Abstract
Podocyte injury is a feature of glomerulopathies associated with proteinuria, which in turn has been used as a clinical prognostic factor for glomerular diseases. The goal of this study is to investigate the relationship between podocyte injury found in biopsied renal tissue and change of proteinuria in IgA nephropathy (IgAN). In all, 35 patients with biopsy-proven IgAN and proteinuria (>1.0 g per 24 h) were enrolled in the IgAN group, while 8 patients with excision of renal harmatoma or carcinoma served as kidney controls (Control). Immunohistochemistry was applied to detect the expression of nestin, cell-cycle regulatory protein p27, as well as complement C5b-9 and complement receptor 1 (CR1). Podocyte foot process width (FPW) and podocyte population in renal biopsied samples were measured by morphometric analysis. On the basis of the podocyte density (Nv), the IgAN patients were divided into podocytopenic group (n=17, Nv<57.10 /μm3 × 106) and normopodocytic group (n=18, Nv≥57.10 /μm3 × 106). Changes of proteinuria were followed for 18 months after biopsy. Compared with the Control, IgAN glomeruli had reduced podocyte expression of p27 and nestin along with decreased podocyte number. IgAN glomeruli also showed activation of C5b-9 in mesangial and subepithelial areas with decreased CR1 expression in podocytes. The C5b-9 positivity was inversely correlated with the number of WT-1-positive podocytes. Although the magnitude of proteinuria at biopsy correlated with podocyte FPW (P<0.05), the change in the amount of proteinuria expressed as proteinuria progression rate significantly correlated with the podocyte density. Thus, the normopodocytic group showed significantly lower proteinuria progression rate than the podocytopenic group regardless the comparable clinical features at biopsy and treatment regimen between the two groups. The results of this study indicate that, in IgAN, podocyte injury is involved in development of proteinuria and loss of podocytes predicts progression of the proteinuria. Complement activation may contribute to podocyte damage in IgAN.
Similar content being viewed by others
Main
IgA nephropathy (IgAN) is the most common type of primary glomerular nephritis in Southeast Asia.1 It has an extremely variable clinical course, ranging from persistent asymptomatic microscopic hematuria to rapidly progressive renal failure. Hypertension, impaired renal function, proteinuria and the severity of histologic lesions at the time of renal biopsy have been used to predict development of progressive renal disease in patients with IgAN.1, 2, 3, 4 As experimental evidence showing a direct deleterious effect of proteinuria on progressive kidney damage,5, 6, 7 sustained nephrotic-range proteinuria (>3–3.5 g/day) has long been accepted as a poor prognosis in many types of progressive glomerulopathies. In IgAN, proteinuria level of >1 g/day is an indicator for aggressive treatment involving corticosteroids.8 However, emerging studies have found that, rather than the amount of proteinuria appearing at diagnosis, it is the change in magnitude of the proteinuria that is a stronger predictor of renal outcome.4, 8, 9, 10, 11, 12 Consistent with these findings, a recent study reported that patients who achieved a sustained reduction in proteinuria have a better prognosis regardless the initial proteinuria level.13 Another study also showed that mean proteinuria during follow-up was a powerful independent prognostic predictor in IgAN.14 In this study, we chose the change of proteinuria as primary outcome.
Experimental and clinical studies suggest that proteinuria reflects damage and/or loss of glomerular podocytes. Indeed, recent studies have shown podocyte injury in proteinuric IgAN, which was characterized by reduced expression of podocyte markers such as GLEPP-1,15 nephrin and CD2AP,16, 17 necrosis and detachment of podocytes from the glomerular basement membrane (GBM),18 as well as decreased number of podocytes in Indians or Caucasians with IgAN.19, 20 Although such studies indicate that podocyte injury is associated with proteinuria at the time of biopsy, it is not clear whether podocyte injury predicts proteinuria progression and renal outcome in IgAN.
The mechanisms underlying IgAN remain unclear. Aberrantly glycosylated IgA molecules have been found in the glomerular mesangium with IgAN.21 These deposits were postulated to activate mesangial cells22, 23 and local complements.24 Mesangial activation of C3 may occur through the mannan-binding lectin pathway or alternative pathway leading to the generation of C5b-9 in IgAN.25, 26 A recent study showed that positive mesangial C4d staining, a downstream activated complement factor of mannan-binding lectin pathway, was associated with evolution to end-stage renal disease in patients with IgAN.27 The mRNA expression ratio of C3 to DAF (decay accelerating factor, a candidate for the focal suppression of complement activation) of glomerular cells was also found to be correlated with the severity of glomerular injury in IgAN.28 Moreover, it has also been found that subepithelial deposition of C5b-9 could attack podocytes in membranous nephropathy. In contrast, normal podocyte itself may synthesize complement regulatory proteins, such as complement receptor 1 (CR1), to reduce susceptibility to complement attack.29 Thus, we also studied whether complement activation took part in podocyte injury in IgAN.
Thus, this study examined podocyte injury in IgAN and its effects on proteinuria at the time of diagnosis as well as proteinuria progression. We also accessed the possible relationship between complement activation and podocyte injury. We found that, hypertension, impaired renal function and level of proteinuria at the time of renal biopsy did not predict progression, instead podocyte density significantly related with the resolution of proteinuria.
Materials and methods
Subjects
All proteinuric patients who underwent renal biopsy in our renal care program and received the diagnosis of IgAN from January 2000 were enrolled into the study. The included patients met the following criteria: (1) dominant or co-dominant deposition of mesangial IgA by immunofluorescence microscopy; (2) exclusion of diseases with IgA deposition, including systemic lupus erythematosus, Schönlein-Henoch purpura and liver disease; (3) proteinuria >1.0 g/day; and (4) normal serum creatinine. A total of 35 IgAN patients were included. Eight patients with excision of renal harmatoma or carcinoma without proteinuria or hematuria, hypertension or renal impairment served as kidney controls (Control).
This study was approved by the Institutional Review Board of Research Ethics Committee of Huashan Hospital, Fudan University, Shanghai, China.
Clinical and Laboratory Data
Serum IgA, C3, C4, creatinine, magnitude of proteinuria based on 24-hr urine collections and blood pressure were assessed at biopsy, the time referred as baseline, and over time. Each patient was evaluated with laboratory tests every 3 months for 18 months, including 24-h urine protein, serum creatinine and blood pressure.
The effect of treatment was evaluated by the proteinuria progression rate, reflecting the rate change of proteinuria from baseline, with the percent change plotted for each subject. A regression line then was drawn, and the slope of this line reflecting the average percent change of proteinuria per month was referred as the proteinuria progression rate. We also defined partial remission when proteinuria dropped to <0.5 g/day, and complete remission when proteinuria was <0.2 g/day during the follow-up.
Each IgAN patient received renoprotective therapy with either an angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker. The use of corticosteroid or immunosuppressant was recorded.
Routine Examinations on Biopsied Renal Tissue
Renal specimens, obtained by needle-core biopsies (14- or 16-gauge) performed under ultrasonographic guidance, were fixed with 4% paraformaldehyde in phosphate-buffered saline, dehydrated although graded alcohols, embedded in paraffin, then sectioned for routine stainings (hematoxylin & eosin, periodic acid-Schiff, silver methenamine and Masson's trichrome). The biopsies were graded according to the scheme of Lee et al.30 Detailed renal morphologic changes were also evaluated for mesangial cellularity, percentage of segmental sclerotic glomeruli, percentage of glomeruli showing endocapillary hypercellularity, percentage of crescent glomeruli and interstitial fibrosis.31 For each case, at least eight glomeruli were scored.
Frozen tissue sections were processed for routine immunofluorescence microscopy with antisera for IgG, IgA, IgM, C3, C1q and fibrinogen. Mesangial immunoglobulins and C3 by immunofluorescence were semiquantitated (0—negative, 1—minimally positive, 2—moderately positive and 3—maximally positive).
Immunohistochemistry
Four-micron-thick paraffin-embedded tissue sections were used in the study, and a two-step EnVision System peroxidase kit (Dako, USA) was used for immunohistochemistry. Slides were subjected to microwave antigen retrieval with wet heat at sub-boiling temperature for 10 min before the addition of antibodies against Wilm's tumor-1 (WT-1, 1:800, Santa Cruz Biotechnology, USA), nestin (1:400, BD Biosciences, USA), p27 (1:200, Dako), CR1 (1:25, Dako) and C5b-9 (1:25, Abcam, UK).
Dual immunostainings for laminin and C5b-9 were conducted as follows: frozen sections were air dried and fixed in 4% buffered paraformaldehyde for 10 min, incubated with rabbit anti-mouse laminin (1:100, Santa Cruz) at 37 °C for 1 h, then anti-rabbit-Cy2 (1:600, Vector Laboratories, USA) at room termperature for 45 min, followed by C5b-9 immunostaining with primary mouse monoclonal antibodies against human C5b-9 then Cy3-conjugated rabbit anti-mouse IgG (1:800, Dako). The stained sections were examined by confocal microscopy (Leica TSP SP20).
The number of p27-positive nuclei per glomerulus was counted, and the assessment for localization to podocytes was based on the cell morphology and relationship to the basement membrane. Nestin, C5b-9, CR1 expressions were evaluated by the percentage of positive area in the glomeruli. Negative control slides were treated with nonspecific antisera instead of primary antibody. All stainings were reviewed and analyzed without knowledge of the group.
Podocytic Morphometrics
Podocytes were identified by immunohistochemical staining for WT-1, a podocyte differentiation marker. The density of WT-1-positive podocytes in the glomerulus (Nv), that is, the number of podocytes per glomerular volume unit (μm3 × 106) was calculated as previously reported32: Nv=1/β(NA3/VV),1/2 where Nv is the number density of cells per μm3 of tuft volume; NA is the number of intersections of cell nuclei per μm2 of tuft area; VV is fractional areal density of the nuclei; β is the shape factor for prolate ellipsoids, which has the value of 1.65 for podocytes. All biopsied glomeruli were analyzed except for the ones with global sclerosis. The mean podocyte Nv was counted as 323.22±135.78/μm3 × 106 (mean±s.d.) in Control group. A cut-off value <57.10 /μm3 × 106, the low 2.5 percentile of the Nv in Control group, was applied as the criterion for podocyte depletion. This value is lower than the criteria that were applied in human studies with diabetic nephropathy.33, 34 By that, 35 IgAN cases were further divided into two groups: podocytopenic group (n=17, Nv<57.10/μm3 × 106), and normopodocytic group (n=18, Nv≥57.10/μm3 × 106).
Transmission electron microscopy (EM) was used to assess podocyte foot process width (FPW). As previously reported,35 10 photographs (10 000 × ) covering one or two glomerular cross-sections were taken by transmission electron microscope (Philips CM10, Eindhoven, The Netherlands). The length of the peripheral GBM was measured and the number of slit pores was counted. The arithmetic mean of the FPW was calculated as follow: FPW=π/4 × ∑GBM length/∑slits, where the ∑slits was the total number of slits counted, ∑GBM length was the total GBM length measured in one glomerulus, and the correction factor π/4 served to correct for the random orientation in which the foot processes were sectioned.
Statistical Analysis
Data were expressed as mean±standard error of mean unless otherwise specified. Mann–Whitney U-tests were used for between-group comparisons. Spearman correlation followed by univariate linear regression analysis was applied to uncover the correlations between nominal variables. Differences of the follow-up parameters were analyzed by mixed model, and difference in remission rate during the study was analyzed by χ2 test. All statistical tests were two-sided and significance was defined as P<0.05. Statistical analysis was performed using Stata and SPSS.
Results
Podocyte Injury and Loss in IgAN
In glomeruli of Control kidneys, most podocytes expressed p27, a negative cell-cycle regulatory protein that maintains podocytes in quiescence by arresting cell cycle in G1 phase.36 By contrast, the proportion of p27-positive podocytes was significantly decreased in glomeruli of IgAN (Control 91.1±2.7 vs IgAN 71.3±2.5%, P<0.05, Figure 1a). As a type VI intermedial filament, nestin is one of the constitutive proteins expressed in the cytoplasm of podocytes, stained in a linear pattern along the GBM. In IgAN, the percentage of nestin-positive area in the glomerulus was decreased by some 30% (Control 17.3±1.8% vs IgAN 12.5±0.9%, P<0.05, Figure 1b) and the continuity of the normal staining pattern was interrupted. Transmission EM revealed podocyte vacuolization, microcystic change, foot process effacement and detachment from the GBM in some glomeruli with IgAN. In areas with reduced number of podocytes, there was focal denudation of the underlying GBM.
Podocyte density (Nv) was significantly lower in the IgAN group than the Control (Control 323±46 vs IgAN 161±38/μm3 × 106, P<0.05, Figure 1c). This decrease in podocyte population coincided with increased severity of glomerular injury, which was reflected by the Lee's grade of IgAN (359±269 /μm3 × 106 for grade I, 270±103 for grade II, 166±81 for grade III and 79±25 for grade IV).
Complement Activation and Association with Podocyte Injury
In IgAN, C3 was found primarily deposited in the mesangial area and occasionally along the capillary loops. Semi-quantitation showed a trend for more C3 deposition in glomeruli with fewer podocytes (Figure 2a). C5b-9 was also mainly expressed in the mesangium and partly located in subepithelial area, a finding confirmed by co-staining for GBM protein laminin (Figure 2b). In addition, C5b-9 deposition inversely correlated with the number of WT-1-positive cells in glomeruli (Figure 2b). In Control glomeruli, CR1 was expressed primarily in the cytoplasm of podocytes (Figure 3a). In IgAN glomeruli, the CR1-positive area was significantly decreased compared with the Control (15.0±1.8 vs 23.8±2.8%, P<0.05, Figure 3a). There was also an inverse correlationship between C5b-9 deposition and CR1 expression in podocytes (Figure 3b), indicating the role of decreased CR1 expression in the increased susceptibility of podocytes to C5b-9 attack.
Relationship of complement activation and podocyte injury in IgAN. (A) Decreased number of WT-1-positive podocytes in IgAN tended to be associated with increased C3 deposition in glomeruli. (B) C5b-9, an activated complement product, which was expressed mainly in glomerular mesangium and partly in subepithelial area (arrow in (a) and arrowhead in (b)). This localization was confirmed by dual staining for laminin (b), in which confocal microscopy revealed some positive C5b-9 deposition (red) outside the laminin-positive GBM (green). Magnifications were 400 for (a), and 600 for (b). The area with positive C5b-9 deposition in IgAN glomeruli was negatively correlated with the podocyte number.
Relationship of CR1 and C5b-9 in IgAN. (a) CR1, a protective mechanism against complement attack, was normally expressed on podocytes in a continuous and linear pattern as shown in Control. In IgAN, the expression of CR1 was significantly decreased and changed to a discontinuous and dotted pattern (400). (b) Spearman correlation analysis showed that the area with positive C5b-9 deposition in IgAN glomeruli negatively correlated with the CR1 positivity.
Relationship between Podocyte Injury and Proteinuria at Biopsy
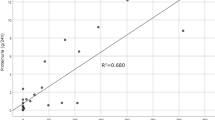
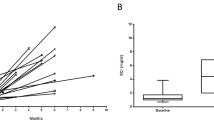
A significant correlation was found between the podocyte FPW and the amount of proteinuria at the time of biopsy (Figure 4a), the latter one of which also tended to correlate with podocyte density (P=0.07, Figure 4b). Moreover, the podocyte density was found significantly correlated with proteinuria progression rate (Figure 5a). However, the clinical characteristics of normopodocytic group and podocytopenic group were not significantly different at the time of biopsy (Table 1). It is noteworthy that this relationship was not affected by treatment with corticosteroid and angiotensin blocking drugs. Thus, patients with podocytopenia at biopsy had significantly slower reduction in proteinuria than normopodocytic patients regardless of treatment (P<0.05, Figure 5b). Futhermore, after 18 months follow-up, the complete remission rate, partial remission rate and total remission rate were all significantly greater in the normopodocytic group (complete remission rate 28%, partial remission rate 39% and total remission rate 67%) than in the podocytopenic group (complete remission rate 12%, partial remission rate 23% and total remission rate 35%, Figure 5c). As there was no significant differences in the glomerular histologic changes comparing the podocytopenic with the normopodocytic group (mesangial cellularity score 0.46±0.12 vs 0.66±0.12, percentage of glomeruli showing segmental sclerosis 53 vs 56%, percentage of glomeruli showing endocapillary hypercellularity 24 vs 28%, percentage of glomeruli showing crescents 12 vs 17% and interstitial fibrosis score 1.33 vs 1.07), the different resolution of proteinuria in IgAN patients was determined mainly by the level of podocyte injury in this study.
Relationship between podocyte population and progression of IgAN. (a) Proteinuria progression rate correlated to podocyte density. (b) IgAN patients with normal range podocyte number showed significantly more rapid decrease in proteinuria during follow-up when compared with the podocytopenic subjects (P<0.05 by mixed model analysis). (c) Significantly fewer individuals reached complete or partial regression in the podocytopenic group than in the group with normal-range podocyte number (P<0.05 by χ2 test).
Discussion
Proteinuria is not only a hallmark of glomerulopathy, but also is believed to be a mechanism of progressive glomerular damage.37 Several clinical studies have shown that proteinuria is a strong prognostic factor for IgAN progression.8, 9, 12 Our study revealed multiple podocyte injuries in proteinuric IgAN, including decreased cell-cycle protein p27, decreased type IV intermediate filament nestin expression, widened foot process and ultimately decreased podocyte density. We further showed that podocyte injury, especially the number of podocytes is a better predictor of progression than the level of proteinuria at the time of biopsy in IgAN. We also found that complement activation correlates with podocyte injury.
The blood-to-urine barrier, that is, glomerular filtration barrier, is highly organized and consists of three different layers: the fenestrated endothelium of glomerular capillaries, GBM, which is the fused basal lamina of endothelial cells and podocytes, and the filtration slits of the podocytes. Podocyte injury, which occurs in minimal change disease, focal segmental glomerular sclerosis and diabetic nephropathy, is considered to be a key factor associated with proteinuria.38 Podocytes can retract and broaden their foot processes after injury and detach from the GBM when injury becomes severe.39 In our study, increased FPW correlated and decreased podocyte density tended to correlate with the level of proteinuria at time of biopsy. These findings are in consistence with the results from some other groups that podocytopenia associates with the amount of proteinuria in IgAN.19, 20
Podocytopenia has been found associated with development of glomerulosclerosis in several human and experimental diseases,40 and the loss of podocyte population parallels progression of glomerulosclerosis.41 Our study also noted that decreased podocyte density paralleled the Lee's grade of IgAN. In an animal model with chronic glomerulopathy, increased and persistent urinary excretion of podocytes correlates with the progression of the disease.42 Moreover, recent studies have shown that corticosteroid treatment may have direct effects on podocytes.43, 44 In contrast, the clinical response to immunosuppression therapy in focal segmental glomerular sclerosis is different according to the podocyte number.45 We, therefore, postulated that it was not the severity of the proteinuria at diagnosis but rather the dynamic change of proteinuria during treatment and follow-up that is a more important predictor for the outcome of IgAN. Indeed, the results of our study showed a significant correlation between podocyte density and proteinuria progression rate. The rate change of proteinuria in IgAN patients with normal podocyte number is significantly slower than those with podocytopenia. Our data also indicated that the IgAN patients in podocytopenia group were less likely to have remission in proteinuria than the patients in normopodocytic group, regardless of the comparable baseline characteristics or therapeutic regimens. We did not see remarkable changes in renal function parameters in our IgAN patients, although the follow-up period is relatively short.
It was previously found that IgA per se does not directly induce podocyte injury.16, 46 There is an increasing body of evidence showing that stress-tension, a result of increased intraglomerular pressure, causes podocyte injury and loss,47, 48 in which increased activity of angiotensin II and its type 1 receptor AT1 have an important role.48, 49 Other mechanisms that are involved in IgAN-related podocyte injury include increased level of proinflammatory factor TNF-α.16, 46 In our study, we unveiled that complement activation may contribute to podocyte injury in IgAN. It is known that IgAN is an immune-mediated disease characterized by IgA deposition in mesangial area, followed by C3 activation through alternative pathway or lectin pathway,25 and finally formation of membrane attack complex C5b-9.50 In our study, C5b-9 deposited not only in mesangial area but also in subepithelial area, indicating that C5b-9 might directly attack podocytes in IgAN. Podocytes that undergo C5b-9 attack may produce oxidants, laminin and type IV collagen,51 disrupt actin microfilaments,52 upregulate cyclooxygenase-253 and induce DNA damage.54 Moreover, podocytes express CR1, which is a physiological inhibitor of C3.55 We found that the CR1 expression on podocytes decreased significantly in IgAN, which was also reported by other investigators.56 It has been suggested that the decrease in CR1 on podocytes is not due to consumption but due to decreased synthesis. Loss of CR1 synthesis might increase the sensitivity of podocytes to complement attack.36, 57 Our observation of inverse correlationship between podocyte density and C5b-9 deposition in glomeruli suggested that complement activation might take part in podocyte injury in IgAN.
In summary, results from our study indicate that there are multiple podocyte injuries in IgAN with proteinuria. Loss of podocytes not only associated with proteinuria at diagnosis but also predicted progression of proteinuria in IgAN. We also show that complement activation may contribute to podocyte injury in IgAN. These findings might be relevant to future therapeutic and prognostic considerations for IgAN.
References
D’Amico G, Minetti L, Ponticelli C, et al. Prognostic indicators in idiopathic IgA mesangial nephropathy. Q J Med 1986;59:363–378.
Alamartine E, Sabatier JC, Guerin C, et al. Prognostic factors in mesangial IgA glomerulonephritis: an extensive study with univariate and multivariate analyses. Am J Kidney Dis 1991;18:12–19.
Katafuchi R, Oh Y, Hori K, et al. An important role of glomerular segmental lesions on progression of IgA nephropathy: a multivariate analysis. Clin Nephrol 1994;41:191–198.
Bartosik LP, Lajoie G, Sugar L, et al. Predicting progression in IgA nephropathy. Am J Kidney Dis 2001;38:728–735.
Morigi M, Macconi D, Zoja C, et al. Protein overload-induced NF-kappaB activation in proximal tubular cells requires H(2)O(2) through a PKC-dependent pathway. J Am Soc Nephrol 2002;13:1179–1189.
Zoja C, Benigni A, Remuzzi G . Cellular responses to protein overload: key event in renal disease progression. Curr Opin Nephrol Hypertens 2004;13:31–37.
Tang S, Leung JC, Abe K, et al. Albumin stimulates interleukin-8 expression in proximal tubular epithelial cells in vitro and in vivo. J Clin Invest 2003;111:515–527.
Jafar TH, Stark PC, Schmid CH, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med 2003;139:244–252.
Donadio JV, Bergstralh EJ, Grande JP, et al. Proteinuria patterns and their association with subsequent end-stage renal disease in IgA nephropathy. Nephrol Dial Transplant 2002;17:1197–1203.
Szeto CC, Lai FM, To KF, et al. The natural history of immunoglobulin a nephropathy among patients with hematuria and minimal proteinuria. Am J Med 2001;110:434–437.
Radford Jr MG, Donadio Jr JV, Bergstralh EJ . Predicting renal outcome in IgA nephropathy. J Am Soc Nephrol 1997;8:199–207.
Eiro M, Katoh T, Kuriki M, et al. The product of duration and amount of proteinuria (proteinuria index) is a possible marker for glomerular and tubulointerstitial damage in IgA nephropathy. Nephron 2002;90:432–441.
Reich HN, Troyanov S, Scholey JW, et al. Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 2007;18:3177–3183.
Coppo R, D’Amico G . Factors predicting progression of IgA nephropathies. J Nephrol 2005;18:503–512.
Tian J, Wang HP, Mao YY, Jin J, et al. Reduced glomerular epithelial protein 1 expression and podocyte injury in immunoglobulin A nephropathy. J Int Med Res 2007;35:338–345.
Lai KN, Leung JC, Chan LY, et al. Podocyte injury induced by mesangial-derived cytokines in IgA nephropathy. Nephrol Dial Transplant 2009;24:62–72.
Gagliardini E, Benigni A, Tomasoni S, et al. Targeted downregulation of extracellular nephrin in human IgA nephropathy. Am J Nephrol 2003;23:277–286.
Ng WL, Chan KW, Yeung CK, et al. Peripheral glomerular capillary wall lesions in IgA nephropathy and their implications. Pathology 1984;16:324–330.
Hishiki T, Shirato I, Takahashi Y, et al. Podocyte injury predicts prognosis in patients with IgA nephropathy using a small amount of renal biopsy tissue. Kidney Blood Press Res 2001;24:99–104.
Lemley KV, Lafayette RA, Safai M, et al. Podocytopenia and disease severity in IgA nephropathy. Kidney Int 2002;61:1475–1485.
Giannakakis K, Feriozzi S, Perez M, et al. Aberrantly glycosylated IgA1 in glomerular immune deposits of IgA nephropathy. J Am Soc Nephrol 2007;18:3139–3146.
Duque N, Gomez-Guerrero C, Egido J . Interaction of IgA with Fc alpha receptors of human mesangial cells activates transcription factor nuclear factor-kappa B and induces expression and synthesis of monocyte chemoattractant protein-1, IL-8, and IFN-inducible protein 10. J Immunol 1997;159:3474–3482.
Lai KN, Tang SC, Guh JY, et al. Polymeric IgA1 from patients with IgA nephropathy upregulates transforming growth factor-beta synthesis and signal transduction in human mesangial cells via the renin-angiotensin system. J Am Soc Nephrol 2003;14:3127–3137.
Bogers WM, Stad RK, van Es LA, et al. Immunoglobulin A: interaction with complement, phagocytic cells and endothelial cells. Complement Inflamm 1991;8:347–358.
Hisano S, Matsushita M, Fujita T, et al. Mesangial IgA2 deposits and lectin pathway-mediated complement activation in IgA glomerulonephritis. Am J Kidney Dis 2001;38:1082–1088.
Abe K, Miyazaki M, Koji T, et al. Intraglomerular synthesis of complement C3 and its activation products in IgA nephropathy. Nephron 2001;87:231–239.
Espinosa M, Ortega R, Gomez-Carrasco JM, et al. Mesangial C4d deposition: a new prognostic factor in IgA nephropathy. Nephrol Dial Transplant 2009;24:886–891.
Abe K, Miyazaki M, Koji T, et al. Expression of decay accelerating factor mRNA and complement C3 mRNA in human diseased kidney. Kidney Int 1998;54:120–130.
Kelly LJ, Vicario PP, Thompson GM, et al. Peroxisome proliferator-activated receptors gamma and alpha mediate in vivo regulation of uncoupling protein (UCP-1, UCP-2, UCP-3) gene expression. Endocrinology 1998;139:4920–4927.
Lee HS, Lee MS, Lee SM, et al. Histological grading of IgA nephropathy predicting renal outcome: revisiting HS Lee's glomerular grading system. Nephrol Dial Transplant 2005;20:342–348.
Roberts IS, Cook HT, Troyanov S, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int 2009;76:546–556.
Weibel E . Stereologic Methods. Practical Methods for Biological. Academic Press: London, 1979, pp 415.
White KE, Bilous RW . Structural alterations to the podocyte are related to proteinuria in type 2 diabetic patients. Nephrol Dial Transplant 2004;19:1437–1440.
White KE, Bilous RW, Marshall SM, et al. Podocyte number in normotensive type 1 diabetic patients with albuminuria. Diabetes 2002;51:3083–3089.
van den Berg JG, van den Bergh Weerman MA, Assmann KJ, et al. Podocyte foot process effacement is not correlated with the level of proteinuria in human glomerulopathies. Kidney Int 2004;66:1901–1906.
Nagata M, Nakayama K, Terada Y, et al. Cell cycle regulation and differentiation in the human podocyte lineage. Am J Pathol 1998;153:1511–1520.
Abbate M, Zoja C, Remuzzi G . How does proteinuria cause progressive renal damage? J Am Soc Nephrol 2006;17:2974–2984.
Jalanko H, Patrakka J, Tryggvason K, et al. Genetic kidney diseases disclose the pathogenesis of proteinuria. Ann Med 2001;33:526–533.
Shankland SJ . The podocyte's response to injury: role in proteinuria and glomerulosclerosis. Kidney Int 2006;69:2131–2147.
Matsusaka T, Xin J, Niwa S, et al. Genetic engineering of glomerular sclerosis in the mouse via control of onset and severity of podocyte-specific injury. J Am Soc Nephrol 2005;16:1013–1023.
Wharram BL, Goyal M, Wiggins JE, et al. Podocyte depletion causes glomerulosclerosis: diphtheria toxin-induced podocyte depletion in rats expressing human diphtheria toxin receptor transgene. J Am Soc Nephrol 2005;16:2941–2952.
Hara M, Yanagihara T, Kihara I . Cumulative excretion of urinary podocytes reflects disease progression in IgA nephropathy and Schonlein-Henoch purpura nephritis. Clin J Am Soc Nephrol 2007;2:231–238.
Ransom RF, Vega-Warner V, Smoyer WE, et al. Differential proteomic analysis of proteins induced by glucocorticoids in cultured murine podocytes. Kidney Int 2005;67:1275–1285.
Wada T, Pippin JW, Marshall CB, et al. Dexamethasone prevents podocyte apoptosis induced by puromycin aminonucleoside: role of p53 and Bcl-2-related family proteins. J Am Soc Nephrol 2005;16:2615–2625.
Kim YH, Goyal M, Kurnit D, et al. Podocyte depletion and glomerulosclerosis have a direct relationship in the PAN-treated rat. Kidney Int 2001;60:957–968.
Lai KN, Leung JC, Chan LY, et al. Activation of podocytes by mesangial-derived TNF-alpha: glomerulo-podocytic communication in IgA nephropathy. Am J Physiol Renal Physiol 2008;294:F945–F955.
Endlich N, Kress KR, Reiser J, et al. Podocytes respond to mechanical stress in vitro. J Am Soc Nephrol 2001;12:413–422.
Durvasula RV, Petermann AT, Hiromura K, et al. Activation of a local tissue angiotensin system in podocytes by mechanical strain. Kidney Int 2004;65:30–39.
Ding G, Reddy K, Kapasi AA, et al. Angiotensin II induces apoptosis in rat glomerular epithelial cells. Am J Physiol Renal Physiol 2002;283:F173–F180.
Nangaku M, Alpers CE, Pippin J, et al. CD59 protects glomerular endothelial cells from immune-mediated thrombotic microangiopathy in rats. J Am Soc Nephrol 1998;9:590–597.
Torbohm I, Schonermark M, Wingen AM, et al. C5b-8 and C5b-9 modulate the collagen release of human glomerular epithelial cells. Kidney Int 1990;37:1098–1104.
Topham PS, Haydar SA, Kuphal R, et al. Complement-mediated injury reversibly disrupts glomerular epithelial cell actin microfilaments and focal adhesions. Kidney Int 1999;55:1763–1775.
Takano T, Cybulsky AV . Complement C5b-9-mediated arachidonic acid metabolism in glomerular epithelial cells : role of cyclooxygenase-1 and -2. Am J Pathol 2000;156:2091–2101.
Pippin JW, Durvasula R, Petermann A, et al. DNA damage is a novel response to sublytic complement C5b-9-induced injury in podocytes. J Clin Invest 2003;111:877–885.
Puri TS, Quigg RJ . The many effects of complement C3- and C5-binding proteins in renal injury. Semin Nephrol 2007;27:321–337.
Moll S, Miot S, Sadallah S, et al. No complement receptor 1 stumps on podocytes in human glomerulopathies. Kidney Int 2001;59:160–168.
Teixeira JE, Costa RS, Lachmann PJ, et al. CR1 stump peptide and terminal complement complexes are found in the glomeruli of lupus nephritis patients. Clin Exp Immunol 1996;105:497–503.
Acknowledgements
This study was supported by National Natural Science Foundation of China (30570858), Excellence of Yong Teachers Program (EYTP) and 211 Program from Ministry of China. We thank Dr Valentina Kon for kind reviewing and helpful suggestions during the preparation of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Xu, L., Yang, HC., Hao, CM. et al. Podocyte number predicts progression of proteinuria in IgA nephropathy. Mod Pathol 23, 1241–1250 (2010). https://doi.org/10.1038/modpathol.2010.110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.110
Keywords
This article is cited by
-
Mitofusin2 expression is associated with podocyte injury in IgA nephropathy
European Journal of Medical Research (2023)
-
Inactivation of mediator complex protein 22 in podocytes results in intracellular vacuole formation, podocyte loss and premature death
Scientific Reports (2020)
-
Parthenolide ameliorates tweak-induced podocytes injury
Molecular Biology Reports (2020)
-
IgA nephropathy
Nature Reviews Disease Primers (2016)
-
ELISA analysis of urinary nephrin and podocalyxin standardized by aquaporin-2 in adult patients with nephrotic syndrome
Journal of Nephrology (2014)