)