Abstract
Papillary thyroid carcinoma (PTC) accounts for >80% thyroid malignancies, and BRAFV600E mutation is frequently found in >40% PTC. Interleukin-12 (IL-12) is a proinflammatory heterodimeric cytokine with strong antitumor activity. It is not known whether IL-12 immunotherapy is effective against BrafV600E-induced PTC. In the present study, we investigated the effectiveness of IL-12 immunotherapy against BrafV600E-induced PTC in LSL-BrafV600E/TPO-Cre mice. LSL-BrafV600E/TPO-Cre mice were created for thyroid-specific expression of BrafV600E under the endogenous Braf promoter, and spontaneous PTC developed at about 5 weeks of age. The mice were subjected to two treatment regimens: (1) weekly intramuscular injection of 50 μg plasmid DNA expressing a single-chain IL-12 fusion protein (scIL-12/CMVpDNA), (2) daily intraperitoneal injection of mouse recombinant IL-12 protein (mrIL-12, 100 ng per day). The role of T cells, natural killer (NK) cells, and transforming growth factor-β (TGF-β) in IL-12-mediated antitumor effects was determined by a 51Cr-release cytotoxicity assay. Tumor size and weight were significantly reduced by either weekly intramuscular injection of scIL-12/CMVpDNA or daily intraperitoneal injection of mrIL-12, and tumor became more localized. Survival was significantly increased when treatment started at 1 week of age as compared with that at the 6 weeks of age. Both NK and CD8+ T cells were involved in the cytotoxicity against tumor cells and their antitumor activity was significantly reduced in tumor-bearing mice. TGF-β also inhibited the antitumor activity of NK and CD8+ T cells. The immune suppression was completely reversed by IL-12 treatment and partially recovered by anti-TGF-β antibody. We conclude that both IL-12 gene therapy and recombinant protein therapy are effective against PTC. Given that the immune response is significantly suppressed in tumor-bearing mice and can be restored by IL-12, the current study raises a possibility of the application of IL-12 as an adjuvant therapy for thyroid cancer.
Similar content being viewed by others
Main
Thyroid cancer is the most common malignancy in the endocrine system and its incidence has been rising in recent years.1 It is commonly classified into papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC), and anaplastic thyroid carcinoma (ATC). PTC is the most common type of differentiated thyroid carcinoma, accounting for >80% of thyroid malignancies.2 Differentiated (PTC and FTC) thyroid cancer has relatively good prognosis, whereas ATC is highly aggressive and most patients die within 1 year of the diagnosis. Most differentiated thyroid cancers can be cured by surgery and 131I therapy. However, 10–20% of patients die from recurrence or progression into poorly differentiated tumors refractory to classical treatments such as suppression of serum thyroid-stimulating hormone by thyroxine following surgery and radioiodine therapy.3, 4, 5 To treat these patients, it becomes necessary to search for new treatment strategies such as tyrosine kinase inhibitors and immunotherapy.
BRAFV600E mutation is frequently found in PTC with an overall rate of 42% and has been associated with recurrence and poor prognosis.6 To treat patients with recurrent or poorly differentiated PTC, novel approaches have been explored: for example, by targeting RAS–RAF–MEK–ERK MAP kinase signaling pathway using Sorafenib (BAY 43-9006, an inhibitor of multiple receptor tyrosine kinases),7, 8, 9, 10 vascular endothelial growth factor receptor signaling using Lenvatinib,11 or targeting AKT/mammalian target of rapamycin pathway.12 Although these approaches produced promising results, and Sorafenib and Lenvatinib have been approved recently by FDA for the treatment of patients with recurrent or metastatic radioactive iodine-refractory differentiated thyroid cancer, immunotherapy has not been explored in these patients. In our previous studies, we have demonstrated that IL-12 is effective against ATC in a mouse xenograft model.13 The antitumor activity of IL-12 has not been investigated in genetically engineered mouse models, which are often regarded as superior to the xenograft models.14 As CD8+ T cells has important roles in IL-12-mediated antitumor activity and athymic nude mice have no functional T cells, the effects of IL-12-mediated antitumor activity could not be fully appreciated in the nude mice xenograft model.
Genetically engineered BrafV600E mouse models have been developed recently.15, 16, 17 Thyroid expression of BrafV600E leads to malignant transformation of thyroid epithelial cells to PTC and rapid progression to poorly differentiated thyroid cancer. In the present study, we investigated the antitumor activity of IL-12 immunotherapy in BrafV600E knock-in mice. We found that the immune response of CD8+ T and natural killer (NK) cells against tumor cells was significantly suppressed in tumor-bearing mice. IL-12 immunotherapy could inhibit tumor growth and prolong survival by reactivating both CD8+ T and NK cells.
MATERIALS AND METHODS
Animals
LSL-BrafV600E and TPO-Cre strains are generous gifts from Drs Catrin Pritchard (Department of Biochemistry, University of Leicester, Leicester, UK) and Shioko Kimura (Laboratory of Metabolism, National Cancer Institute, Bethesda, MD, USA), respectively. They have been described previously.18, 19 LSL-BrafV600E strain contains a floxed BrafV600E knock-in allele, which becomes an activated oncogene upon Cre-mediated deletion of the floxed transcriptional stop sequence following breeding with TPO- Cre mice,18 which express Cre recombinase under the control of the thyroid peroxidase gene (TPO) promoter. The TPO promoter is active only in thyroid follicular cells at about E14.5.15 To generate LSL-BrafV600E/TPO-Cre mice, LSL-BrafV600E and TPO-Cre strains at the 6–8 weeks of age were bred together and the offspring were characterized by genotyping. The resulting LSL-BrafV600E/TPO-Cre mice express mutant BrafV600E transcripts under the endogenous Braf promoter between 3 and10 days postnatally and spontaneous PTC developed at about 5 weeks of age.15 LSL-BrafV600E/TPO-Cre mice were about half the size of LSL-BrafWT/TPO-Cre mice because of hypothyroidism. LSL-BrafWT/TPO-Cre mice were used as normal controls.
Genotyping of LSL-BrafV600E/TPO-Cre Mice
Genotyping of Cre-mediated recombination of the LSL-BrafV600E-targeted allele has been described previously.19 Briefly, the following primers were used to detect LSL-BrafV600E recombination in the mouse tissue: primer A, 5′-AGTCAATCATCCACAGAGACCT-3′; primer B: 5′-GCTTGGCTGGACGTAAACTC-3′; and primer C, 5′-GCCCAGGCTCTTTATGAGAA-3′. Primers A+C detect the wild-type allele (466 bp) and Cre-recombined BrafV600E allele (Lox-BrafV600E, 518 bp). Primers B+C detect the LSL-BrafV600E allele (140 bp).
Determination of Serum Levels of mIL-12
A single injection of 50 μg of scIL-12/CMVpDNA intramuscularly or a single intraperitoneal injection of 100 ng recombinant mIL-12 was given to five LSL-BrafV600E/TPO-Cre mice, respectively. Serum was collected either every 3 days for 2 weeks following scIL-12/CMVpDNA injection or every 2 for 10 h after recombinant mIL-12 injection. Serum IL-12 levels were analyzed using a mouse IL-12 ELISA Kit (R&D Systems, Minneapolis, MN, USA).
Establishment of a Thyroid Tumor Cell Line
A PTC tumor from a 4-month-old LSL-BrafV600E/TPO-Cre mouse was harvested aseptically using blunt dissection. The tumor was then mechanically dissociated by mincing and passing through a 40-μM mesh sterile screen, and suspended in DMEM/F12 growth medium (10% fetal bovine serum, 100 U/ml penicillin, and 100 μg/ml streptomycin). Cells were further dissociated by incubation in growth medium containing 100 U/ml type I collagenase (Sigma-Aldrich) and 1.0 U/ml dispase I (Roche Diagnostics, Indianapolis, IN, USA) at 37 °C in a rocking water bath for 60 min. The cell suspension was washed two times with growth media and resuspended in a 10-mm culture dish with DMEM/F12 growth medium containing 2 mU/ml bovine TSH (Sigma-Aldrich) to establish a BVE cell line (BrafV600E-induced tumor cell line). The BVE cell line was tested to be tumorigenic after injection of 106 cells subcutaneously into the nude mice. The thyroid origin of the cell line was confirmed by thyroid-specific gene expression of Tshr, Tg, and Slc5a5 and PCR-based genotyping, which shows thyroid-specific 518 bp Lox-BrafV600E fragment (Supplementary Figure 1).
Detection of Thyroid-Specific Gene Expression
The Tshr, Tg, and Slc5a5 gene expression in the thyroid tumor cell line was detected by RT-PCR using the following primers: (1) the Tshr gene (NM_011648, thyrotropin receptor): 5′-TCTGCTGCTCGCCCTGTCCAGG-3′ (forward, in exon 1) and 5′-GGTATGGTCTTCAGATGAGTCT-3′ (reverse, in exon 2). The primer pairs span 92 kb of intron 1 and amplify a 174 bp cDNA fragment); (2) the Tg gene (NM_009375, thyroglobulin): 5′-AGTACCAGGTAGATGCACAGCC-3′ (forward, in exon 2) and 5′-CCAGCTGCCTGCTGCCAGGTA-3′ (reverse, in exon 3). The primer pairs span 945 bp of intron 2 and amplify a 192 bp cDNA fragment; (3) the Slc5a5 gene (NM_053248.2, sodium iodide symporter): 5′-GCATCGCTCCTGTCCACAGGAA-3′ (forward, in exon 4) and 5′-TCCATCAGGTTGATCCGGGAAT-3′ (reverse, in exon 5). The primer pairs span 742 bp of intron 4 and amplify a 203 bp cDNA fragment. The PCR conditions were 95 °C for 5 min, followed by 35 cycles of amplification (95 °C for 40 s, 50–62 °C for 40 s, and 72 °C for 40 s), with final extension at 72 °C for 5 min. The resulting PCR products were analyzed by gel electrophoresis. Each successfully amplified fragment was directly sequenced using the BigDye Terminator V3.1 Cycle Sequencing Kit and ABI Prism 3100 Sequencer (Applied Biosystems, Foster City, CA, USA).
TSH Measurements
Blood was collected by cardiac puncture. Serum TSH was measured using MILLIPLEX MAP Mouse Pituitary Magnetic Bead Panel following the manufacturer’s instruction (EMD Millipore Corporation, Billerica, MA, USA).
IL-12 Gene Therapy Against Established Thyroid Tumors in LSL-BrafV600E/TPO-Cre Mice
Fifty micrograms of plasmid DNA expressing single-chain mouse IL-12 fusion protein (scIL-12/CMVpDNA) in 50 μl PBS were injected into the rectus femoris muscle of hind leg per animal as described previously.13, 20 Ten mice in the treatment group received weekly intramuscular injection of scIL-12/CMVpDNA for 2 months starting from 6 to 8 weeks of age. The same number of mice in the control group received weekly intramuscular injection of vector DNA (CMVpDNA). Mice were observed for survival and killed at the end of 12 months. Tumor load and histology were examined and compared with controls.
Recombinant IL-12 Therapy Against Established Thyroid Tumors in LSL-BrafV600E/TPO-Cre Mice
The half-life of rIL-12 is about 5–10 h and daily injection is required to reach effective serum level. Ten mice received daily intraperitoneal injection of recombinant IL-12 (R&D Systems, Minneapolis, MN, USA) for 5 days (100 ng IL-12 per day in 50 μl PBS), followed by 2-day rest for a total of 40 injections starting from 6 to 8 weeks of age. The same number of mice in the control group received only daily injection of 50 μl PBS. Mice were observed for survival and killed at the end of 12 months. Thyroid tumor load and histology were examined and compared with controls.
Recombinant IL-12 Therapy To Prevent Thyroid Tumorigenesis in LSL-BrafV600E/TPO-Cre Mice
Ten mice received daily intraperitoneal injection of recombinant IL-12 for 5 days, followed by 2-day rest for a total of 40 injections starting from day 7 after birth. Half dosage (50 ng IL-12 in 25 μl PBS per day) was given for the first 3 weeks and normal dosage (100 ng IL-12 in 50 μl PBS per day) for the rest of the treatment. Control mice were injected with PBS only. Mice were observed for survival and killed at the end of 12 months.
Histology and Immunohistochemistry
Histology and immunohistochemical staining was described previously.21 Briefly, 4-μm-thick formalin-fixed, paraffin-embedded tissue sections were prepared and stained with hematoxylin and eosin or anti-CD68 (pan-macrophage marker), anti-CD80 (M1 macrophage marker), and anti-CD206 (M2 macrophage marker) antibodies, respectively (BioLegend, San Diego, CA, USA). Dako LSAB+Kit, HRP was used for immunostaining (Dako, Carpinteria, CA, USA). The sections were counterstained with Mayer’s hematoxylin.
NK Cell Assay and Phenotyping of Effector Cells
A 4-h 51Cr-release assay was used to measure the specific cytotoxicity of spleen cells at different effector/target ratios as described previously.22, 23, 24 The killer cells were immune phenotyped for the presence of surface markers: Thy1, Lyt2, L3/T4, and asialo-GM-1 (aGM1) by using complement-mediated (Cederlane Low-Tox-M Rabbit Complement, 1:20 dilution) cytotoxicity assay in the presence of appropriate antibodies. Briefly, spleen cells (effector cells) were harvested and pooled from six 12-week-old LSL-BrafV600E/TPO-Cre mice (tumor-bearing mice) or three LSL-BrafWT/TPO-Cre mice (normal control) with or without IL-12 treatment (100 ng, intraperitoneal injection for 5 days). BVE cells (target cells at 1 × 106) were labeled with 100 μCi Na51CrO4 (Perkin-Elmer, Waltham, MA, USA) for 2 h at 37 °C. The target cells were then washed two times in a culture medium and resuspended at 5000 cells per well in a 96-well round-bottomed plate. The effector cells were added to the target cells at various effector to target (E:T) ratios in the presence or absence of anti-mouse CD90.2 (Thy1.2, a pan T-cell marker), CD8 (Lyt2), and CD4 (L3/T4) antibodies at 1:20 dilution, and anti-mouse asialo GM1 (anti-NK cell antibody) at 1:200 dilution (Cedarlane, Burlington, ON, Canada). Different concentrations of transforming growth factor-β1 (TGF-β1) antibody (R&D Systems, Abingdon, UK) were also used to investigate its role in tumor target cell killing. After 4 h incubation at 37 °C and 45 min in the presence of complement, 100 μl supernatants were collected and counted with an automatic gamma counter (Canberra-Packard Cobra 5002, Burladingen, Germany). The percentage of specific cytotoxic activity was calculated as follows: ((experimental c.p.m.−spontaneous c.p.m.)/(maximal c.p.m.−spontaneous c.p.m.)) × 100. The spontaneously released c.p.m. was obtained by collecting supernatant of target cells in the complete culture medium. The maximal c.p.m. was released by adding 1% NP40 to the wells in the experiments.
Statistical Analyses
Tumor load and cytotoxicity among different treatment groups were analyzed using the Student’s t-test or repeated measures ANOVA and Bonferroni post-test when appropriate. Kaplan–Meier analysis was used to calculate survival. Differences were considered statistically significant when the P-value was <0.05.
RESULTS
IL-12 Immunotherapy to Treat Established PTC
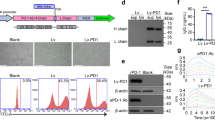
We used two approaches to evaluate IL-12 immunotherapy against PTC: IL-12 gene therapy and IL-12 recombinant protein therapy. IL-12 gene therapy produced persistent low levels of serum IL-12 that peaked at day 6 and last ~2 weeks after single intramuscular injection (Supplementary Figure 2). By contrast, IL-12 recombinant protein therapy resulted in much higher levels of serum IL-12, which were peaked at 2 h and rapidly cleared within 10 h (Supplementary Figure 2). Thus, daily intraperitoneal injection was required to maintain serum IL-12 level. Twenty LSL-BrafV600E/TPO-Cre mice (10 in each group) were given either weekly IL-12 gene therapy or daily 100 ng IL-12 recombinant protein for 2 months. As shown in Figure 1a, the tumor load was reduced by >40% after 2-month IL-12 gene therapy or IL-12 recombinant protein therapy (66.7±6.0 mg in control vs 40±3.3 mg in gene therapy or 37.5±3.1 mg in IL-12 protein therapy group, P<0.01). Histologically, tumors became localized and more differentiated with the reappearance of follicular architecture (Figure 1b). Mononuclear cells and macrophage infiltration were also observed (Figure 1b), indicating that they were activated and mobilized for tumor clearance. Serum TSH levels were not significantly changed during IL-12 treatment. TSH was >50 000 pg/ml (beyond the detection limit of the kit) before and after treatment (n=8) and is >100-fold higher than LSL-BrafWT/TPO-Cre mice (n=5, 394.3±8.7 pg/ml). However, we could not completely rule out some effect of the treatment on the TSH responsiveness of the tumors in the model. The very high serum TSH levels precluded clear determination of a change in TSH levels that might have signaling effects. To evaluate whether IL-12 immunotherapy could affect the survival, 20 LSL-BrafV600E/TPO-Cre mice at the 6–8 weeks of age were treated with either weekly IL-12 gene therapy (n=10) or daily IL-12 recombinant protein therapy (n=10) for 2 months. The mice were monitored for 12 months. As shown in Figure 2a, the survival was significantly increased following IL-12 immunotherapy. Three mice were still alive at the end of the experiment following IL-12 protein therapy (P<0.01) and two mice were alive following IL-12 gene therapy (P<0.05). All the control mice died within 8 months because of tumor load/progression and hypothyroidism.
Thyroid tumor load from LSL-BrafV600E/TPO-Cre mice after interleukin-12 (IL-12) treatment. (a) Tumor weight before and after IL-12 therapy. Mice were killed 1 month after the treatment. Thyroid tumors were removed and their weight was measured. Reduction of tumor size and weight were observed after treatment. (b) Histology of thyroid tumors before and after treatment. As compared with tumors before treatment (A and D), Papillary thyroid carcinoma (PTC) tumors become localized (indicated by block arrows) after either recombinant IL-12 protein therapy (B and E) or IL-12 gene therapy (C and F). Reappearance of follicular architecture is observed with infiltration of many mononuclear cells and macrophages (indicated by arrows) (B).
Effect of interleukin-12 (IL-12) immunotherapy on the survival of LSL-BrafV600E/TPO-Cre mice. (a) Two groups of mice (n=10 in each group) were given either intramuscular injection of 50 μg scIL-12/CMVpDNA or daily intraperitoneal injection of 100 ng recombinant IL-12 protein. Treatment was started at 6–8 weeks of age and continued for 2 months. The survival of the mice was monitored for 12 months. The difference between control and gene therapy (P<0.05) or protein therapy (P<0.01) groups is statistically significant. (b) Effect of early IL-12 immunotherapy on the survival of LSL-BrafV600E/TPO-Cre mice. Ten mice were given daily intraperitoneal injection of IL-12 recombinant protein at 7 days of age and continued for 2 months. The survival of the mice was monitored for 12 months. All the mice in the control group die within 9 months and 4 mice in the treatment group are still alive at the end of 12 months (P<0.01).
Effect of Early IL-12 Immunotherapy on Thyroid Tumorigenesis and Survival
To determine whether early IL-12 immunotherapy could prevent thyroid tumorigenesis or extend survival, we treated 10 LSL-BrafV600E/TPO-Cre mice with IL-12 recombinant protein at the age of 7 days for 2 months. The mice were monitors for 12 months. Although early immunotherapy could not prevent tumor development (all the mice had large tumors at the end of 12 months), it significantly prolonged the survival (Figure 2b). Four mice in the treatment group were still alive at the end of 12 months, whereas all the control mice died within 9 months (P<0.01).
Cytolytic Activity of Immune Cells Induced by IL-12 Immunotherapy
To determine the mechanisms of IL-12-mediated antitumor activities, we measured cytolytic activity of splenocytes from various groups of mice treated with or without IL-12 against BVE tumor cells in a 4-h 51Cr-release assay. As shown in Figure 3a, there was a significant reduction of splenocytes-mediated cytotoxicity against tumor cells in the tumor-bearing mice: 24.3±1.1 (normal LSL-BrafWT/TPO-Cre mice) vs 1.4±0.2 (tumor-bearing LSL-BrafV600E/TPO-Cre mice) at E:T ratio of 10, 38.6±1.3 vs 3.7±1.0 at E:T ratio of 25, and 65±2.1 vs 10.6±0.2 at E:T ratio of 50 (P<0.01), indicating that the splenic effector cell cytotoxicity from the tumor-bearing mice was significantly suppressed. After IL-12 treatment, the effector cell cytotoxicity was substantially improved and was comparable to that from the wild-type mice (Figure 3a). Next, we investigated what kinds of immune effector cells were involved in the cytotoxicity against tumor cells. The cytotoxicity of splenocytes was significantly reduced in the presence of anti-CD8 (P<0.05) or anti-NK cell antibodies (P<0.01). No significant reduction was observed in the presence of anti-CD4 antibodies or anti-CD90.2 antibodies (P>0.05) (Figure 3b). These data indicate that CD8+ T and NK cells are major immune cells involved in the cytolytic activity against tumor cells.
Cytolytic activity of splenocytes against BVE tumors cells. (a) LSL-BrafWT/TPO-Cre mice (TPO-BrafWT, n=3) or LSL-BrafV600E/TPO-Cre mice (TPO-BrafV600E, n=6) were treated with or without 100 ng recombinant interleukin-12 (IL-12) for 5 days. Splenocytes from LSL-BrafWT/TPO-Cre mice (normal control) and LSL-BrafV600E/TPO-Cre mice (tumor-bearing) were used as effector cells in a 4-h 51Cr-release assay against BVE tumor cells (target cells) at various effector to target (E:T) ratios. Cytolytic activity of splenocytes is inhibited in the tumor-bearing mice and recovers after IL-12 treatment. Results are presented as mean±s.e.m. of three separate experiments. (b) Phenotyping of immune cells in the splenocytes-mediated cytolytic activity against tumor cells. Splenocytes were harvested from LSL-BrafV600E/TPO-Cre mice treated with 100 ng IL-12 for 5 days. Their cytolytic activities against BVE tumor cells were evaluated in the presence or absence of anti-CD4 (L3/T4), anti-CD8 (Lyt2), anti-CD90.2 (anti-Thy1.2), or anti-natural killer (NK) cell (anti-mouse asialo GM1) antibodies, respectively, in a 51Cr-release assay. Cytolytic activity of splenocytes is significantly reduced in the presence of anti-CD8 (Lyt2) or anti-NK cell antibodies (P<0.01). Results are presented as mean±s.e.m. of triplicate. Data shown are results from one experiment and representative of three separate experiments.
Effect of TGF-β on the Cytotoxicity of Splenocytes Against Tumor Cells
Epithelial–mesenchymal transition is involved in the PTC progression from well-differentiated tumor to poorly differentiated tumor and TGF-β has been implicated in promoting this process.25 As BVE tumor cells secrete higher level of TGF-β compared with normal thyroid cells (data not shown), TGF-β may be involved in the immune suppression of CD8+ T and NK cells in the tumor-bearing mice. We next investigated whether TGF-β has any role in inhibiting the cytolytic activity of CD8+ T and NK cells. Splenocytes from normal LSL-BrafWT/TPO-Cre mice were cultured in the presence of TGF-β, and the cytolytic activity of splenocytes against BVE tumor cells was measured in a 4-h 51Cr-release assay. As shown in Figure 4a, TGF-β inhibited the cytolytic activity of splenocytes and it was dose-dependent (P<0.01). It also inhibited IL-12-mediated cytolytic activity of splenocytes against BVE tumor cells (Figure 4b). We further investigated whether anti-TGF-β antibody could restore cytolytic activity of splenocytes from tumor-bearing mice. As shown in Figure 4c, the treatment with anti-TGF-β antibody partially restored cytolytic activity of splenocytes.
Inhibitory effect of transforming growth factor-β (TGF-β) on cytolytic activity of splenocytes. (a) Splenocytes from LSL-BrafWT/TPO-Cre (TPO-BrafWT) mice were used as effector cells in a 51Cr-release assay against BVE tumor cells in the presence or absence of different concentrations of TGF-β. Cytotoxicity of splenocytes is significantly reduced by TGF-β and is dose-dependent (P<0.01). (b) LSL-BrafWT/TPO-Cre mice were treated with 100 ng recombinant interleukin-12 (IL-12) for 5 days. Splenocytes from the normal mice were used as effector cells in a 51Cr-release assay against BVE tumor cells in the presence or absence of 5 ng/ml TGF-β1. TGF-β inhibits IL-12-induced cytolytic activity of splenocytes (P<0.01). (c) Splenocytes from LSL-BrafV600E/TPO-Cre (TPO-BrafV600E) mice were used as effector cells in a 51Cr-release assay against BVE tumor cells in the presence or absence of different concentrations of anti-TGF-β antibody. Anti-TGF-β antibody at the 2 μg/ml can partially restore cytolytic activity of splenocytes (P<0.05). Results are presented as mean±s.e.m. of triplicate. Data shown are results from one experiment and representative of three separate experiments.
IL-12 Immunotherapy Increases M1 Tumor-Infiltrating Macrophages
Macrophages are master regulators of inflammation and can differentiate into M1 and M2 macrophages.26 M1 macrophages are activated by lipopolysaccharide or T-helper 1 (Th1) produced interferon-γ. They secrete high levels of IL-12 and low levels of IL-10, and are involved in inflammation and tissue destruction. By contrast, M2 macrophages are activated by Th2 produced anti-inflammatory cytokines IL-4 and IL-10. They produce high levels of IL-10, TGF-β and low levels of IL-12. They are associated with tissue repair, angiogenesis, and tumor promotion. Tumor-associated macrophages are mainly of the M2 phenotype.27 To determine what type of macrophages was activated in the tumor tissue following IL-12 immunotherapy, we performed immunostaining of macrophages using three macrophage markers: CD68, CD80, and CD206. As shown in Figure 5, very little macrophage infiltration is present in the tumor tissue before IL-12 therapy and they are mainly M2 macrophages (CD68+/CD80−/CD206+). The ratio of M1/M2 is about 1/3. However, the M1 macrophages (CD68+/CD80+/CD206−) are significantly increased after IL-12 therapy. The M1/M2 ratio is reversed and is about 3/1.
Interleukin-12 (IL-12) immunotherapy increases M1-infiltrating macrophages. The tumor-infiltrating macrophages were immunostained by anti-CD68 (pan-macrophage marker), anti-CD80 (M1 macrophage marker) and anti-CD206 (M2 macrophage marker) antibodies, respectively. Macrophages are indicated by arrows. The M1 macrophages (CD68+/CD80+/CD206−) are increased after IL-12 therapy.
DISCUSSION
We have demonstrated in the present study that IL-12 immunotherapy is effective against BrafV600E-induced PTC in a genetically engineered mouse model. The therapeutic effects of both IL-12 gene therapy and recombinant protein therapy are comparable and are mediated via CD8+ T and NK cells. Wennerberg et al.28 have recently demonstrated that human anaplastic thyroid carcinoma (ATC) cells are also sensitive to NK cell-mediated lysis and ATC-derived NK cells display a suppressed phenotype with downregulated expression of NKG2D, which is an activating receptor expressed on CD8+ T and NK cells.29 They further demonstrate that the suppression of NK cell-mediated lysis can be restored by blocking prostaglandin-E2, indicating Cox-2 inhibitors may have therapeutic benefit against ATC. However, the selective Cox-2 inhibitor celecoxib failed as a solitary agent (400 mg orally two times a day for 12 months) to treat patients with progressive metastatic differentiated thyroid cancer in an early clinical trial.30 Given that the immune response is suppressed in tumor-bearing hosts (human and mouse), treatment strategies (such as IL-12 immunotherapy or Cox-2 inhibitors) to overcome immune suppression in combination with classic and targeted therapies should offer significant therapeutic benefits against thyroid cancer. The current study confirms in vivo that IL-12 immunotherapy is effective against PTC.
IL-12 is a 70 kDa disulfide-linked heterodimeric cytokine comprising two subunits, p35 (35 kDa) and p40 (40 kDa) subunits and mediates enhancement of the cytotoxic activity of CD8+ T and NK cells.31, 32 It has a pivotal role in modulating the immune response by amplifying cytokine networks involved in the induction of Th1 cells while suppressing Th2 response.33 Indeed, IL-12 possesses the most significant antitumor activity among all cytokines tested. We and others have shown the efficacy of IL-12 gene therapy with a single-chain IL-12 fusion construct created by linkage of the p35 and p40 cDNAs.13, 34 The monomeric nature of single-chain IL-12 fusion protein ensures equal molar expression of each subunit, thereby avoiding the formation of p40 homodimers that antagonize IL-12 activity.35
Although IL-12 has shown significant antitumor activities in many experimental animal models,36 clinical trials with IL-12 used as a single agent in patients with advanced solid tumors and hematologic malignancies have shown mixed response rate ranging from 0 to 11%, except for cutaneous T-cell lymphoma, AIDS-related Kaposi sarcoma, and non-Hodgkin’s lymphoma where higher response rate is demonstrated.37 This is probably because of the lower doses of IL-12 given to the patients because of severe dose-dependent systemic toxicity and higher tumor load (patients in advanced stage). The IL-12 dose used in the current study (daily intraperitoneal injection of 100 ng IL-12, around 4.5–7.7 μg/kg) is well tolerated in mice, which is 10 times higher than the 500 ng/kg tolerated in humans.38 It has been shown that no tumor responses were seen at the 100 ng/kg, but partial or complete response was observed in 71% of Kaposi sarcoma patients receiving higher doses.39 Furthermore, none of the patients in clinical trials received daily injection of IL-12 for >1 month, which may be required for showing therapeutic effects as a single agent given that its serum half-life is about 5–10 h.40 In our current study, we have demonstrated that early systemic IL-12 treatment can significantly prolong survival when tumor load is low as compared with late treatment for established tumors. These data indicate that the application of IL-12 immunotherapy is more appropriate as an adjuvant therapy and should be used in combination with other treatment options such as surgery, radioactive iodine therapy, TSH suppression or targeted therapies against MAKP and/or PIK3/AKT signaling pathways.
Owing to toxicity of systemic administration of IL-12 in cancer patients, gene therapy offers advantage in reducing systemic side effects by local expression of IL-12 gene. The relatively low serum IL-12 levels would reduce systemic toxicity. It has been successfully used in both preclinical41 and clinical trials.42, 43, 44 The commonly used methods include intratumoral injection of IL-12 plasmid DNA,43 peritumoral injection of IL-12-producing autologous fibroblasts42 or autologous tumor cells,45 and intratumoral injection of dendritic cells secreting interleukin-12.44 The response rate ranges from 6 to 89% depending on the tumor types and method of delivery. Intratumoral injection of IL-12 plasmid DNA in patients with advanced malignant melanoma,43 and peritumoral injection of IL-12-producing autologous fibroblasts in patients with disseminated cancer42 have achieved 89% (8/9) and 56% (5/9) response rate, respectively. Currently, there is no clinical trial data available on intramuscular injection of IL-12 plasmid DNA. However, based on our previous and current preclinical studies,13, 20 it should be able to deliver a therapeutic dose by maintaining a lower but more stable serum IL-12 concentrations, which is in contrast to the sharp peaks and troughs in serum levels after bolus systemic injection. The current study could facilitate a clinical trial of IL-12 gene therapy for poorly differentiated thyroid carcinoma, especially in combination with other treatment strategies.
TGF-β has an important role in tumor initiation and progression.46 It can function either as a tumor suppressor or a promoter.47 The mechanisms underlying this dual role of TGF-β remain unclear. There are three TGF-β ligands, TGF-β1, TGF-β2, and TGF-β3. TGF-β1 is the most commonly upregulated ligand in tumor cells.48 It is well known that TGF-β exerts systemic immune suppression and inhibits host immunosurveillance.49 Neutralizing TGF-β enhances CD8+ T- and NK cell-mediated antitumor immune responses.50, 51 Given that TGF-β signaling is upregulated in PTC,25 it likely has a significant role in the suppression of host immune response against thyroid tumor cells. The current study has confirmed the hypothesis. Furthermore, the immune suppression can be reversed and normal immune response be restored by IL-12 immunotherapy. These data support the application of IL-12 immunotherapy as an adjuvant therapy against PTC.
References
Davies L, Welch HG . Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 2006;295:2164–2167.
Hundahl SA, Fleming ID, Fremgen AM et al. A National Cancer Data Base Report on 53,856 Cases of Thyroid Carcinoma Treated in the U.S., 1985–1995 [see comments]. Cancer 1998;83:2638–2648.
Durante C, Haddy N, Baudin E et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–2899.
Mazzaferri EL, Kloos RT . Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 2001;86:1447–1463.
Hollenbeak CS, Boltz MM, Schaefer EW et al. Recurrence of differentiated thyroid cancer in the elderly. Eur J Endocrinol 2013;168:549–556.
Xing M . Braf mutation in thyroid cancer. Endocr Relat Cancer 2005;12:245–262.
Duntas LH, Bernardini R . Sorafenib: rays of hope in thyroid cancer. Thyroid 2010;20:1351–1358.
Cabanillas ME, Waguespack SG, Bronstein Y et al. Treatment with tyrosine kinase inhibitors for patients with differentiated thyroid cancer: The M. D. Anderson Experience. J Clin Endocrinol Metab 2010;95:2588–2595.
Kloos RT, Ringel MD, Knopp MV et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 2009;27:1675–1684.
Gupta-Abramson V, Troxel AB, Nellore A et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008;26:4714–4719.
Schlumberger M, Tahara M, Wirth LJ et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med 2015;372:621–630.
Jin N, Jiang T, Rosen DM et al. Dual inhibition of mitogen-activated protein kinase kinase and mammalian target of rapamycin in differentiated and anaplastic thyroid cancer. J Clin Endocrinol Metab 2009;94:4107–4112.
Shi Y, Parhar RS, Zou M et al. Gene therapy of anaplastic thyroid carcinoma with a single-chain interleukin-12 fusion protein. Hum Gene Ther 2003;14:1741–1751.
Richmond A, Su Y . Mouse xenograft models vs gem models for human cancer therapeutics. Dis Model Mech 2008;1:78–82.
Franco AT, Malaguarnera R, Refetoff S et al. Thyrotrophin receptor signaling dependence of Braf-induced thyroid tumor initiation in mice. Proc Natl Acad Sci USA 2011;108:1615–1620.
Knauf JA, Ma X, Smith EP et al. Targeted expression of Brafv600e in thyroid cells of transgenic mice results in papillary thyroid cancers that undergo dedifferentiation. Cancer Res 2005;65:4238–4245.
Charles RP, Iezza G, Amendola E et al. Mutationally activated Braf(V600e) elicits papillary thyroid cancer in the adult mouse. Cancer Res 2011;71:3863–3871.
Kusakabe T, Kawaguchi A, Kawaguchi R et al. Thyrocyte-specific expression of Cre recombinase in transgenic mice. Genesis 2004;39:212–216.
Mercer K, Giblett S, Green S et al. Expression of endogenous oncogenic V600eb-Raf induces proliferation and developmental defects in mice and transformation of primary fibroblasts. Cancer Res 2005;65:11493–11500.
Shi Y, Parhar RS, Zou M et al. Gene therapy of melanoma pulmonary metastasis by intramuscular injection of plasmid DNA encoding tissue inhibitor of metalloproteinases-1. Cancer Gene Ther 2002;9:126–132.
Zou M, Al-Baradie RS, Al-Hindi H et al. S100a4 (Mts1) gene overexpression is associated with invasion and metastasis of papillary thyroid carcinoma. Br J Cancer 2005;93:1277–1284.
Parhar RS, Shi Y, Zou M et al. Effects of cytokine-mediated modulation of Nm23 expression on the invasion and metastatic behavior of B16f10 melanoma cells. Int J Cancer 1995;60:204–210.
Parhar RS, Lala PK . Amelioration of B16f10 melanoma lung metastasis in mice by a combination therapy with indomethacin and interleukin 2. J Exp Med 1987;165:14–28.
Lala PK, Parhar RS . Cure of B16f10 melanoma lung metastasis in mice by chronic indomethacin therapy combined with repeated rounds of interleukin 2: characteristics of killer cells generated in situ. Cancer Res 1988;48:1072–1079.
Knauf JA, Sartor MA, Medvedovic M et al. Progression of Braf-induced thyroid cancer is associated with epithelial–mesenchymal transition requiring concomitant map kinase and TGFbeta signaling. Oncogene 2011;30:3153–3162.
Mills CD . Anatomy of a discovery: M1 and M2 macrophages. Front Immunol 2015;6:212.
Galdiero MR, Garlanda C, Jaillon S et al. Tumor associated macrophages and neutrophils in tumor progression. J Cell Physiol 2013;228:1404–1412.
Wennerberg E, Pfefferle A, Ekblad L et al. Human anaplastic thyroid carcinoma cells are sensitive to NK cell-mediated lysis via Ulbp2/5/6 and chemoattract NK cells. Clin Cancer Res 2014;20:5733–5744.
Gonzalez S, Lopez-Soto A, Suarez-Alvarez B et al. Nkg2d ligands: key targets of the immune response. Trends Immunol 2008;29:397–403.
Mrozek E, Kloos RT, Ringel MD et al. Phase II study of celecoxib in metastatic differentiated thyroid carcinoma. J Clin Endocrinol Metab 2006;91:2201–2204.
Kobayashi M, Fitz L, Ryan M et al. Identification and purification of natural killer cell stimulatory factor (Nksf), a cytokine with multiple biologic effects on human lymphocytes. J Exp Med 1989;170:827–845.
Stern AS, Podlaski FJ, Hulmes JD et al. Purification to homogeneity and partial characterization of cytotoxic lymphocyte maturation factor from human B-lymphoblastoid cells. Proc Natl Acad Sci USA 1990;87:6808–6812.
Colombo MP, Trinchieri G . Interleukin-12 in anti-tumor immunity and immunotherapy. Cytokine Growth Factor Rev 2002;13:155–168.
Lode HN, Dreier T, Xiang R et al. Gene therapy with a single chain interleukin 12 fusion protein induces T cell-dependent protective immunity in a syngeneic model of murine neuroblastoma. Proc Natl Acad Sci USA 1998;95:2475–2480.
Chen L, Chen D, Block E et al. Eradication of murine bladder carcinoma by intratumor injection of a bicistronic adenoviral vector carrying cDNAs for the IL-12 heterodimer and its inhibition by the IL-12 P40 subunit homodimer. J Immunol 1997;159:351–359.
Lasek W, Zagozdzon R, Jakobisiak M . Interleukin 12: still a promising candidate for tumor immunotherapy? Cancer Immunol Immunother 2014;63:419–435.
Del Vecchio M, Bajetta E, Canova S et al. Interleukin-12: biological properties and clinical application. Clin Cancer Res 2007;13:4677–4685.
Alatrash G, Hutson TE, Molto L et al. Clinical and immunologic effects of subcutaneously administered interleukin-12 and interferon alfa-2B: phase I trial of patients with metastatic renal cell carcinoma or malignant melanoma. J Clin Oncol 2004;22:2891–2900.
Little RF, Pluda JM, Wyvill KM et al. Activity of subcutaneous interleukin-12 in AIDS-related Kaposi sarcoma. Blood 2006;107:4650–4657.
Atkins MB, Robertson MJ, Gordon M et al. Phase I evaluation of intravenous recombinant human interleukin 12 in patients with advanced malignancies. Clin Cancer Res 1997;3:409–417.
Sangro B, Melero I, Qian C et al. Gene therapy of cancer based on interleukin 12. Curr Gene Ther 2005;5:573–581.
Kang WK, Park C, Yoon HL et al. Interleukin 12 gene therapy of cancer by peritumoral injection of transduced autologous fibroblasts: outcome of a phase I study. Hum Gene Ther 2001;12:671–684.
Heinzerling L, Burg G, Dummer R et al. Intratumoral injection of DNA encoding human interleukin 12 into patients with metastatic melanoma: clinical efficacy. Hum Gene Ther 2005;16:35–48.
Mazzolini G, Alfaro C, Sangro B et al. Intratumoral injection of dendritic cells engineered to secrete interleukin-12 by recombinant adenovirus in patients with metastatic gastrointestinal carcinomas. J Clin Oncol 2005;23:999–1010.
Sun Y, Jurgovsky K, Moller P et al. Vaccination with IL-12 gene-modified autologous melanoma cells: preclinical results and a first clinical phase I study. Gene Ther 1998;5:481–490.
Bierie B, Moses HL, Tumour Microenvironment . TGFbeta: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer 2006;6:506–520.
Massague J . TGFbeta in cancer. Cell 2008;134:215–230.
Derynck R, Zhang YE . Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature 2003;425:577–584.
Yang L, Pang Y, Moses HL . TGF-beta and immune cells: an important regulatory axis in the tumor microenvironment and progression. Trends Immunol 2010;31:220–227.
Thomas DA, Massague J . TGF-beta directly targets cytotoxic T cell functions during tumor evasion of immune surveillance. Cancer Cell 2005;8:369–380.
Lee JC, Lee KM, Kim DW et al. Elevated Tgf-beta1 secretion and down-modulation of Nkg2d underlies impaired NK cytotoxicity in cancer patients. J Immunol 2004;172:7335–7340.
Acknowledgements
We thank Drs Shioko Kimura and Catrin Pritchard for the generous gifts of TPO-Cre and LSL-BrafV600E mice, respectively. We also thank Mr Wilfredo Antiquera for excellent technical support. This study is supported by KACST Grant 11-BIO1434-20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
The BRAFV600E mutation is found in more than 40% of papillary thyroid cancer (PTC) cases. In the present study, the authors found that both IL-12 gene therapy and recombinant protein therapy are effective against PTC in a mouse model. Given that the immune response is significantly suppressed in tumor-bearing mice and can be restored by IL-12, these results suggest that IL-12 may be an adjuvant therapy for thyroid cancer.
Rights and permissions
About this article
Cite this article
Parhar, R., Zou, M., Al-Mohanna, F. et al. IL-12 immunotherapy of BrafV600E-induced papillary thyroid cancer in a mouse model. Lab Invest 96, 89–97 (2016). https://doi.org/10.1038/labinvest.2015.126
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2015.126
This article is cited by
-
A novel signature to predict thyroid cancer prognosis and immune landscape using immune-related LncRNA pairs
BMC Medical Genomics (2022)
-
Novel targeted therapies and immunotherapy for advanced thyroid cancers
Molecular Cancer (2018)