Abstract
The aim of this study was to evaluate the prognostic value of Ki67 in relation to established prognostic factors in lymph node-negative breast cancer, and furthermore, whether the prognostic impact was dependent on estrogen receptor (ER) status and histological grade. In 200 premenopausal patients, with 5 years of follow-up, Ki67 was determined on tissue microarrays. In univariate analysis, Ki67 (≤20 vs >20%) was a prognostic factor for distant disease-free survival (hazard ratio: 2.7, 95% confidence interval: 1.3–5.4, P=0.005) and overall survival (hazard ratio: 4.9, 95% confidence interval: 1.7–14, P=0.003). When stratifying for ER status and histological grade, Ki67 was a significant prognostic factor for distant disease-free survival and overall survival only in the ER-positive group, and only in patients with histological grade 2, respectively. In multivariate analysis, human epidermal growth factor receptor 2 and age were independent prognostic factors for distant disease-free survival, whereas Ki67, histological grade, and tumor size were not. Ki67 was, however, an independent prognostic factor in the 87% of the patients who had not received adjuvant medical treatment. Agreement between the three readers was very good (κ-values: 0.83–0.88). Furthermore, Ki67 was a significant prognostic factor for all three investigators (hazard ratio: 2.7–3.2). This study shows that Ki67 is a prognostic factor in node-negative breast cancer. It is noteworthy that the prognostic information of Ki67 is restricted to ER-positive patients, and to patients with histological grade 2. Taken together, Ki67, as an easily assessed and reproducible proliferation factor, may be an alternative or complement to histological grade as a prognostic tool and for selection of adjuvant treatment.
Similar content being viewed by others
Main
Breast cancer is a diagnosis with large variability in prognosis. Generally established prognostic and treatment predictive factors in node-negative breast cancer are age, tumor size, histological grade, estrogen receptor (ER) and progesterone receptor (PR) status, and human epidermal growth factor receptor 2 (HER2) status.1, 2, 3 There is, however, a need to better identify patients with a high risk of relapse, as adjuvant treatment, especially chemotherapy, should be avoided for low-risk patients. High proliferation rates have been shown to be associated with worse prognosis in breast cancer, and also with a higher probability of response to chemotherapy.1, 3, 4, 5, 6, 7, 8
Proliferation can be measured by thymidine labeling index and flow cytometric analysis of S-phase fraction. These two markers have been evaluated in prospective trials,9, 10 but the complexity of the assays and the need for fresh frozen tumor tissue have limited their use.1, 4
Gene array profiling as a prognostic tool has led to further subclassification of breast cancer, and revealed prognostic differences within ER-positive disease and patients with histological grade 2, subgroups previously considered homogenous.6, 11, 12, 13, 14, 15, 16 In many of these genetic signatures, the majority of genes are genes of proliferation, suggesting an importance of proliferation in determining prognosis.3, 6, 11, 12, 13, 14, 15, 16 One gene signature is recommended by the ASCO guidelines,1 and according to the last St Gallen guidelines, multigene assays could assist in deciding whether to add chemotherapy in cases where its use was uncertain after consideration of conventional markers.3 However, costs for these tests are still substantial, and no results from prospective trials have yet been presented.
As far as Ki67 is concerned, several studies have shown that high Ki67 proliferation index is associated with worse distant disease-free survival and/or overall survival in both node-positive and node-negative patients.5, 8, 17, 18, 19, 20, 21, 22 It is also a predictor of better response to chemotherapy.5, 7 Furthermore, as Ki67 is also affordable and easily assessed on paraffin-embedded tumor material, it has been widely used, even though it has not been generally recommended for use by all guidelines,1, 2 as there is no international standardization for the method. However, Ki67 and mitotic frequency have just recently been included in the St Gallen guidelines, but it is noted that the reliability of these measures still varies in different geographic settings.3
The first aim was to compare the prognostic value of Ki67 to the established prognostic factors in premenopausal patients with lymph node-negative breast cancer, and as the prognostic impact of gene array profiling varies depending on ER status and histological grade, we specifically aimed at studying whether the prognostic value of Ki67 differed in corresponding subgroups. Second, by using both semi-quantitative and quantitative assessments of Ki67, agreement between readers and different methods of Ki67 quantification was assessed.
Materials and methods
Patients
The initial patient population consisted of 237 premenopausal women with lymph node-negative breast cancer, included from 1991 to 1994 in a prospective study of the prognostic value of S-phase fraction.9 Ki67 was considered evaluable in 200 of these 237 patients. In 14 cases, no paraffin blocks were retrieved from the pathology departments, and for the remaining cases, 16 were non-evaluable because of staining difficulties, and 7 cases because of the individual tumor sections being lost in the tissue microarray or otherwise non-evaluable. Primary surgical treatment, postoperative radiation, and adjuvant systemic treatment have been described earlier in detail.9 Patient and tumor characteristics are presented in Table 1.
The median follow-up for the end point distant metastasis was 10.8 years for patients alive and free from distant metastases at the latest review of the patients’ records, but because of non-proportional hazards for most of the prognostic factors studied, results for the first 5 years are presented. The study was approved by the ethics committee of Lund University Hospital.
Histological Grading, ER and PR Analysis
Tumor grading was performed according to Elston and Ellis.23 All tumor specimens were re-evaluated by seven experienced pathologists, performed without any knowledge of patient history. Five preparations were excluded because of poor staining. ER and PR were analyzed as described earlier.9
Tumor Tissue Microarray
A tissue microarray was constructed from the paraffin-embedded histopathological blocks. Two 0.6-mm core biopsies were obtained from representative areas of each tumor, and brought into a new paraffin block using a manual arrayer (Beecher Instruments, MD, USA). Sections (4 μm) were made and stained with hematoxylin and eosin B. Both core biopsies were evaluated, and the one with the highest percentage of positively stained cells was chosen.
Ki67
Ki67 index was determined by the labeled streptavidin biotin method using the antibody MIB-1 (DAKO, K5001, Copenhagen, Denmark). Antigen retrieval was performed in a microwave oven in citrate buffer for 15 min. Slides were stained in a TechMate 500 (DAKO) with an incubation time of 25 min at room temperature and with MIB-1 diluted 1:500. Diaminobenzidene was used as chromogen.
The tumors were assessed independently by three of the investigators. The semi-quantitative assessment was done by a pathologist (DG) and categorized into 12 groups, 0–1, 2–5, 6–10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, 81–90, and 91–100%. The cutoff was predefined at the seventh decile,18 corresponding to a high Ki67 proliferation index of >20% positively stained tumor cells. In the quantitative assessments, all tumor cells in the tissue microarray were counted independently by two of the investigators (KL and MK).
HER2 Status
HER2 protein was detected by Herceptest (DAKO K5206, Copenhagen, Denmark), whereas gene amplification was determined by HER2 FISH pharmDxTM Kit (DAKO K5331, Copenhagen, Denmark) according to the manufacturer's instructions. Seven tumors were not evaluable because of insufficient tumor material or fixation artefacts. All patients with amplified tumors, and all with Herceptest 3+ where fluorescent in situ hybridization analysis could not be evaluated, were considered HER2-positive.
Statistical Methods
Distant disease-free survival was chosen as primary and overall survival as secondary end point. The Kaplan–Meier method was used to estimate distant disease-free survival, and the log-rank test was used to compare survival in different strata. The Cox proportional hazards model was used for estimation of univariate and multivariate hazard ratios. Proportional hazards assumptions were checked both graphically and by Schoenfeld's test.24 All factors were used as dichotomous covariates in the statistical analysis, with the exception of grade (three groups) and age, which was also analyzed as a continuous variable. The null hypothesis of no prognostic effect by Ki67 in ER-positive and ER-negative patients was evaluated using a Cox model with a term for the interaction between ER status and Ki67. Cutoff values were chosen before statistical analyses. For the established prognostic factors, standard cutoff values were used, and were the same as for earlier published patient series.9 For Ki67 the seventh decile was chosen.18 Association between the factors were analyzed using Pearson's χ2 test, and for histological grade, Pearson's χ2 test for trend. All P-values corresponded to two-sided tests. Kappa statistics were used to evaluate the agreement between the three readers regarding Ki67 status. Unless otherwise stated, P<0.05 was considered significant. The statistical calculations were performed using Stata Version 11.0 (StataCorp 2009, College Station, TX, USA).
Results
Patient and Tumor Characteristics
During the first 5 years of follow-up, 25 patients were diagnosed with locoregional recurrences. Distant metastases were recorded in 32 patients, and at 5 years the distant disease-free survival was 84% (95% confidence interval: 78–88%) and the overall survival was 92% (95% confidence interval: 87–95%). Detailed characteristics of the patients are presented in Table 1. With the exception of reproducibility data, results from the semi-quantitative assessments were used for all the following analyses. The median Ki67 value was 10%, and the interquartile range was 5–30%. High Ki67 was associated with age <50 years, large tumor size, histological grade 3, ER-negativity, PR-negativity, and HER2-positivity (Table 2).
Distant Disease-Free Survival
Univariate analyses
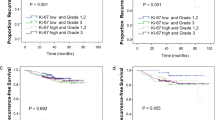
In univariate analysis, Ki67 was a prognostic factor for distant disease-free survival (hazard ratio: 2.7, 95% confidence interval: 1.3–5.4, P=0.005). At 5 years, distant disease-free survival for the low- and high-risk groups was 89 and 73%, respectively (Figure 1). The strongest univariate prognostic factor for distant disease-free survival was HER2, followed by age, PR, Ki67, histological grade (3 vs 1+2), and ER. Histological grade 2+3 vs 1 and tumor size were not significant factors (Table 3).
The prognostic value of Ki67 in subgroups of ER status and histological grade
When stratifying for ER status, there was a strong negative effect of high Ki67 in the ER-positive group (hazard ratio: 5.0, 95% confidence interval: 1.8–14, P=0.002), but not in the ER-negative group (hazard ratio: 0.90, 95% confidence interval: 0.34–2.4, P=0.83) (Figures 2a and b). The negative prognostic impact of Ki67 in ER-positive patients remained significant after adjustment for HER2, age, and tumor size, even though it is questionable to fit a Cox-model with four covariates to a subset of patients with only 15 events. However, the same conclusion was drawn from three bivariate analyses including Ki67 and one of the other covariates Ki67 adds prognostic information. Models with both Ki67 and histological grade or Ki67 and PR were not considered because of colinearity. The differential prognostic effect of Ki67 in ER-positive and ER-negative patients was further analyzed, and found to differ significantly corresponding to a significant interaction term (hazard ratio: 5.5, 95% confidence interval: 1.4–22, P=0.02).
A strong negative effect of high Ki67 was also seen in patients with histological grade 2 (hazard ratio: 15, 95% confidence interval: 3.8–58, P<0.001), with distant recurrence rates for the low- and high-risk groups of 5% (3/56) and 54% (7/13), respectively, corresponding to a relative risk of 10 (Figure 3b). However, in histological grade 1 (log-rank, P=0.54) and histological grade 3 (log-rank, P=0.21), Ki67 was not a significant prognostic factor (Figures 3a and c). The negative prognostic impact of Ki67 in histological grade 2 remained significant (P≤0.001) in a series of bivariate models adjusting for HER2, age, and tumor size.
Multivariate analyses
In a series of bivariate models fitted for the entire patient population, the prognostic impact of Ki67 remained significant after adjustment for HER2, age, and tumor size. Models combining Ki67 with ER, PR, or histological grade were not considered because of colinearity. When adjusting simultaneously for HER2, age, and tumor size (Table 4), Ki67 was not a significant prognostic factor (hazard ratio: 1.9, 95% confidence interval: 0.89–4.2, P=0.09). Also, PR and histological grade (3 vs 1+2 or 2+3 vs 1) were insignificant if substituted, one at a time, for Ki67 in the multivariate model presented in Table 4 (data not shown). The multivariate analysis including Ki67, HER2, age, and tumor size was repeated for the 87% of the patients who had received no adjuvant medical treatment (n=169, 21 distant recurrences, Table 4). In this subgroup, Ki67 was an independent prognostic factor for distant disease-free survival (hazard ratio: 3.0, 95% confidence interval: 1.2–8.0, P=0.023) together with HER2 and age. Histological grade was, however, not an independent prognostic factor in this subgroup after adjustment for HER2, age, and tumor size (P=0.08 for grade 3 vs 1+2 and P=0.57 for grade 2+3 vs 1).
Overall Survival
Of the 16 patients who died within 5 years, 15 died of breast cancer and the overall survival at 5 years was 92% (95% confidence interval: 87–95%). In univariate analysis, Ki67 was a significant prognostic factor for overall survival (hazard ratio: 4.9, 95% confidence interval: 1.7–14, P=0.003) together with HER2, histological grade, PR, ER, tumor size, and age (data not shown).
When stratifying for ER status, there was a strong negative effect by Ki67 in the ER-positive group (log-rank, P=0.0007), but not in the ER-negative group (log-rank, P=0.60). The same results were seen when stratifying for histological grade, in which Ki67 had a strong negative impact in the group with histological grade 2 (log-rank, P<0.0001), but not in histological grades 1 and 3.
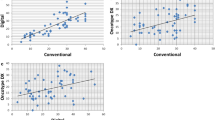
Relationship between three Independent Readers Using Semi-Quantitative or Quantitative assessments of Ki67 and Correlation to Distant Disease-free Survival in Univariate Analysis
Of the 200 cases assessed semi-quantitatively (DG), 183 cases were scored independently by all three investigators. The remaining 17 cases were considered non-evaluable by either one or two of the other investigators. Using the seventh decile,18 equivalent to a cut-point of >20% positively stained tumor cells defined by the semi-quantitative method, 33% of the 183 patients had a high proliferation index, leading to cut-points of 14.2% (KL), and 18.1% (MK) for the two readers performing quantitative assessments. The pairwise level of agreement between the three investigators was between 92 and 95%, with corresponding κ-values of 0.83–0.88 (Table 5). In a second analysis, the reference cut-point of 20% was applied on the results from all three investigators, with levels of agreement between 89 and 93%, and corresponding κ-values of 0.73–0.82. In univariate analysis, Ki67 was a significant prognostic factor for distant disease-free survival for all three investigators using either cut-point (hazard ratios: 2.7–3.2, data not shown).
Discussion
This study confirms that Ki67 is a prognostic marker for distant recurrence5, 6, 7, 18, 19, 21, 22 and overall survival5, 6, 7, 17, 18, 20, 21, 22 in lymph node-negative breast cancer. Interestingly, it only adds prognostic information in the ER-positive group and in patients with histological grade 2, the latter which to our knowledge no earlier study on Ki67 has addressed. These results are in line with those obtained with gene array tests.11, 12, 13, 14, 15, 16 In the initial classification of breast cancers,11 which also later subdivided ER-positive disease,14 the largest cluster of genes are those of proliferation, including Ki67. In the 70-gene ‘poor prognosis’ signature,15 proliferation also dominates. In the 21-gene Recurrence Score,13 developed for ER-positive, lymph node-negative, tamoxifen-treated patients, the main driving force is proliferation, with Ki67 being one of the 21 genes. For ER-negative breast cancer, the expression levels of complement and immune response pathway genes have instead been shown to be more important for clinical outcome.25 Even though our patient material is not equivalent to the patient material in the above-mentioned studies, it nevertheless suggests that a division of ER-positive disease can be achieved by merely analyzing one marker of proliferation, in line with another recent publication on Ki67.22
Histological grade was not an independent prognostic factor in this study, not even in the subgroup of medically untreated patients, in which Ki67 was of independent prognostic value. Because of studies showing interobserver variability,13, 26, 27 the value of histological grade has been questioned. Furthermore, between 30 and 60% of patients will be classified as histological grade 2, a group with intermediate and variable prognosis, which constitutes a problem when selecting adjuvant medical treatment. In our study, 35% of the patients were classified as histological grade 2, and by stratifying for Ki67, we were able to divide the patients in two groups with significant differences in prognosis. This has further support in gene expression profiling studies, in which genetic signatures have been identified, which reclassify patients with histological grade 2 into two groups with significant differences in prognosis, similar to the prognosis of patients with histological grades 1 and 3.12, 16 These signatures contain a number of genes involved in proliferation, and our study suggests, in analogy with ER-positive disease, that similar results can be achieved merely by looking at one marker of proliferation, Ki67.
In the entire patient population, neither histological grade nor Ki67 were independent prognostic factors, but in the patients not treated with systemic adjuvant therapy, Ki67 was an independent prognostic factor. The independent prognostic value of Ki67 has also been lost in prior studies with populations <200.7 Had our study included more patients, Ki67 might have proven to be an independent prognostic factor in the entire population. Of note is also that in the subgroup analyses of the ER-positive patients and the patients with histological grade 2, in which Ki67 is a significant prognostic factor, there are limited numbers of events (15 and 10, respectively), which has lead to broad confidence intervals.
Because of non-proportional hazards, the follow-up in this study was restricted to 5 years, even though all patients alive and free from distant recurrences at 5 years have additional follow-up. As earlier publications have noted, the estimated effects of several prognostic factors will decrease when extending the follow-up.28 However, in one publication presenting 10 years follow-up data, only Ki67 was a significant prognostic factor in a cohort of T1, node-negative breast.29 This is, however, mainly because of the fact that the negative prognostic effect of high Ki67 seen the first 5 years is so strong that the impact with 10 years of follow-up remains significant although the effect is non-existing or even weakly positive between 5 and 10 years.
The importance of proliferation in tumor behavior and prognosis has been established in studies on other markers of proliferation. Thymidine labeling index has reached the highest level of evidence but the use of fresh tissue and radioactive isotopes makes it hard to apply routinely.10 S-phase fraction has also been evaluated prospectively,9 but there have been concerns about reproducibility, tumor heterogeneity, and contamination of normal cells. For different cyclins as well as cyclin inhibitors p21 and p27, reports are fewer, and to some extent contradictory and methodological standardization is lacking.4, 5, 18 No proliferation markers have been recommended for clinical use, mainly because of low levels of evidence or methodological difficulties,1, 2, 3 with the exception of Ki67 and mitotic activity, recently recommended by one guideline.3 Problems with reproducibility have, however, been reported with mitotic activity.26, 27 As far as Ki67 is concerned, we found a good correlation between three readers as well as between manual counting and semi-quantitative analysis, in line with earlier publications.19
Evaluation of Ki67 can be done both on whole section17, 19, 20, 21, 22, 30 and tissue microarray.18 We chose tissue microarray as it is less time consuming, allows assessments of large numbers of tumors on a single slide, and as earlier studies have shown a good agreement of Ki67 quantification between tissue microarray and large section.31, 32 Our findings support the use of Ki67 as a reproducible, easily assessed marker of proliferation. Another advantage with Ki67 is that paraffin-embedded material can be used, whereas multigene assays need fresh frozen tissue,11, 12, 14, 15, 16 with the exception of the 21-gene Recurrence Score.13
The predefined cutoff we chose, 20%, set at the seventh decile, is within the range of cutoffs from earlier published studies (5–30%), defined as optimized cut-points, median cut-points, or categorization in three groups.3, 17, 18, 19, 20, 22, 30 Optimal cutoffs of 25% for high-grade tumors sensitive to chemotherapy, and 10% for slowly proliferating tumors have been suggested.30 In line with the results in an earlier publication, a cutoff at the seventh decile defines a high-risk population, likely to benefit from adjuvant chemotherapy.18
In summary, this study confirms the prognostic value of Ki67 in node-negative breast cancer, but it also reveals that the prognostic impact is restricted to ER-positive tumors and histological grade 2. There are many markers of proliferation, but Ki67 is an affordable, reproducible and easily assessed technique, and also has the advantage that it can be assessed on paraffin-embedded tumor material. Taken together, Ki67 might be clinically helpful for prognostic considerations as an alternative or complement to histological grade and for selection of patients for adjuvant medical treatment.
References
Harris L, Fritsche H, Mennel R, et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007;25:5287–5312.
Eifel P, Axelson JA, Costa J, et al. National Institutes of Health Consensus Development Conference Statement: adjuvant therapy for breast cancer, November 1–3, 2000. J Natl Cancer Inst 2001;93:979–989.
Goldhirsch A, Ingle JN, Gelber RD, et al. Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2009. Ann Oncol 2009;20:1319–1329.
Beresford MJ, Wilson GD, Makris A . Measuring proliferation in breast cancer: practicalities and applications. Breast Cancer Res 2006;8:216.
Colozza M, Azambuja E, Cardoso F, et al. Proliferative markers as prognostic and predictive tools in early breast cancer: where are we now? Ann Oncol 2005;16:1723–1739.
de Azambuja E, Cardoso F, de Castro Jr G, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer 2007;96:1504–1513.
Urruticoechea A, Smith IE, Dowsett M . Proliferation marker Ki-67 in early breast cancer. J Clin Oncol 2005;23:7212–7220.
Brown DC, Gatter KC . Ki67 protein: the immaculate deception? Histopathology 2002;40:2–11.
Malmstrom P, Bendahl PO, Boiesen P, et al. S-phase fraction and urokinase plasminogen activator are better markers for distant recurrences than Nottingham Prognostic Index and histologic grade in a prospective study of premenopausal lymph node-negative breast cancer. J Clin Oncol 2001;19:2010–2019.
Silvestrini R, Daidone MG, Luisi A, et al. Biologic and clinicopathologic factors as indicators of specific relapse types in node-negative breast cancer. J Clin Oncol 1995;13:697–704.
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000;406:747–752.
Ivshina AV, George J, Senko O, et al. Genetic reclassification of histologic grade delineates new clinical subtypes of breast cancer. Cancer Res 2006;66:10292–10301.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 2004;351:2817–2826.
Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 2001;98:10869–10874.
van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature 2002;415:530–536.
Sotiriou C, Wirapati P, Loi S, et al. Gene expression profiling in breast cancer: understanding the molecular basis of histologic grade to improve prognosis. J Natl Cancer Inst 2006;98:262–272.
Railo M, Lundin J, Haglund C, et al. Ki-67, p53, ER receptors, ploidy and S phase as long-term prognostic factors in T1 node-negative breast cancer. Tumour Biol 2007;28:45–51.
Ahlin C, Aaltonen K, Amini RM, et al. Ki67 and cyclin A as prognostic factors in early breast cancer. What are the optimal cut-off values? Histopathology 2007;51:491–498.
Brown RW, Allred CD, Clark GM, et al. Prognostic value of Ki-67 compared to S-phase fraction in axillary node-negative breast cancer. Clin Cancer Res 1996;2:585–592.
Pinder SE, Wencyk P, Sibbering DM, et al. Assessment of the new proliferation marker MIB1 in breast carcinoma using image analysis: associations with other prognostic factors and survival. Br J Cancer 1995;71:146–149.
Rudolph P, Alm P, Heidebrecht HJ, et al. Immunologic proliferation marker Ki-S2 as prognostic indicator for lymph node-negative breast cancer. J Natl Cancer Inst 1999;91:271–278.
Jung SY, Han W, Lee JW, et al. Ki-67 Expression gives additional prognostic information on St. Gallen 2007 and adjuvant! Online risk categories in early breast cancer. Ann Surg Oncol 2009;16:1112–1121.
Elston CW, Ellis IO . Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 1991;19:403–410.
Schoenfeld D . Partial residuals for the proportional hazards regression model. Biometrika 1982;69:239–241.
Teschendorff AE, Miremadi A, Pinder SE, et al. An immune response gene expression module identifies a good prognosis subtype in estrogen receptor negative breast cancer. Genome Biol 2007;8:R157.
Harvey JM, de Klerk NH, Sterrett GF . Histological grading in breast cancer: interobserver agreement, and relation to other prognostic factors including ploidy. Pathology 1992;24:63–68.
Boiesen P, Bendahl PO, Anagnostaki L, et al. Histologic grading in breast cancer--reproducibility between seven pathologic departments. South Sweden Breast Cancer Group. Acta Oncol 2000;39:41–45.
Hilsenbeck SG, Ravdin PM, de Moor CA, et al. Time-dependence of hazard ratios for prognostic factors in primary breast cancer. Breast Cancer Res Treat 1998;52:227–237.
Railo M, Lundin J, Haglund C, et al. Ki-67, p53, Er-receptors, ploidy and S-phase as prognostic factors in T1 node negative breast cancer. Acta Oncol 1997;36:369–374.
Spyratos F, Ferrero-Pous M, Trassard M, et al. Correlation between MIB-1 and other proliferation markers: clinical implications of the MIB-1 cutoff value. Cancer 2002;94:2151–2159.
Nocito A, Bubendorf L, Tinner EM, et al. Microarrays of bladder cancer tissue are highly representative of proliferation index and histological grade. J Pathol 2001;194:349–357.
Ruiz C, Seibt S, Al Kuraya K, et al. Tissue microarrays for comparing molecular features with proliferation activity in breast cancer. Int J Cancer 2006;118:2190–2194.
Acknowledgements
We are indebted to participating departments of the South Sweden Breast Cancer Group for providing samples and clinical follow-up. The study was supported by funds from the Swedish Cancer Society, the Swedish Research Council, the Gunnar Nilsson Cancer Foundation, the Mrs Berta Kamprad Foundation, Skåne County Council's Research and Development Foundation, and Governmental Funding of Clinical Research within the National Health Service.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Disclosure/conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Klintman, M., Bendahl, PO., Grabau, D. et al. The prognostic value of Ki67 is dependent on estrogen receptor status and histological grade in premenopausal patients with node-negative breast cancer. Mod Pathol 23, 251–259 (2010). https://doi.org/10.1038/modpathol.2009.167
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2009.167
Keywords
This article is cited by
-
Identifying accessible prognostic factors for breast cancer relapse: a case-study on 405 histologically confirmed node-negative patients
World Journal of Surgical Oncology (2017)
-
Ki-67 is a prognostic marker for hormone receptor positive tumors
Clinical and Translational Oncology (2016)
-
Influence of BCL2-938 C>A promoter polymorphism and BCL2 gene expression on the progression of breast cancer
Tumor Biology (2016)
-
Invasive lobular carcinoma of the breast: long-term prognostic value of Ki67 and histological grade, alone and in combination with estrogen receptor
SpringerPlus (2014)
-
Association between insulin-like growth factor-1 receptor (IGF1R) negativity and poor prognosis in a cohort of women with primary breast cancer
BMC Cancer (2014)