Abstract
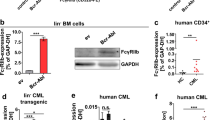
Myeloid and lymphoid malignancies associated with fibroblast growth factor receptor-1 (FGFR1) abnormalities are characterized by constitutively activated FGFR1 kinase and rapid transformation to acute myeloid leukemia and lymphoblastic lymphoma. Molecular targeted therapies have not been widely used for stem cell leukemia/lymphoma (SCLL). Ponatinib (AP24534), which potently inhibits native and mutant BCR-ABL, also targets the FGFR family. Using murine BaF3 cells, stably transformed with six different FGFR1 fusion genes, as well as human KG1 cells expressing activated chimeric FGFR1 and five newly established murine SCLL cell lines, we show that ponatinib (<50 nM) can effectively inhibit phosphoactivation of the fusion kinases and their downstream effectors, such as PLCγ, Stat5 and Src. Ponatinib also significantly extended survival of mice transplanted with different SCLL cell lines. Ponatinib administered at 30 mg/kg daily also significantly delayed, or even prevented, tumorigenesis of KG1 cells in xenotransplanted mice. Furthermore, we demonstrate that ponatinib specifically inhibits cell growth and clonogenicity of normal human CD34+ progenitor cells transformed by chimeric FGFR1 fusion kinases. Overall, our data provide convincing evidence to suggest that pharmacologic inhibition of FGFR1 fusion kinases with ponatinib is likely to be beneficial for patients with SCLL and perhaps for other human disorders associated with dysregulated FGFR1 activity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Vega F, Medeiros LJ, Davuluri R, Cromwell CC, Alkan S, Abruzzo LV . t(8;13)-Positive bilineal lymphomas: report of 6 cases. Am J Surg Pathol 2008; 32: 14–20.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009; 114: 937–951.
Baumann H, Kunapuli P, Tracy E, Cowell JK . The oncogenic fusion protein-tyrosine kinase ZNF198/fibroblast growth factor receptor-1 has signaling function comparable with interleukin-6 cytokine receptors. J Biol Chem 2003; 278: 16198–16208.
Chen J, Deangelo DJ, Kutok JL, Williams IR, Lee BH, Wadleigh M et al. PKC412 inhibits the zinc finger 198-fibroblast growth factor receptor 1 fusion tyrosine kinase and is active in treatment of stem cell myeloproliferative disorder. Proc Natl Acad Sci USA 2004; 101: 14479–14484.
Dong S, Kang S, Gu TL, Kardar S, Fu H, Lonial S et al. 14-3-3 Integrates prosurvival signals mediated by the AKT and MAPK pathways in ZNF198-FGFR1-transformed hematopoietic cells. Blood 2007; 110: 360–369.
Roumiantsev S, Krause DS, Neumann CA, Dimitri CA, Asiedu F, Cross NC et al. Distinct stem cell myeloproliferative/T lymphoma syndromes induced by ZNF198-FGFR1 and BCR-FGFR1 fusion genes from 8p11 translocations. Cancer Cell 2004; 5: 287–298.
Ren M, Qin H, Ren R, Tidwell J, Cowell JK . Src activation plays an important key role in lymphomagenesis induced by FGFR1 fusion kinases. Cancer Res 2011; 71: 7312–7322.
Holroyd A, Cross NC, Macdonald DH . The two faces of myeloproliferative neoplasms: Molecular events underlying lymphoid transformation. Leuk Res 2011; 35: 1279–1285.
Ren M, Li X, Cowell JK . Genetic fingerprinting of the development and progression of T-cell lymphoma in a murine model of atypical myeloproliferative disorder initiated by the ZNF198-fibroblast growth factor receptor-1 chimeric tyrosine kinase. Blood 2009; 114: 1576–1584.
Ren M, Cowell JK . Constitutive Notch pathway activation in murine ZMYM2-FGFR1-induced T-cell lymphomas associated with atypical myeloproliferative disease. Blood 2011; 117: 6837–6847.
Wong WS, Cheng KC, Lau KM, Chan NP, Shing MM, Cheng SH et al. Clonal evolution of 8p11 stem cell syndrome in a 14-year-old Chinese boy: a review of literature of t(8;13) associated myeloproliferative diseases. Leuk Res 2007; 31: 235–238.
Abruzzo LV, Jaffe ES, Cotelingam JD, Whang-Peng J, Del Duca V, Medeiros LJ . T-cell lymphoblastic lymphoma with eosinophilia associated with subsequent myeloid malignancy. Am J Surg Pathol 1992; 16: 236–245.
Inhorn RC, Aster JC, Roach SA, Slapak CA, Soiffer R, Tantravahi R et al. A syndrome of lymphoblastic lymphoma, eosinophilia, and myeloid hyperplasia/malignancy associated with t(8;13)(p11;q11): description of a distinctive clinicopathologic entity. Blood 1995; 85: 1881–1887.
Macdonald D, Aguiar RC, Mason PJ, Goldman JM, Cross NC . A new myeloproliferative disorder associated with chromosomal translocations involving 8p11: a review. Leukemia 1995; 9: 1628–1630.
Jackson CC, Medeiros LJ, Miranda RN . 8p11 myeloproliferative syndrome: a review. Hum Pathol 2010; 41: 461–476.
Turner N, Grose R . Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer 2010; 10: 116–129.
Chase A, Grand FH, Cross NC . Activity of TKI258 against primary cells and cell lines with FGFR1 fusion genes associated with the 8p11 myeloproliferative syndrome. Blood 2007; 110: 3729–3734.
Wasag B, Lierman E, Meeus P, Cools J, Vandenberghe P . The kinase inhibitor TKI258 is active against the novel CUX1-FGFR1 fusion detected in a patient with T-lymphoblastic leukemia/lymphoma and t(7;8)(q22;p11). Haematologica 2011; 96: 922–926.
O′Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F et al. AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell 2009; 16: 401–412.
Darzynkiewicz Z, Juan G . Analysis of DNA content and BrdU incorporation. Curr Protoc Cytom 2001; Chapter 7: Unit 7.7.
Ren M, Tidwell JA, Sharma S, Cowell JK . Acute progression of BCR-FGFR1 induced murine B-lympho/myeloproliferative disorder suggests involvement of lineages at the pro-B cell stage. PLoS One 2012; 7: e38265.
Mohammadi M, Honegger AM, Rotin D, Fischer R, Bellot F, Li W et al. A tyrosine-phosphorylated carboxy-terminal peptide of the fibroblast growth factor receptor (Flg) is a binding site for the SH2 domain of phospholipase C-gamma 1. Mol Cell Biol 1991; 11: 5068–5078.
Furley AJ, Reeves BR, Mizutani S, Altass LJ, Watt SM, Jacob MC et al. Divergent molecular phenotypes of KG1 and KG1a myeloid cell lines. Blood 1986; 68: 1101–1107.
Choi S, Choi HH, Choi JH, Yoon BH, You HJ, Hyun JW et al. Inhibitory effect of 8-oxo-7,8-dihydro-2′-deoxyguanosine on the growth of KG-1 myelosarcoma in Balb/c nude mice. Leuk Res 2006; 30: 1425–1436.
Machado EA, Gerard DA, Lozzio CB, Lozzio BB, Mitchell JR, Golde DW . Proliferation and differentiation of human myeloid leukemic cells in immunodeficient mice: electron microscopy and cytochemistry. Blood 1984; 63: 1015–1022.
Suciu-Foca N, Feirt N, Zhang QY, Vlad G, Liu Z, Lin H et al. Soluble Ig-like transcript 3 inhibits tumor allograft rejection in humanized SCID mice and T cell responses in cancer patients. J Immunol 2007; 178: 7432–7441.
Gozgit JM, Wong MJ, Wardwell S, Tyner JW, Loriaux MM, Mohemmad QK et al. Potent activity of ponatinib (AP24534) in models of FLT3-driven acute myeloid leukemia and other hematologic malignancies. Mol Cancer Ther 2011; 10: 1028–1035.
Gozgit JM, Wong MJ, Moran L, Wardwell S, Mohemmad QK, Narasimhan NI et al. Ponatinib (AP24534), a multi-targeted pan-FGFR inhibitor with activity in multiple FGFR-amplified or mutated cancer models. Mol Cancer Ther 2012; 11: 690–699.
Dean M, Fojo T, Bates S . Tumour stem cells and drug resistance. Nat Rev Cancer 2005; 5: 275–284.
Acknowledgements
We are grateful to Dr Els Lierman for providing the CUX1-FGFR1 vector. Ponatinib was kindly provided by Ariad Pharmaceuticals Inc. This work was supported by Grant CA076167 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Ren, M., Qin, H., Ren, R. et al. Ponatinib suppresses the development of myeloid and lymphoid malignancies associated with FGFR1 abnormalities. Leukemia 27, 32–40 (2013). https://doi.org/10.1038/leu.2012.188
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2012.188
Keywords
This article is cited by
-
Identification of a novel HOOK3-FGFR1 fusion gene involved in activation of the NF-kappaB pathway
Cancer Cell International (2022)
-
A truncated derivative of FGFR1 kinase cooperates with FLT3 and KIT to transform hematopoietic stem cells in syndromic and de novo AML
Molecular Cancer (2022)
-
IRAK1-regulated IFN-γ signaling induces MDSC to facilitate immune evasion in FGFR1-driven hematological malignancies
Molecular Cancer (2021)
-
Downregulation of PUMA underlies resistance to FGFR1 inhibitors in the stem cell leukemia/lymphoma syndrome
Cell Death & Disease (2020)
-
FGFR1 fusion kinase regulation of MYC expression drives development of stem cell leukemia/lymphoma syndrome
Leukemia (2018)