Abstract
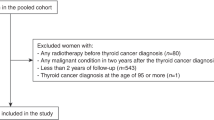
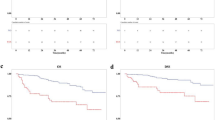
Exposure to ionizing radiation increases the risk of myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN), but such risks are not known in well-differentiated thyroid cancer (WDTC) patients treated with radioactive iodine (RAI). A total of 148 215 WDTC patients were identified from Surveillance, Epidemiology and End Results registries between 1973 and 2014, of whom 54% underwent definitive thyroidectomy and 46% received adjuvant RAI. With a median follow-up of 6.6 years, 77 and 66 WDTC patients developed MDS and MPN, respectively. Excess absolute risks for MDS and MPN from RAI treatment when compared to background rates in the US population were 6.6 and 8.1 cases per 100 000 person-years, respectively. Compared to background population rates, relative risks of developing MDS (3.85 (95% confidence interval, 1.7–7.6); P=0.0005) and MPN (3.13 (1.1–6.8); P=0.012) were significantly elevated in the second and third year following adjuvant RAI therapy, but not after thyroidectomy alone. The increased risk was significantly associated with WDTC size ⩾2 cm or regional disease. Development of MDS was associated with shorter median overall survival in WDTC survivors (10.3 vs 22.5 years; P<0.001). These data suggest that RAI treatment for WDTC is associated with increased risk of MDS with short latency and poor survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
La Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer 2015; 136: 2187–2195.
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM . Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA 2017; 317: 1338–1348.
Surveillance, Epidemiology, and End Results (SEER) Program (Research Data (1973–2014), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2017, based on the November 2016 submission). Available at: http://www.seer.cancer.gov.
Nixon IJ, Ganly I, Patel SG, Palmer FL, Di Lorenzo MM, Grewal RK et al. The results of selective use of radioactive iodine on survival and on recurrence in the management of papillary thyroid cancer, based on Memorial Sloan-Kettering Cancer Center risk group stratification. Thyroid 2013; 23: 683–694.
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al. American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016 2015; 26: 1–133.
Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med 2012; 366: 1674–1685.
Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B et al. Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 2012; 366: 1663–1673.
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer Cooper DS American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer Doherty GM American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer Haugen BR American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer Kloos RT American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer Lee SL et alAmerican Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009; 19: 1167–1214.
Iyer NG, Morris LG, Tuttle RM, Shaha AR, Ganly I . Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 2011; 117: 4439–4446.
Teng CJ, Hu YW, Chen SC, Yeh CM, Chiang HL, Chen TJ et al. Use of radioactive iodine for thyroid cancer and risk of second primary malignancy: a nationwide population-based study. J Natl Cancer Inst 2016; 108: 2.
Sawka AM, Thabane L, Parlea L, Ibrahim-Zada I, Tsang RW, Brierley JD et al. Second primary malignancy risk after radioactive iodine treatment for thyroid cancer: a systematic review and meta-analysis. Thyroid 2009; 19: 451–457.
Subramanian S, Goldstein DP, Parlea L, Thabane L, Ezzat S, Ibrahim-Zada I et al. Second primary malignancy risk in thyroid cancer survivors: a systematic review and meta-analysis. Thyroid 2007; 17: 1277–1288.
Klimek VM, Tray NJ . Therapy-related myeloid neoplasms: what's in a name? Curr Opin Hematol 2016; 23: 161–166.
Hsu WL, Preston DL, Soda M, Sugiyama H, Funamoto S, Kodama K et al. The incidence of leukemia, lymphoma and multiple myeloma among atomic bomb survivors: 1950-2001. Radiat Res 2013; 179: 361–382.
Iwanaga M, Hsu WL, Soda M, Takasaki Y, Tawara M, Joh T et al. Risk of myelodysplastic syndromes in people exposed to ionizing radiation: a retrospective cohort study of Nagasaki atomic bomb survivors. J Clin Oncol 2011; 29: 428–434.
Radivoyevitch T, Sachs RK, Gale RP, Molenaar RJ, Brenner DJ, Hill BT et al. Defining AML and MDS second cancer risk dynamics after diagnoses of first cancers treated or not with radiation. Leukemia 2016; 30: 285–294.
Lassmann M, Reiners C, Luster M . Dosimetry and thyroid cancer: the individual dosage of radioiodine. Endocr Relat Cancer 2010; 17: R161–R172.
Altman DG, Bland JM . How to obtain the confidence interval from a P value. BMJ 2011; 343: d2090.
R Core Team. R: A Language And Environment For Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2017..
Nardi V, Winkfield KM, Ok CY, Niemierko A, Kluk MJ, Attar EC et al. Acute myeloid leukemia and myelodysplastic syndromes after radiation therapy are similar to de novo disease and differ from other therapy-related myeloid neoplasms. J Clin Oncol 2012; 30: 2340–2347.
Barrington SF, Kettle AG, O'Doherty MJ, Wells CP, Somer EJ, Coakley AJ . Radiation dose rates from patients receiving iodine-131 therapy for carcinoma of the thyroid. Eur J Nucl Med 1996; 23: 123–130.
Ravichandran R, Binukumar J, Saadi AA . Estimation of effective half life of clearance of radioactive Iodine (I) in patients treated for hyperthyroidism and carcinoma thyroid. Indian J Nucl Med 2010; 25: 49–52.
Monteiro Gil O, Oliveira NG, Rodrigues AS, Laires A, Ferreira TC, Limbert E et al. Cytogenetic alterations and oxidative stress in thyroid cancer patients after iodine-131 therapy. Mutagenesis 2000; 15: 69–75.
Erselcan T, Sungu S, Ozdemir S, Turgut B, Dogan D, Ozdemir O . Iodine-131 treatment and chromosomal damage: in vivo dose-effect relationship. Eur J Nucl Med Mol Imaging 2004; 31: 676–684.
de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev 2013; 22: 561–570.
Rollison DE, Howlader N, Smith MT, Strom SS, Merritt WD, Ries LA et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001-2004, using data from the NAACCR and SEER programs. Blood 2008; 112: 45–52.
Gillis NK, Ball M, Zhang Q, Ma Z, Zhao Y, Yoder SJ et al. Clonal haemopoiesis and therapy-related myeloid malignancies in elderly patients: a proof-of-concept, case-control study. Lancet Oncol 2017; 18: 112–121.
Takahashi K, Wang F, Kantarjian H, Doss D, Khanna K, Thompson E et al. Preleukaemic clonal haemopoiesis and risk of therapy-related myeloid neoplasms: a case-control study. Lancet Oncol 2017; 18: 100–111.
Wong TN, Ramsingh G, Young AL, Miller CA, Touma W, Welch JS et al. Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature 2015; 518: 552–555.
Keegan THM, Bleyer A, Rosenberg AS, Li Q, Goldfarb M . Second primary malignant neoplasms and survival in adolescent and young adult cancer survivors. JAMA Oncol 2017; 3: 1554–1557.
Sidana S, Elson P, Gerds AT, Carraway HE, Advani AS, Saunthararajah Y et al. Survival outcomes of leukemias and myelodysplastic syndromes occurring as second cancers in the United States: A SEER registry-based population analysis. Blood 2015; 126: 2507.
Jagsi R, Abrahamse P, Hawley ST, Graff JJ, Hamilton AS, Katz SJ . Underascertainment of radiotherapy receipt in Surveillance, Epidemiology, and End Results registry data. Cancer 2012; 118: 333–341.
Veiga LH, Lubin JH, Anderson H, de Vathaire F, Tucker M, Bhatti P et al. A pooled analysis of thyroid cancer incidence following radiotherapy for childhood cancer. Radiat Res 2012; 178: 365–376.
Schneider AB, Sarne DH . Long-term risks for thyroid cancer and other neoplasms after exposure to radiation. Nat Clin Pract Endocrinol Metab 2005; 1: 82–91.
Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM et al. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 1995; 141: 259–277.
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505.
Acknowledgements
IRB approval (also in main manuscript text): The Cleveland Clinic Institutional Review Board has deemed studies using de-identified, publicly available data (such as those used herein) to be exempt from Institutional Review Board review.
Author contributions
All authors were involved in the preparation of this report. SM is the principal investigator who generated the study hypothesis and was involved in all aspects of the study, including study design, interpretation and writing of the report. RJM contributed to the study design, collecting data, analyzing data, interpreting data and writing of the report. TR contributed to designing the methodology and analyzing data. CP, AN, HEC, MK, DA, CN, DA, JPM, NM and MAS were involved in study design, data interpretation and guiding the research. All authors read and approved the manuscript before submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Molenaar, R., Pleyer, C., Radivoyevitch, T. et al. Risk of developing chronic myeloid neoplasms in well-differentiated thyroid cancer patients treated with radioactive iodine. Leukemia 32, 952–959 (2018). https://doi.org/10.1038/leu.2017.323
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2017.323
This article is cited by
-
In utero origin of myelofibrosis presenting in adult monozygotic twins
Nature Medicine (2022)
-
Incidence rate and factors associated with the development of secondary cancers after radioiodine therapy in differentiated thyroid cancer: a multicenter retrospective study
European Journal of Nuclear Medicine and Molecular Imaging (2022)
-
Second primary malignancy risk in thyroid cancer and matched patients with and without radioiodine therapy analysis from the observational health data sciences and informatics
European Journal of Nuclear Medicine and Molecular Imaging (2022)
-
Risk of hematologic malignancies after breast ductal carcinoma in situ treatment with ionizing radiation
npj Breast Cancer (2021)
-
Errare humanum est, sed in errare perseverare diabolicum: methodological errors in the assessment of the relationship between I-131 therapy and possible increases in the incidence of malignancies
European Journal of Nuclear Medicine and Molecular Imaging (2020)