Abstract
The bone marrow microenvironment, known as ‘hematopoietic stem cell niche,’ is essential for the survival and maintenance of hematopoietic stem cells. Myelodysplastic syndromes (MDS) are a group of clonal hematopoietic stem cell diseases, which eventually result in leukemic transformation (acute myelogenous leukemia with myelodysplasia-related changes, AML-MRC). However, the precise components and functions of the MDS niche remain unclear. Recently, CXCL12-abundant reticular cells were shown to act as a hematopoietic stem cell niche in the murine bone marrow. Using immunohistochemistry, we show here that CXCL12+ cells were located in the cellular marrow or perivascular area, and were in contact with CD34+ hematopoietic cells in control and MDS/AML-MRC bone marrow. MDS bone marrow exhibited higher CXCL12+ cell density than control or AML, not otherwise specified (AML-NOS) bone marrow. Moreover, AML-MRC bone marrow also exhibited higher CXCL12+ cell density than control bone marrow. CXCL12+ cell density correlated positively with bone marrow blast ratio in MDS cases. CXCL12 mRNA level was also higher in MDS bone marrow than in control or AML-NOS bone marrow. In vitro coculture analysis revealed that overexpression of CXCL12 in stromal cells upregulated BCL-2 expression of leukemia cell lines. Triple immunostaining revealed that the CD34+ hematopoietic cells of MDS bone marrow in contact with CXCL12+ cells were BCL-2-positive and TUNEL-negative. In the bone marrow of MDS cases, CXCL12-high group showed significantly higher Bcl-2+/CD34+ cell ratio and lower apoptotic cell ratio than CXCL12-low group. Moreover, CXCL12-high refractory cytopenia with multilineage dysplasia (RCMD) cases had a greater tendency to progress to refractory anemia with excess blasts (RAEBs) or AML-MRC than CXCL12-low RCMD cases. These results suggest that CXCL12+ cells constitute the niche for CD34+ hematopoietic cells, and may be associated with the survival/antiapoptosis of CD34+ hematopoietic cells and disease progression in MDS. Thus, CXCL12+ cells may represent a novel MDS therapeutic target.
Similar content being viewed by others
Main
The bone marrow microenvironment, known as the hematopoietic stem cell niche, is considered essential for the survival, differentiation, and maintenance of hematopoietic stem cells and hematopoietic progenitor cells with variable regulatory signals.1, 2 Several cell types have been proposed to compose the bone marrow microenvironment, including osteoblasts, endothelial cells, mesenchymal stem cells, adipocytes, macrophages, nonmyelinating Schwann cells,3 and reticular cells.4 Among these cell types, CXCL12-abundant reticular cells have recently been shown to contribute to hematopoietic stem cell maintenance and to act as the hematopoietic niche in a mouse model.4, 5 CXCL12 is a chemokine that, together with its receptor CXCR4, acts as a signal transducer in many kinds of cells. CXCR4 is expressed by various types of cells including hematopoietic stem cells, and CXCL12–CXCR4 signaling is known to be involved in mobilizing and trafficking hematopoietic progenitor cells6 and have a crucial role in maintaining the hematopoietic stem cell pool.7 CXCL12 also enhances the survival/antiapoptosis of hematopoietic progenitor cells in vitro and in vivo.8 Experiments using knockout mice have revealed that depleting CXCL12-abundant reticular cells leads to reduced hematopoietic stem cell numbers.5 Morphologically, CXCL12-abundant reticular cells have long processes and are scattered throughout the murine bone marrow as a network.4, 5 The sinusoid endothelia are surrounded by the CXCL12-abundant reticular cells, and most hematopoietic stem cells are in contact with CXCL12-abundant reticular cells.4, 5
Recent studies have also focused on the importance of the relationship between cancer stem cells and their niche for the regulation and maintenance of the cancer stem cells. Cancer stem cells are a specific cell population capable of initiating and sustaining tumor proliferation.9, 10, 11 These cells, including leukemia stem cells, are known to be chemotherapy-resistant, and their survival may be related to disease recurrence.12 The interaction between niche and leukemia stem cells was identified recently to be associated with chemotherapy resistance in an acute myelogenous leukemia (AML) mouse model.13 Thus, therapies must target the interaction between niche and cancer stem cells to improve the response to therapies.
Myelodysplastic syndromes (MDS) are a heterogeneous group of clonal hematopoietic disorders derived from hematopoietic stem cell abnormalities. An increase in blasts occurs with disease progression, which finally results in leukemic transformation (AML with myelodysplasia-related changes, AML-MRC). AML-MRC is generally considered incurable without allogenic hematopoietic stem cell transplantation, and AML-MRC has an unfavorable prognosis because of a low probability of complete hematologic remission and a high possibility of leukemia relapse after chemotherapy.14
In this study, we investigated the expression of CXCL12 in MDS/AML-MRC bone marrow to analyze the role of the hematopoietic niche in the pathogenesis of MDS. Understanding the interaction of hematopoietic cells with bone marrow niches should help in developing novel niche-targeted MDS therapies.
MATERIALS AND METHODS
Clinical Samples
Formalin-fixed, paraffin-embedded bone marrow samples were collected from 13 control cases, 33 MDS cases (refractory cytopenia with multilineage dysplasia (RCMD)=16; refractory anemia with ringed sideroblasts=2; RAEB=15), 10 AML-MRC cases, and 10 AML-not otherwise specified (NOS) cases (M2=5, M4=3, M5=2) at Tokyo Medical and Dental University. Fresh-frozen bone marrow samples were obtained from 16 control cases, 39 MDS cases (RCMD=26, RAEBs=13), 12 AML-MRC cases, and 10 AML-NOS cases (M0=2, M1=1, M2=3, M4=1, M5=2, M6=1) at National Hospital Organization Kumamoto Medical Center. Control samples were obtained from donors who had abnormalities in laboratory data including blood count, IgG level, sIL-2 R level, or from patients who suffered from malignant lymphoma for disease staging. These control samples all had no morphologic abnormalities in bone marrows. Diagnosis was confirmed according to the WHO criteria, and informed consent was obtained from all donors. This study was approved by the ethics committees of Tokyo Medical and Dental University and the National Hospital Organization Kumamoto Medical Center, and all procedures were used in accord with the ethical standards established by these committees.
Immunohistochemistry
The 4-μm-thick formalin-fixed, paraffin-embedded bone marrow sections were used. After deparaffinization, heat-based antigen retrieval, endogenous peroxidase blockade using 3% hydrogen peroxide, and blocking were performed. The primary antibodies used were as follows: CXCL12, mouse monoclonal, clone no. 79018 1:100 (R&D Systems, Minneapolis, MN, USA); CD34, mouse monoclonal (Nichirei Bioscience, Tokyo, Japan); BCL-2, mouse monoclonal, 1:100 (Dako, Glostrup, Denmark); c-kit, rabbit polyclonal, 1:1000 (Dako); and cleaved caspase-3, rabbit monoclonal, 1:100 (Cell Signaling Technology, Danvers, MA, USA). The primary antibodies were incubated overnight at 4 °C. Detection was performed as follows: ABC Kit (Vector Laboratories, Burlingame, CA, USA) or EnVision+ System-HRP (Dako) with diaminobenzidine (DAB; Nichirei Bioscience); or HISTOFINE simple stain AP series (Nichirei Bioscience) with Vector Blue (Vector Laboratories) or Warp Red Chromogen Kit (Biocare Medical, Concord, CA, USA). A TUNEL assay was also performed using the In Situ Cell Death Detection Kit, POD (Roche Diagnostics, Tokyo, Japan) with DAB. For double or triple immunostaining, heat treatment and blocking were performed between each step. We used human tonsil samples as positive controls and confirmed that there was no crossreaction among the antigen detection steps. For negative isotype control, mouse IgG1 (code X0931; Dako) and rabbit immunoglobulin fraction (solid-phase absorbed, code X0936; Dako) diluted to the same concentration of primary antibodies were used.
Evaluation of Immunostaining Specimens
The CXCL12+ cell density of bone marrow specimens was measured as the area (%) of CXCL12+ cell in the cellular marrow. First, each specimen was scanned to identify the area containing the greatest CXCL12+ cell density. Then, after the three highest areas of density were photoscanned at × 1000, we quantified the area of CXCL12+ cells and cellular bone marrow in the field using ImageJ software (http://imagej.nih.gov/ij/). The CXCL12+ cell density was calculated as the mean percentage of CXCL12+ cell area per cellular bone marrow area. The adjacency of CD34+ hematopoietic cells to CXCL12+ cells was manually quantified on a 5 high power field (HPF; × 400 magnification) observation of multistained specimens in each case under the microscope. We distinguished CD34+ vascular endothelial cells from CD34+ hematopoietic cells by their morphologic characteristics. The ratio of BCL-2+ cells per CD34+ hematopoietic cells was calculated on 5 HPF observation. The apoptotic cell ratio was quantified as the percentage of TUNEL-positive cells based on a count of at least 500 hematopoietic cells.
Preparation of RNA and Real-Time Quantitative PCR for Bone Marrow Samples
RNA was extracted from fresh-frozen bone marrow samples and reverse-transcribed as described before.15 PCR reactions with Fast Start Universal SYBR Green Master (Rox) (Roche Diagnostics) and specific primers for CXCL12 and SCF (Table 1) were monitored using the ABI Prism 7900HT Sequence Detection System (Applied Biosystems, Foster, CA, USA). Values for each gene expression were normalized using the relative quantity of β-actin or GAPDH as an endogenous control.
Cell Lines
A mouse fibroblast cell line (3T3), a human acute myeloid leukemia cell line (HL60), a human acute monocytic leukemia cell line (THP-1), and a human chronic myelogenous leukemia (CML) cell line (K562) was cultured as described before.16
Transfection of CXCL12 into 3T3 Cells
Sequences of human CXCL12α were amplified from the cDNA library of HeLa cells using appropriate PCR primers and inserted into the TA cloning site of pTARGET Mammalian Expression Vector System (Promega, Tokyo, Japan). The human CXCL12α primers used for transfection were: 5′-CGCCATGAACGCCAAGGTCGTGGTCG-3′ and 5′-GGCTGTTGTGCTTACTTGTTTAAAGC-3′. The CXCL12 construct was transfected into 3T3 cells using Hily Max Transfection Reagent (Nippon Gene, Tokyo, Japan) (3T3-CXCL12), and ‘mock transfection’ was used as the empty vector (3T3-control).
Coculture Analysis of Leukemia Cells and 3T3 Cells
The 3T3-control and 3T3-CXCL12 cells were adjusted to a concentration of 1 × 105 cells per ml in 6-well plates. After 24 h incubation, HL60, THP-1, and K562 cells were added (2 × 105 cells per ml) and cocultured with 3T3 cells for 48 h. To inhibit the CXCL12/CXCR4 signaling, we use CXCR4 antagonist, AMD3100 (EMD Chemicals, San Diego, CA, USA). Leukemia cell lines were added to 3T3 cells after the 2 h preincubation in medium with 10 μM AMD3100.
Preparation of RNA and Real-Time Quantitative PCR for 3T3 and Leukemia Cell Lines
RNA was extracted from 3T3 cells and leukemia cell lines cocultured with 3T3 cells and reverse transcribed as described before. The expression of human CXCL12 and mouse Cxcl12 in 3T3 cells and the expression of antiapoptotic genes BCL-2 and BCL-XL and proapoptotic genes BAD and BAX in leukemia cell lines was evaluated by real-time PCR. PCR reactions with Fast Start Universal SYBR Green Master (Rox) (Roche Diagnostics) and specific primers (Table 1) or reactions with FAST qPCR Master Mix Plus (Nippon Gene) and the primers and TaqMan probes for Gapdh, TaqMan® Rodent GAPDH Control Reagents (Applied Biosystems), were monitored using the ABI Prism 7900HT Sequence Detection System (Applied Biosystems). Values for each gene expression were normalized using the relative quantity of GAPDH or Gapdh as an endogenous control.
Immunofluorescence
3T3 cells were fixed in 1% paraformaldehyde in PBS and permeabilized with 0.1% NP-40 in PBS at room temperature. Cells were incubated with anti-CXCL12 antibody (R&D Systems) at a 1:100 dilution for 1 h at room temperature. Cells were then stained with FITC-conjugated anti-mouse antibody (Dako) at a 1:100 dilution for 20 min at room temperature. Slides were washed and mounted with Vectashield mounting medium containing 4′,6-diamidino-2-phenylindole (Vector Laboratories). Images were acquired using a BZ-9000 microscope (Keyence, Osaka, Japan) with a × 400 objective.
Western Blotting
The extracts of leukemia cell lines cocultured with 3T3-control or 3T3-CXCL12 cells were used for western blotting. The primary antibodies were anti-human BCL-2 mouse monoclonal antibody (Dako) and anti-GAPDH rabbit polyclonal antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Protein intensity was detected using the ECL Plus Western Blotting Detection System (GE Healthcare, Danbury, CT, USA).
Statistical Analysis
Mann–Whitney’s U-test and Kruskal–Wallis test were used to analyze the RT-PCR and immunohistochemistry data obtained using the human bone marrow samples. χ2-Test was used to evaluate the association between the immunohistochemistry data and prognosis in RCMD cases. Student’s t-test was used to determine differences in mRNA expression data from in vitro analysis. P<0.05 was considered statistically significant.
RESULTS
CXCL12+ Cells are Reticular Cells Scattered Throughout the Human Bone Marrow
First, we examined the morphology and distribution of CXCL12+ cells in control human bone marrows using immunohistochemistry. CXCL12+ cells were identified as reticular cells with long cytoplasmic processes, and the cells were scattered throughout the control bone marrow (Figure 1a). The distribution pattern of these cells was similar to that of CXCL12-abundant reticular cells in murine bone marrow.5 In control human bone marrow, CXCL12+ cells were located among hematopoietic cells of the cellular marrow (Figure 1a), around adipocytes (Figure 1b), in the perivascular area (Figures 1c and d), or in the endosteal area (data not shown). The endothelial cells of capillaries and sinusoids were negative for CXCL12.
Representative images of CXCL12+ cells in bone marrow samples. Scale bar indicates 25 μm. (a–d) CXCL12+ cells in control bone marrow. Arrowheads indicate CXCL12+ cells (brown). CXCL12+ cells are located among hematopoietic cells (a), around adipocytes (b), and in the perivascular area together with capillaries (c) or sinusoids (d). Asterisk indicates the lumen of the sinusoid. (e–g) CXCL12+ cells in myelodysplastic syndrome (MDS) (e), acute myelogenous leukemia with myelodysplasia-related changes (AML-MRC) (f), and AML, not otherwise specified (AML-NOS) (g) bone marrows. Note that CXCL12+ cells increased in MDS and AML-MRC bone marrow, but were scarce in AML-NOS bone marrow.
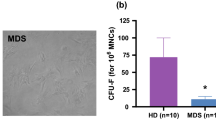
CXCL12+ Cell Density is Increased in MDS/AML-MRC Bone Marrow
To compare the frequency of CXCL12+ cells in MDS/AML-MRC bone marrow with that in control and AML-NOS bone marrows, we analyzed CXCL12+ cell density in these bone marrow samples using immunohistochemistry. Negative control samples were shown in Supplementary Figure 1a. The frequency of CXCL12+ cells in cellular marrow was greater in MDS (Figure 1e) and AML-MRC (Figure 1f) than in control samples (Figures 1a and b). In contrast to these observations, stromal CXCL12+ cells were relatively scarce in AML-NOS bone marrow (Figure 1g). CXCL12+ cell density calculated using an image analyzer in the cellular bone marrow was significantly higher in MDS than in control (P<0.0001) or AML-NOS samples (P<0.0001; Figure 2a). Similarly, AML-MRC bone marrow exhibited significantly higher CXCL12+ cell density than control (P=0.001) or AML-NOS samples (P=0.0002; Figure 2a). In contrast, AML-NOS bone marrow exhibited significantly lower CXCL12+ cell density than control (P=0.03; Figure 2a). Then, we divided MDS cases into CXCL12-high groups (CXCL12+ cell density ≥5%, which is the nearest integer number above the mean±2 s.d. value of the control samples, 4.39) and CXCL12-low groups (CXCL12+ cell density <5%). In MDS bone marrow, CXCL12-high cases showed significantly higher ratio of bone marrow blast than CXCL12-low cases (P=0.0065; Table 2).
CXCL12 expression in bone marrow samples. (a) CXCL12+ cell density (%) in bone marrow samples. *P<0.0001, **P<0.0001, ***P=0.001, ****P=0.0002, and *****P=0.03. (b) A box plot showing CXCL12 expression in bone marrow samples determined by RT-PCR. The quantity of CXCL12 mRNA expression were normalized using the relative quantity of β-actin. *P=0.0363, **P=0.0008, and ***P=0.0234.
Quantitative RT-PCR also showed that MDS bone marrow exhibited significantly higher levels of CXCL12 expression than control (P=0.0363) or AML-NOS bone marrow (P=0.0008; Figure 2b). Furthermore, CXCL12 expression in AML-NOS was significantly lower than in control samples (P=0.0234; Figure 2b). CXCL12-abundant reticular cells in murine bone marrow are known to be major producers of stem cell factor (SCF) in the bone marrow5 and we also investigate the SCF expression in MDS bone marrow. As a result, MDS bone marrow expressed significantly higher levels of SCF than control bone marrow (P=0.0294, data not shown).
CXCL12+ Cells Constitute a Niche-Like Structure for CD34+ Hematopoietic Cells in Control and MDS/AML-MRC Bone Marrows
To evaluate the locational relationships between CXCL12+ cells and vasculature or hematopoietic stem cells, we double immunostained for CXCL12 and CD34. Negative control samples were shown in Supplementary Figure 1b. In control bone marrow, double immunostaining confirmed that CXCL12+ cells localized in the cellular marrow (Figure 3a) and in the perivascular area (Figure 3b), and often in contact with CD34+ hematopoietic cells (Figures 3a and b). In MDS/AML-MRC bone marrow, both CXCL12+ cells and CD34+ hematopoietic cells had increased in number, and the CD34+ hematopoietic cells were intermingled and often in direct contact with CXCL12+ cells (Figure 3c and data not shown for AML-MRC). Clusters of CD34+ hematopoietic cells, known as ‘abnormal localization of immature precursors’ (ALIP), also localized near CXCL12+ cells in MDS bone marrow (Figure 3d). The CXCL12+ cells in MDS bone marrow, as in control bone marrow, were located in the cellular marrow or along with vasculatures identified as CD34+c-kit− elongated luminal structures, and the CXCL12+ cells contacted CD34+c-kit+ hematopoietic cells (Figure 3e). Negative isotype control sample is shown in Supplementary Figure 1c. With regard to the distance between CXCL12+ cells and CD34+ hematopoietic cells, 96.0±7.2% of the CD34+ hematopoietic cells were located within five cell diameters17 from CXCL12+ cells, and 66.6±19.4% of the CD34+ hematopoietic cells were adjoining to (within one cell diameters) CXCL12+ cells in control bone marrow samples (Table 3). In MDS samples, 95.7±2.3% of the CD34+ hematopoietic cells were located within five cell diameters from CXCL12+ cells, and 53.6±10.7% of the CD34+ hematopoietic cells were adjoining to CXCL12+ cells (Table 3). The actual distance between the CD34+ hematopoietic cells and CXCL12+ cells within one cell diameters were 0.27±0.15 μm in control bone marrow and 0.19±0.18 μm in MDS bone marrow. There was no statistically significant difference between control and MDS samples with respect to the distance between CXCL12+ cells and CD34+ hematopoietic cells (Table 3). These results suggest that CXCL12+ cells constitute a niche-like structure for CD34+ hematopoietic cells in MDS/AML-MRC bone marrow, as well as in control bone marrow.
Localization of CXCL12+ cells in control and myelodysplastic syndrome (MDS)/acute myelogenous leukemia with myelodysplasia-related changes (AML-MRC) bone marrow. (a–d) Double immunostaining for CXCL12 (blue) and CD34 (brown) in bone marrow samples. Black arrowheads indicate CXCL12+ cells. White arrowheads indicate CD34+ hematopoietic cells. Black arrows indicate vascular endothelial cells (also CD34+). Among the CD34+ cells, we distinguished between vascular endothelial cells and CD34+ hematopoietic cells as follows. The vascular endothelial cells were elongated and formed luminal spaces, whereas CD34+ hematopoietic cells were spherical and had a large round nucleus and scant cytoplasm (high N/C ratio). Scale bar indicates 25 μm. (a and b) Representative images of control bone marrow showing parenchymal (a) and perivascular (b) localization of CXCL12+ cells and their proximity to CD34+ hematopoietic cells. (c and d) Representative images of myelodysplastic syndrome (MDS bone marrow showing increased numbers of CD34+ hematopoietic cells near CXCL12+ cells. The clusters of CD34+ hematopoietic cells (abnormal localization of immature (ALIP)) also localized near CXCL12+ cells (d). (e) Triple immunostaining for CXCL12 (red), CD34 (brown), and c-kit (blue) in MDS bone marrow. Scale bars indicate 25 μm (left panel) and 10 μm (right panels). Black arrows indicate vascular endothelial cells identified as CD34+c-kit- elongated luminal structure. White arrowheads indicate CD34+ hematopoietic cells identified as CD34+c-kit+ round cells with high N/C ratio. CXCL12+ cells (black arrowheads) were located in the perivascular area and among the hematopoietic nests. They were mostly in contact with CD34+c-kit+ hematopoietic cells.
CXCL12 Upregulates BCL-2 Expression of Human Leukemia Cell Line
To investigate the effects of CXCL12 on the cellular dynamics of hematopoietic cells, we analyzed in vitro cocultures of human leukemia cell lines (HL60, THP-1, and K562) and 3T3-CXCL12 cells. The expression of transfected human CXCL12 in 3T3-CXCL12 cells was confirmed using real-time quantitative PCR (Figure 4a) and immunofluorescent labeling (Figure 4c). The expression level of mouse endogenous Cxcl12 was similar between 3T3-control cells and 3T3-CXCL12 cells (Figure 4b). CXCL12 was shown recently to enhance the survival/antiapoptosis of CD34+ hematopoietic cells,8, 18 and stromal cells producing CXCL12 were shown to prevent apoptosis in leukemia cells by upregulating BCL-2 expression19 through CXCL12/CXCR4 signaling.20 Our results showed that leukemia cells cocultured with 3T3-CXCL12 cells expressed more BCL-2 protein than leukemia cells cocultured with 3T3-control cells (Figure 4d). We used the human-specific anti-BCL-2 antibody to avoid the error to detect mouse Bcl-2 from the contaminated mouse 3T3 cells. The enhancement of BCL-2 expression in leukemia cells under the coculture with 3T3-CXCL12 cells was inhibited by CXCR4 antagonist, AMD3100 (Figure 4d). These results suggested that CXCL12 upregulates the expression of antiapoptotic BCL-2 protein of human leukemia cells though CXCL12/CXCR4 signaling in vitro. We further investigated the expression of BCL-2 and another antiapoptotic gene BCL-XL and proapoptotic genes BAX and BAD. As a result, leukemia cells cocultured with 3T3-CXCL12 cells expressed more antiapoptotic genes BCL-2 and BCL-XL than leukemia cells cocultured with 3T3-control cells, whereas there were no significant difference in BAX and BAD expression (Figure 4e).
In vitro analysis of BCL-2 expression of leukemia cell line cocultured with 3T3-CXCL12 cells. (a) Human CXCL12 mRNA expression in 3T3-control and 3T3-CXCL12 cells. ND, not determined. (b) Mouse CXCL12 mRNA expression in 3T3-control and 3T3-CXCL12 cells. No significant differences between two groups. (c) Immunofluorescence of CXCL12 expression (green) in 3T3-control and 3T3-CXCL12 cells. (d) Western blotting analysis of human BCL-2 expression in leukemia cell line. BCL-2 protein levels were higher in HL60, THP-1, and K562 cells when these cells were cocultured with 3T3-CXCL12 cells than when they were cocultured with 3T3-control cells. CXCR4 inhibitor AMD3100 canceled the effect. Changes in protein levels quantified by Image J were described under each blotting band. (e) The mRNA expression of human antiapoptotic genes, BCL-2 and BCL-XL, and pro-apoptotic genes, BAX and BAD, in leukemia cell line. BCL-2 and BCL-XL levels were significantly higher in HL60, THP-1, and K562 cells when these cells were cocultured with 3T3-CXCL12 cells than when they were cocultured with 3T3-control cells. *P<0.05 and **P<0.01.
CD34+ Hematopoietic Cells in Contact with CXCL12+ Cells Highly Expressed BCL-2 and were Antiapoptotic in MDS Bone Marrow
To examine BCL-2 expression and apoptotic status of MDS CD34+ hematopoietic cells that contact CXCL12+ cells, we performed multistaining in bone marrow samples. We used TUNEL and cleaved caspase-3 as apoptosis markers. CD34+ hematopoietic cells that contacted CXCL12+ cells exhibited upregulated BCL-2 expression in MDS bone marrow (Figure 5a). We also observed that BCL-2+ hematopoietic cells (Figure 5b) and CD34+ hematopoietic cells (Figure 5c) were TUNEL-negative. Moreover, CD34+ hematopoietic cells that contacted CXCL12+ cells were negative for cleaved caspase-3 (Figure 5d), suggesting that these cells were resistant to various apoptosis signals in the MDS bone marrow.
BCL-2 expression of CD34+ hematopoietic cells in contact with CXCL12+ cells in myelodysplastic syndrome (MDS) bone marrow. (a) Triple immunostaining for CD34 (blue), CXCL12 (red), and BCL-2 (brown) in MDS bone marrow. Scale bar indicates 10 μm. CD34+ hematopoietic cells that contacted CXCL12+ cells directly had upregulated expression of BCL-2. White arrowheads indicate CD34+ BCL-2+ hematopoietic cells and black arrowheads indicate CXCL12+ cells. (b) Double staining for terminal deoxynucleotidyl transferase dUTP nick-end labeling (TUNEL) reaction and BCL-2 immunohistochemistry. TUNEL-positive cells are indicated by black arrowheads (brown). BCL-2-positive cells are indicated by white arrowheads (blue). Note that the BCL-2+ hematopoietic cells are TUNEL-negative, suggesting that these cells might avoid apoptosis. Scale bar indicates 25 μm. (c) Double staining for TUNEL reaction and CD34 immunohistochemistry. TUNEL-positive cells are indicated by black arrowheads (brown). CD34-positive cells are indicated by white arrowheads (blue). Scale bar indicates 25 μm. (d) Triple immunostaining for CD34 (brown), CXCL12 (red), and cleaved caspase-3 (blue) in MDS bone marrow. Scale bar indicates 10 μm. CD34+ hematopoietic cells (white arrowheads) that contacted CXCL12+ cells (black arrowheads) were negative for cleaved caspase-3. Note that cleaved caspase 3-positive cell adjoining to CXCL12+ cell is negative for CD34. (e) The percentage of the BCL-2+ cells among the CD34+ hematopoietic cells in MDS bone marrow. CXCL12-low groups: CXCL12+ cell density <5%; CXCL12-high groups: CXCL12+ cell density ≥5%. The bar indicates the median value. *P=0.001. (f) The apoptotic cell ratio (TUNEL-positive cell ratio) of the hematopoietic cells in MDS bone marrow. The bar indicates the median value. **P=0.0025.
CXCL12+ Cell Density was Associated with BCL-2 Expression of MDS CD34+ Hematopoietic Cells and Apoptotic Cell Ratio of MDS Bone Marrow
Next, we examined the association between the CXCL12+ cell density and BCL-2 expression and apoptotic cell ratio of hematopoietic cells in MDS bone marrow. As shown in Figure 5e, CXCL12-high cases exhibited significantly higher BCL-2+/CD34+ cell ratio (the percentage of BCL-2+ cells among CD34+ hematopoietic cells) than CXCL12-low cases in MDS (P=0.001). Moreover, CXCL12-high cases exhibited significantly lower apoptotic cell ratio of hematopoietic cells than CXCL12-low cases in MDS (P=0.0025; Figure 5f). These results suggest that adhesion and interaction with CXCL12+ cells induced resistance to apoptosis in MDS CD34+ hematopoietic cells by upregulating BCL-2 expression.
CXCL12+ Cell Density is Associated with Disease Progression in MDS Patients
To know the relationship between CXCL12+ cell density and disease progression in MDS cases, we investigated the prognosis of the RCMD patients who could be observed for more than 2 years of follow-up period. Among the RCMD patients, four of the five CXCL12-high cases progressed to RAEB or AML-MRC (two cases progressed into RAEB, two cases into AML-MRC), whereas none of the six CXCL12-low cases showed disease progression (P<0.05). These results suggest that higher CXCL12+ cell density may be associated with poor prognosis in RCMD patients.
DISCUSSION
Although CXCL12-abundant reticular cells are known to function as hematopoietic niches in the murine bone marrow,5 CXCL12+ cells in human bone marrow have not been fully characterized. Moreover, little is known about bone marrow niches in hematopoietic malignancies. Thus, identifying the characteristics and functions of CXCL12+ cells in human bone marrow under normal and neoplastic conditions can enhance our understanding of the pathogenesis of myeloid neoplasms.
In this study, we found that CXCL12+ cells created a niche-like structure in control and MDS/AML-MRC bone marrows (Figure 6). Moreover, CXCL12+ cell density in MDS/AML-MRC bone marrow was greater than in control bone marrow. Our result agrees with recent data showing that CD271+/ALP+ mesenchymal stromal cells (MSCs) were immunoreactive for CXCL12 in human bone marrow and that CD271+ MSC area and CXCL12+/ALP+ cell area were both increased in MDS,21 and that CXCL12 cytokine levels were high in MDS bone marrow plasma.22, 23
Schematic illustration of the hematopoietic niche created by CXCL12+ stromal cells and hematopoietic cells in human bone marrow. (a) In control bone marrow, CXCL12+ cells are scattered in the parenchyma and perivascular area, in contact with CD34+ hematopoietic cells, including hematopoietic stem cells. (b) In myelodysplastic syndrome (MDS)/acute myelogenous leukemia with myelodysplasia-related changes (AML-MRC) bone marrow, CXCL12+ cell density and CD34+ hematopoietic cells are both increased. CXCL12+ cells are located in the cellular marrow and perivascular area, and the majority of CD34+ hematopoietic cells are in intimate contact with CXCL12+ cells, as was the case in control bone marrow. The clusters of CD34+ hematopoietic cells (abnormal localization of immature precursors: ALIP) also exhibited close localization with CXCL12+ cells. (c) In contrast, AML, not otherwise specified (AML-NOS) bone marrow exhibited decreased CXCL12+ cell density, whereas immature blasts markedly increased throughout the marrow parenchyma.
With regard to the interaction between CXCL12+ cells and hematopoietic cells, our analyses of in vitro cocultures and MDS samples indicated that contact or interaction with CXCL12+ cells enhances BCL-2 expression and antiapoptosis in CD34+ hematopoietic cells through CXCL12/CXCR4 signaling in MDS bone marrow. Because previous flow cytometric analysis showed that BCL-2 expression in MDS CD34+ hematopoietic cells was upregulated with disease progression,24 an increase in CXCL12+ cells may be associated with the acquisition of apoptosis resistance in MDS bone marrow. This response may be induced by CXCL12/CXCR4 signaling as reported before,20 considering that CD34+ hematopoietic cells in MDS bone marrow express high levels of CXCR4.23 The previous study also showed that coculture with CXCL12-producing stromal cell diminished ara-C-induced apoptosis in leukemic cells by BCL-2 upregulation.19 Therefore, under a similar mechanism, increased expression of CXCL12 might be associated with the chemoresistance of CD34+ hematopoietic cells in MDS/AML-MRC bone marrow.
CXCL12-abundant reticular cells are known to be major producers of SCF in the bone marrow,5 and we found that the MDS bone marrow expresses high levels of SCF. SCF has been shown to increase undifferentiated ‘blast cell’ colonies or clusters in leukemic-type growth of MDS CD34+ cells,25 suggesting that the increase in CXCL12+ cells is associated with blast expansion, partly through SCF/c-kit signaling.
CXCL12/CXCR4 signaling may also modulate other microenvironmental factors such as angiogenesis by recruiting endothelial progenitor cells26, 27, 28 and by secreting angiogenic factors such as angiopoietin-1.29 A previous study showed that the vascularity was higher in MDS than in control bone marrow,30 suggesting that CXCL12+ cells may be associated with angiogenesis in MDS bone marrow.
In contrast to MDS/AML-MRC bone marrow, AML-NOS bone marrow exhibited relatively lower levels of CXCL12 expression and CXCL12+ cell density. A xenograft model of acute lymphoblastic leukemia (ALL) revealed that leukemia cells were able to modulate the niche at the expense of normal hematopoietic stem cells by downregulating CXCL12 levels in areas of leukemia infiltration.31 Another study using a transgenic mouse model of CML in the chronic phase showed that increased G-CSF production by leukemia cells caused a decrease in CXCL12 expression in CML bone marrow, leading to selective impairment of normal hematopoietic stem cell growth and increased growth of CML leukemia stem cells.32 These data suggest that leukemia cell growth in AML-NOS bone marrow, as well as in ALL and CML bone marrows, disrupts the normal hematopoietic stem cell niche and creates new abnormal malignant niches that sequester normal hematopoietic stem cells, whereas CD34+ hematopoietic cells in MDS might use the pre-existing niche for their survival and expansion (Figure 6).
In conclusion, our data suggest that CXCL12+ cells constitute the niche for CD34+ hematopoietic cells of MDS and may be associated with blast expansion, survival/antiapoptosis of CD34+ hematopoietic cells and disease progression. Therefore, niche-targeted therapy against the CXCL12+ cells/hematopoietic cell axis may contribute toward developing a novel strategy for inhibiting disease progression or improving chemosensitivity in MDS patients.
References
Wilson A, Trumpp A . Bone-marrow haematopoietic-stem-cell niches. Nat Rev Immunol 2006;6:93–106.
Morrison SJ, Spradling AC . Stem cells and niches: mechanisms that promote stem cell maintenance throughout life. Cell 2008;132:598–611.
Yamazaki S, Ema H, Karlsson G et al. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 2011;147:1146–1158.
Nagasawa T, Omatsu Y, Sugiyama T . Control of hematopoietic stem cells by the bone marrow stromal niche: the role of reticular cells. Trends Immunol 2011;32:315–320.
Omatsu Y, Sugiyama T, Kohara H et al. The essential functions of adipo-osteogenic progenitors as the hematopoietic stem and progenitor cell niche. Immunity 2010;33:387–399.
Aiuti A, Webb IJ, Bleul C et al. The chemokine SDF-1 is a chemoattractant for human CD34+ hematopoietic progenitor cells and provides a new mechanism to explain the mobilization of CD34+ progenitors to peripheral blood. J Exp Med 1997;185:111–120.
Sugiyama T, Kohara H, Noda M et al. Maintenance of the hematopoietic stem cell pool by CXCL12–CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 2006;25:977–988.
Broxmeyer HE, Cooper S, Kohli L et al. Transgenic expression of stromal cell-derived factor-1/CXC chemokine ligand 12 enhances myeloid progenitor cell survival/antiapoptosis in vitro in response to growth factor withdrawal and enhances myelopoiesis in vivo. J Immunol 2003;170:421–429.
Jordan CT, Guzman ML, Noble M . Cancer stem cells. N Engl J Med 2006;355:1253–1261.
Bonnet D, Dick JE . Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med 1997;3:730–737.
Lapidot T, Sirard C, Vormoor J et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 1994;367:645–648.
Dick JE, Lapidot T . Biology of normal and acute myeloid leukemia stem cells. Int J Hematol 2005;82:389–396.
Saito Y, Uchida N, Tanaka S et al. Induction of cell cycle entry eliminates human leukemia stem cells in a mouse model of AML. Nat Biotechnol 2010;28:275–280.
Szotkowski T, Rohon P, Zapletalova L et al. Secondary acute myeloid leukemia—a single center experience. Neoplasma 2010;57:170–178.
Suzuki S, Kurata M, Abe S et al. Overexpression of MCM2 in myelodysplastic syndromes: association with bone marrow cell apoptosis and peripheral cytopenia. Exp Mol Pathol 2012;92:160–166.
Abe S, Kurata M, Suzuki S et al. Minichromosome maintenance 2 bound with retroviral Gp70 is localized to cytoplasm and enhances DNA-damage-induced apoptosis. PLoS One 2012;7:e40129.
Méndez-Ferrer S, Michurina TV, Ferraro F et al. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 2010;466:829–834.
Lataillade JJ, Clay D, Bourin P et al. Stromal cell-derived factor 1 regulates primitive hematopoiesis by suppressing apoptosis and by promoting G(0)/G(1) transition in CD34(+) cells: evidence for an autocrine/paracrine mechanism. Blood 2002;99:1117–1129.
Konopleva M, Konoplev S, Hu W et al. Stromal cells prevent apoptosis of AML cells by up-regulation of anti-apoptotic proteins. Leukemia 2002;16:1713–1724.
Zeng Z, Shi YX, Samudio IJ et al. Targeting the leukemia microenvironment by CXCR4 inhibition overcomes resistance to kinase inhibitors and chemotherapy in AML. Blood 2009;113:6215–6224.
Flores-Figueroa E, Varma S, Montgomery K et al. Distinctive contact between CD34+ hematopoietic progenitors and CXCL12+ CD271+ mesenchymal stromal cells in benign and myelodysplastic bone marrow. Lab Invest 2012;92:1330–1341.
Matsuda M, Morita Y, Hanamoto H et al. CD34+ progenitors from MDS patients are unresponsive to SDF-1, despite high levels of SDF-1 in bone marrow plasma. Leukemia 2004;18:1038–1040.
Zhang Y, Zhao H, Zhao D et al. SDF-1/CXCR4 axis in myelodysplastic syndromes: correlation with angiogenesis and apoptosis. Leuk Res 2012;36:281–286.
Parker JE, Mufti GJ, Rasool F et al. The role of apoptosis, proliferation, and the Bcl-2-related proteins in the myelodysplastic syndromes and acute myeloid leukemia secondary to MDS. Blood 2000;96:3932–3938.
Sawada K, Koizumi K, Tarumi T et al. Role of physiologic concentrations of stem cell factor in leukemic type growth of myelodysplastic CD34+ cells. Leuk Res 1999;23:1–11.
Jin DK, Shido K, Kopp HG et al. Cytokine-mediated deployment of SDF-1 induces revascularization through recruitment of CXCR4+ hemangiocytes. Nat Med 2006;12:557–567.
Walter DH, Haendeler J, Reinhold J et al. Impaired CXCR4 signaling contributes to the reduced neovascularization capacity of endothelial progenitor cells from patients with coronary artery disease. Circ Res 2005;97:1142–1151.
De Falco E, Porcelli D, Torella AR et al. SDF-1 involvement in endothelial phenotype and ischemia-induced recruitment of bone marrow progenitor cells. Blood 2004;104:3472–3482.
Zhou B, Tsaknakis G, Coldwell KE et al. A novel function for the haemopoietic supportive murine bone marrow MS-5 mesenchymal stromal cell line in promoting human vasculogenesis and angiogenesis. Br J Haematol 2012;157:299–311.
Keith T, Araki Y, Ohyagi M et al. Regulation of angiogenesis in the bone marrow of myelodysplastic syndromes transforming to overt leukaemia. Br J Haematol 2007;137:206–215.
Colmone A, Amorim M, Pontier AL et al. Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science 2008;322:1861–1865.
Zhang B, Ho YW, Huang Q et al. Altered microenvironmental regulation of leukemic and normal stem cells in chronic myelogenous leukemia. Cancer Cell 2012;21:577–592.
Acknowledgements
We thank Ms Miori Inoue and Ms Sachiko Ishibashi for their technical assistance. This work was supported in part by a grant-in-aid (No. 21590432) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
Myelodysplastic syndromes (MDS) are clonal hematopoietic stem cell diseases that eventually result in leukemic transformation. This study shows that CXCL12+ cells constitute a niche in the bone marrow for CD34+ hematopoietic progenitor cells, and may be associated with the survival of CD34+ cells and disease progression in MDS. CXCL12+ cells may therefore represent a novel MDS therapeutic target.
Supplementary information
Rights and permissions
About this article
Cite this article
Abe-Suzuki, S., Kurata, M., Abe, S. et al. CXCL12+ stromal cells as bone marrow niche for CD34+ hematopoietic cells and their association with disease progression in myelodysplastic syndromes. Lab Invest 94, 1212–1223 (2014). https://doi.org/10.1038/labinvest.2014.110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2014.110
This article is cited by
-
The CXCL12gamma chemokine immobilized by heparan sulfate on stromal niche cells controls adhesion and mediates drug resistance in multiple myeloma
Journal of Hematology & Oncology (2021)
-
Prominence of nestin-expressing Schwann cells in bone marrow of patients with myelodysplastic syndromes with severe fibrosis
International Journal of Hematology (2019)
-
The bone-marrow niche in MDS and MGUS: implications for AML and MM
Nature Reviews Clinical Oncology (2018)
-
Role of the microenvironment in myeloid malignancies
Cellular and Molecular Life Sciences (2018)