Abstract
CCAAT-enhancer-binding protein delta (C/EBPδ) is a transcription factor mainly known for its role in inflammation and apoptosis/proliferation. Considering that these are key processes in renal fibrosis, we hypothesized that C/EBPδ would potentiate renal fibrosis. In line with this hypothesis, C/EBPδ has recently been suggested to regulate the fibrotic response during glomerulonephritis. Here we determined the importance of C/EBPδ in the development of renal tubulointerstitial fibrosis by subjecting 8- to 12-week-old C/EBPδ-deficient mice and age- and sex-matched wild-type controls to the unilateral ureteral obstruction model. Mice were killed at 1, 3, or 7 days post surgery, and renal tissues were obtained for RNA, protein, and immunohistochemical analysis. We show that C/EBPδ deficiency resulted in a more profound fibrotic response as evident from enhanced tubular injury, collagen deposition in the interstitial area, and higher expression of transforming growth factor-β. Moreover, we show that the increase in renal fibrosis in C/EBPδ-deficient mice does not depend on an altered proliferation/apoptosis balance or on a differential inflammatory response in the obstructed kidney. In conclusion, our study provides direct evidence that C/EBPδ is a novel mediator of renal fibrosis. Modulating C/EBPδ expression could consequently be a potential antifibrotic strategy in patients with chronic kidney disease.
Similar content being viewed by others
Main
Tissue fibrosis is, in general, a hallmark of chronically failing organs and is a leading cause of morbidity and mortality.1 Renal fibrosis is not an exception and is indeed a major risk factor for the progression to end-stage renal disease and consequently a strong predictor for renal disease outcome.2 Interestingly, in most renal diseases, irrespective of the originating compartment, interstitial fibrosis is the principal common pathway leading to end-stage renal disease (ESRD).3 Although not completely understood, renal fibrosis is probably initiated by a robust inflammatory response, which occurs upon disruption of normal tubular integrity4, 5 and the loss of the renal capillary network.6, 7 Subsequently, the accumulation of interstitial leukocytes and myofibroblasts leads to excessive extracellular matrix (ECM) production eventually leading to tubular atrophy and loss of renal function.8, 9, 10
The different stages of obstructive nephropathy leading to tubulointerstitial fibrosis are frequently studied using the well-established murine unilateral ureteral obstruction (UUO) model.4 In this particular model, tubulointerstitial disease is associated with progressive tubular cell loss and atrophy caused by an imbalance in proliferation and apoptosis.9, 11 Moreover, a strong increase in the accumulation of macrophages in the tubulointerstitial compartment is observed.9, 12 Next to these ‘early’ events, transforming growth factor (TGF)-β expression is induced, which is highly relevant, as TGF-β is an important mediator of fibrosis by mediating (myo)fibroblast proliferation and accumulation, epithelial to mesenchymal transition, and ECM production.13, 14
CCAAT-enhancer-binding protein (C/EBP) δ is a member of the C/EBP family of transcription factors.15 Originally identified as a transcription factor that is rapidly upregulated during the acute phase response, shortly after its discovery, C/EBPδ was already implicated in cell proliferation. Nowadays C/EBPδ is believed to act as a tumor suppressor because of its ability to decrease expression of cell cycle proteins cyclin D1 and cyclin E, while increasing the expression of p27.16, 17, 18 Moreover, C/EBPδ regulates pro-apoptotic gene expression during mammary gland involution19, 20 and inhibits the growth of human cell lines from different tumor types in vitro.16, 21, 22 In line, increased mammary epithelial cell proliferation and ductal hyperplasia is one of the main features observed in C/EBPδ-deficient mice.23 Together, these data suggest that C/EBPδ has an important role in the balance between cell proliferation and apoptosis.
Recently, C/EBPδ expression in macrophages emerges as a key process in pathophysiology. Indeed, we recently showed that macrophage recruitment during Klebsiella-induced pulmonary infection is markedly reduced in C/EBPδ-deficient mice, and the reduced number of macrophages correlated with reduced Klebsiella-induced mortality in C/EBPδ-deficient mice.24 Moreover, C/EBPδ modulates the expression of CCL20, interleukin (IL)-23, CXCL1, and TNFAIP6 in macrophages, and these C/EBPδ targets subsequently potentiate the pathogenesis of rheumatoid arthritis,25 whereas macrophage C/EBPδ also induces phagocytosis of apoptotic neuronal cells.26 Finally, a recent paper shows that C/EBPδ directly drives LPS-induced tumor necrosis factor-α, IL-6, and macrophage inflammatory protein-2 in pulmonary macrophages,27 which may be due to C/EBPδ-dependent toll-like receptor-4 expression.28
Interestingly, C/EBPδ also modifies renal inflammation, as C/EBPδ deficiency protected against Habu snake venom-induced glomerulonephritis. In this particular model, C/EBPδ-deficient mice showed reduced smooth muscle α-actin (αSMA) expression in the glomeruli and diminished deterioration of renal function as compared with wild-type mice.29 Whether C/EBPδ-dependent αSMA expression is causally linked to Habu-venom-induced renal dysfunction, however, remains to be established.
Overall, C/EBPδ might thus be involved in some of the key processes leading to tubulointerstitial fibrosis, and therefore we hypothesized that C/EBPδ would aggravate renal fibrosis. We challenged this hypothesis by evaluating renal fibrosis in wild-type and C/EBPδ-deficient mice subjected to the unilateral ureter obstruction (UUO) model. Surprisingly, we show that C/EBPδ limits UUO-induced renal fibrosis, and this protective effect of C/EBPδ seems independent of the proliferation/apoptosis balance or of the infiltration of macrophages.
MATERIALS AND METHODS
Mice
Specific pathogen-free 8- to 12-week-old female C57BL/6 mice were purchased from Charles River and C/EBPδ-deficient mice (on a C57BL/6 background; generated as described previously30) were bred in the animal facility of the Academic Medical Center with free access to food and water. Mice used for experiments were age and sex matched. The Animal Care and Use Committee of the University of Amsterdam approved all animal experiments.
Experimental Model
Mice were subjected to the well-established model of renal progressive injury (ie, unilateral ureteral obstruction; UUO) as described previously.31 Before surgery, all mice received analgesia (subcutaneous injection of 50 μg/kg buprenorphine (Temgesic; Shering-Plough)). During surgery, the right ureter was ligated with 6-0 silk surgical suture through a small abdominal incision under 2.0% isoflurane-induced anesthesia. Subsequently, the abdomen was closed. Mice were killed 1, 3, or 7 days after surgery, and kidneys were collected for further analysis. Contralateral non-obstructed kidneys served as control as described before.31, 32
Histopathological Scoring
To score renal injury, formalin-fixed paraffin embedded PAS-D-stained slides were analyzed by a pathologist (S.F.) in a blinded manner with respect to the following parameters: tubular dilatation, epithelial simplification, and interstitial expansion. Lesions were graded on a scale from 0 to 4: 0=normal; 1=mild, involvement of less than 25% of the cortex; 2=moderate, involvement of 25 to 50% of the cortex; 3=severe, involvement of 50 to 75% of the cortex; 4=extensive damage involving more than 75% of the cortex. Edema as evident from increased interstitial space was also graded in a blinded manner according to the following: 0=normal; 1=mild, 2=moderate, and 3=severe amount of edema. The final score of each slide was the average of 10 randomly chosen, non-overlapping fields in the cortex of the obstructed kidney at a × 400 magnification.
Immunohistochemistry
C/EBPδ protein expression was determined using a rabbit-anti C/EBPδ antibody (#2318; Cell Signaling Technologies) as described before.33 Collagen staining was performed using a rabbit-anti-collagen type I (GTX41286; GeneTex) antibody as described before.34 Proliferative and apoptotic cells were detected using rabbit anti-Ki67 (#RM-9106; Lab Vision) and anticleaved caspase-3 (#9661S; Cell Signaling Technologies) antibodies essentially as described before.35 In short, after deparaffinization and endogenous peroxidase inhibition, slides were boiled in citrate buffer (pH6.0) for 10 min, blocked with normal goat serum for 30 min, and incubated overnight with the primary antibody (1:1000 for C/EBPδ, 1:500 for Ki67, 1:200 for cleaved caspase-3 and 1:400 for collagen type I) at 4 °C. Subsequently, slides were incubated with Powervision PolyHRP-anti-rabbit IgG (DPVR-55HRP; Immunologic) for 30 min at room temperature and stained using DAB (BS04-999; Immunologic).
Co-localization of tubular segmentation markers with C/EBPδ was assessed using rabbit-anti-SGLT2 (proximal tubules) and rabbit-anti-NCC (distal tubules) antibodies. After performing the C/EBPδ staining as described above, slides were boiled in citrate buffer (pH6.0) for 10 min and incubated overnight with the primary antibody (1:400 for SGLT2 and 1:800 for NCC) at 4 °C. Subsequently, slides were incubated with Powervision PolyAP-anti-rabbit IgG (DPVR-55AP; Immunologic) for 30 min at room temperature and stained using the Vector Blue Alkaline Phosphatase Substrate Kit (SK-5300; Vector Labs).
Detection of Macrophages
Macrophage staining was carried out using a rat-anti-F4/80 antibody (MCA497GA; AbD Serotec) as described before.24 In short, slides were deparaffinized and endogenous peroxidase was inhibited by 0.3% H2O2 in methanol for 10 min. Slides were boiled in citrate buffer (pH6.0) for 20 min, blocked with Ultra V block for 10 min, and incubated overnight with the primary antibody (1:500) at 4 °C. Sections were then incubated with a Rabbit (FAB2)-anti-rat IgG (#6130-01; ITK Diagnostics) 1:3000 in 20% Normal Mouse Serum/PBS for 30 min. Subsequently, slides were incubated with Powervision PolyHRP-anti-rabbit IgG (DPVM-55HRP; Immunologic) for 30 min at room temperature and stained using DAB (BS04-999; Immunologic).
Cytokine Detection
Active TGF-β and hepatocyte growth factor (HGF) levels were measured using ELISA (R&D Systems) according to the manufacturer’s recommendations.
RNA Isolation and RT–PCR
For gene expression analysis, mRNA was isolated from kidney homogenates using Tripure isolation reagent (#11667165001; Roche Diagnostics) according to the manufacturer’s recommendations. All mRNA samples were quantified by spectrophotometry and stored at −80 °C until further analysis. mRNA was DNAase treated (#M6101; Promega, the Netherlands) after which cDNA was prepared. Gene expression analysis was performed using a Roche lightcycler with SYBR green PCR master mix (#04707516001; Roche) using the QuantiTect mouse c/ebpδ primer assay kit (#QT00312809; Qiagen Benelux).
Western Blot
After electrophoresis of the samples on a 12.5% SDS-PAGE gel, proteins were transferred onto Immobilon-P membranes (Millipore). The blots were blocked for 1 h at room temperature in 5% Bovine Serum Albumin (BSA) in TBS+0.1% Tween-20 (TBS-T). Rabbit-anti-C/EBPδ (#2318; Cell Signaling Technologies) and mouse-anti-β-actin (sc-81178; Santa Cruz Biotechnology) were diluted 1:1000 in TBS-T supplemented with 5% (C/EBPδ) or 1% (β-actin) BSA. Membranes were incubated overnight at 4 °C, washed in TBS-T, and incubated with a HRP-linked secondary antibody (1:1000 in TBS-T). After 1 h of incubation at room temperature, blots were washed in TBS-T and imaging was performed using Lumi-Light (12015200001; Roche) and an ImageQuant LAS 4000 biomolecular imager for chemiluminescence (GE Healthcare).
Statistics
Differences between groups were analyzed using a t-test if data in all groups were normally distributed or with a Mann–Whitney U-test when the data were not normally distributed. Analyses were performed using GraphPad Prism version 5.0.
RESULTS
Unilateral Ureteral Obstruction Induces C/EBPδ Expression
In order to determine whether C/EBPδ might have a role during UUO-induced fibrosis, we first assessed C/EBPδ expression during UUO. To this end, C/EBPδ mRNA levels in control and obstructed kidneys of wild-type mice were analyzed. As shown in Figures 1a and c, EBPδ mRNA levels rapidly increase with peak levels 1 day after the induction of UUO. Next, we assessed C/EBPδ protein levels by western blot again showing increased C/EBPδ expression 1 day after UUO induction (Figure 1b). To identify the cell types expressing C/EBPδ, kidney sections of control and obstructed wild-type mice were subjected to immunohistochemical analysis using a specific C/EBPδ antibody. As shown in Figures 1c–f, in control kidney (Figure 1c), some cells, probably monocytes, express C/EBPδ. Upon UUO (Figures 1d–f), tubular epithelial cells and pericytes/smooth muscle cells also stained positive for C/EBPδ. Finally, we performed co-localization AQexperiments for C/EBPδ, NCC (distal tubular marker) and SGLT2 (proximal tubular marker). As shown in Figures 1g, h and c, EBPδ co-localizes with NCC but not with SGLT2, showing C/EBPδ is mainly expressed in distal tubules.
C/EBPδ protein expression is increased during UUO. mRNA (a) and protein (b) levels of C/EBPδ in wild-type kidney before and after induction of UUO. (c–f) Immunohistochemical staining of C/EBPδ protein expression in wild-type kidney before (c) and 1 (d), 3 (e), or 7 (f) days after induction of UUO. ( × 20 magnification; insets × 40 magnification). Arrow (→): tubular epithelial cells; arrowhead (▴): pericytes/smooth muscle cells; open arrowhead (<): monocytes. Double staining of C/EBPδ (brown) with NCC (g; blue) or SGLT2 (h; blue) in wild-type kidney 1 day after induction of UUO (40 × magnification). Data are means±s.e.m. **P<0.01, ***P<0.001.
C/EBP δ Limits UUO-Induced Renal Fibrosis
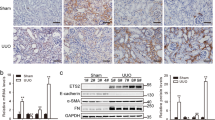
One of the most important mediators in the genesis of renal interstitial fibrosis is TGF-β,13, 36 whereas HGF levels counteract the action of TGF-β.36 Consequently, we next determined whether C/EBPδ modifies TGF-β and/or HGF production by analyzing both proteins in kidney homogenates of wild-type and C/EBPδ-deficient mice subjected to the UUO model. As shown in Figure 2, active TGF-β (Figure 2a) and HGF (Figure 2b) levels increased over time during UUO in wild-type animals. Interestingly, active TGF-β levels were two times higher in C/EBPδ-deficient mice as compared with wild-type mice 7 days after induction of UUO, whereas HGF levels were significantly attenuated in C/EBPδ-deficient mice at day 7.
C/EBPδ attenuates tubulointerstitial fibrogenesis. (a) Active TGF-β and (b) HGF levels in kidney homogenates of wild-type and C/EBPδ-deficient mice during UUO. Data are means±s.e.m. (n=6–8). (c) Quantification of collagen type I protein levels in obstructed kidneys of wild-type and C/EBPδ-deficient mice 7 days after induction of UUO. Data are means±s.e.m. (n=8). (d–g) Immunohistochemical staining of collagen type I protein expression in control (d and f) and 7 days obstructed (f and h) kidneys of wild-type (d and e) or C/EBPδ-deficient (f and g) mice. ( × 20 magnification). *P<0.05, ***P<0.001.
One of the major hallmarks of renal fibrosis is the accumulation of ECM proteins in the interstitium,9, 14, 36 and consequently we analyzed collagen type I deposition in the obstructed kidneys by immunohistochemistry. As shown in Figures 2c–g, collagen type I was highly present in obstructed kidneys 7 days after induction of UUO. Interestingly, collagen type I levels were significantly higher in C/EBPδ-deficient animals compared with wild-type mice (Figures 2c–g). Together, these results suggest that C/EBPδ limits renal fibrosis during obstructive nephropathy.
C/EBP δ Protects Against Tubular Injury
Tubular injury directly drives the formation of interstitial fibrosis.37 Consequently, we assessed the contribution of C/EBPδ to the development of tubular injury. As shown in Figure 3, UUO led to tubular injury in both wild-type and C/EBPδ-deficient animals. Interestingly, UUO-induced tubular damage was increased in C/EBPδ-deficient mice 1 and 3 days post obstruction as compared with wild-type mice. This difference in tubular damage was not observed anymore at day 7 post obstruction, but at this time point end-stage renal disease was reached and tubular injury scores were close to maximum in both genotype groups. C/EBPδ thus limits UUO-induced tubular injury.
C/EBPδ deficiency aggravates tubular injury. (a) Quantification of tubular injury in wild-type and C/EBPδ-deficient obstructed kidneys. Data are means±s.e.m. (n=6–8). **P<0.01. (b, c) PAS-D staining of obstructed kidneys of wild-type and C/EBPδ-deficient mice 3 days after induction of UUO ( × 20 magnification).
The Role of C/EBP δ in the Balance Between Proliferation and Apoptosis
To determine whether the increased tubular injury in C/EBPδ-deficient obstructed kidneys was related to a distortion in the balance between proliferation and apoptosis, we assessed the number of proliferating and apoptotic cells immunohistochemically. As shown in Figures 4a–c, the number of Ki67-positive proliferating cells increased after the induction of UUO with peak levels at day 3. The number of proliferating cells was significantly increased in C/EBPδ-deficient mice as compared with wild-type mice at day 3 after the induction of UUO. However, the difference is rather small (11.5%). As shown in Figures 4d–f, the number of cleaved caspase-3-positive apoptotic cells also increased over time with peak levels at day 7 after the induction of UUO. The increased numbers of apoptotic cells did, however, not significantly differ between the two genotypes. Overall, C/EBPδ seems to slightly affect proliferation without affecting apoptosis during UUO, and the minimal alteration in the proliferation/apoptosis balance does not seem to explain the protective effect of C/EBPδ on fibrosis.
C/EBPδ deficiency slightly influences the balance between proliferation and apoptosis. (a) Quantification of Ki67 expression in wild-type and C/EBPδ-deficient obstructed kidneys. (b, c) Ki67 immunohistochemical staining of obstructed kidneys of wild-type (b) and C/EBPδ-deficient (c) mice 3 days after induction of UUO ( × 20 magnification). (d) Quantification of cleaved-caspase-3 protein expression in wild-type and C/EBPδ-deficient obstructed kidneys. (e, f) Cleaved-caspase-3 immunohistochemical staining of obstructed kidneys of wild-type (e) and C/EBPδ-deficient (f) mice 7 days after induction of UUO ( × 20 magnification). Arrows indicate cleaved-caspase-3-positive cells. Data are means±s.e.m. (n=6–8). **P<0.01.
C/EBP δ does not Affect the Inflammatory Response upon UUO
Next to proliferation/apoptosis, an early event in chronic obstructed nephropathy is a progressive inflammatory response as reflected by the recruitment of macrophages.4 In order to assess whether differential macrophage influx correlated with the observed difference in fibrosis in wild-type and C/EBPδ-deficient mice, we assessed F4/80-positive macrophages in the obstructed kidneys. As shown in Figures 5a–c, macrophage numbers increased drastically between 3 and 7 days after the induction of UUO. However, the number of macrophages did not differ between wild-type and C/EBPδ-deficient obstructed kidneys, suggesting that macrophage infiltration does not contribute to the protective effect of C/EBPδ on fibrosis.
C/EBPδ does not influence macrophage accumulation in obstructed kidneys, but limitis edema formation during UUO. (a) Quantification of F4/80 protein expression in wild-type and C/EBPδ-deficient obstructed kidneys. (b, c) F4/80 immunohistochemical staining of obstructed kidneys of wild-type (b) and C/EBPδ-deficient (c) mice 7 days after induction of UUO ( × 20 magnification). Data are means±s.e.m. (n=6–8). (d) Quantification of edema in wild-type and C/EBPδ-deficient obstructed kidneys. (e and f) Representative pictures of PAS-D-stained wild-type and C/EBPδ-deficient kidney slides 7 days after the induction of UUO. Arrows (→) indicate edema. Data are means±s.e.m.; n=6–8. *P<0.05, **P<0.01.
C/EBP δ Increases Vascular Leakage
Renal microvasculature injury constitutes an important mechanism in renal fibrosis, and disruption of the endothelial integrity may potentiate fibrosis after obstruction of the ureter. Consequently, we assessed the extent of edema in both wild type and C/EBPδ deficient at day 3 and 7 after the induction of UUO. Interestingly, as shown in Figures 5d–f, the amount of edema was significantly increased in obstructed kidneys from C/EBPδ-deficient mice as compared with wild-type mice, showing that C/EBPδ limits vascular leakage during UUO.
DISCUSSION
Independent of the primary cause, tubulointerstitial fibrosis is the final common pathway of many chronic kidney diseases that finally leads to ESRD. It is thus important to get better insight into the mechanisms underlying renal fibrosis in order to design new therapeutic strategies for limiting progressive renal disease. Interestingly, C/EBPδ recently emerged as a transcription factor involved in both proliferation and inflammation. Considering the importance of proliferation and inflammation in tubulointerstitial fibrosis, we hypothesized that C/EBPδ would drive fibrosis and consequently that C/EBPδ deficiency would limit renal fibrosis. Unexpectedly, however, we show that C/EBPδ actually attenuates fibrotic responses in the well-established UUO model of renal fibrosis as evident from increased TGF-β levels and collagen type I synthesis in C/EBPδ-deficient obstructed kidneys compared with wild-type obstructed kidneys.
To elucidate the underlying mechanism by which C/EBPδ would limit UUO-induced fibrosis, we initially focused on the proliferation/apoptosis balance. A distortion in this balance is suggested to contribute to UUO-induced fibrosis, whereas C/EBPδ is particularly well known to regulate the proliferation/apoptosis balance. In the current study, we did not observe major differences in either proliferation or apoptosis in obstructed wild-type vs C/EBPδ-deficient kidneys. This result may be surprising in light of the role of C/EBPδ in proliferation/apoptosis, although one should realize that most of the studies implying C/EBPδ in proliferation/apoptosis have been performed in cancer cells. Indeed, C/EBPδ induces growth arrest and apoptosis in different cancer cell lines,16, 22 whereas C/EBPδ silencing by promoter hypermethylation is positively correlated with tumor progression.38, 39 Importantly, however, C/EBPδ also drives pro-apoptotic gene expression during mammary gland involution,19, 20 and C/EBPδ is thus not only involved in proliferation/apoptosis in a cancer setting. Most likely, C/EBPδ exerts its effect on proliferation/apoptosis in a cell type dependent manner, and C/EBPδ may not be considered a general driver of apoptosis.
Accumulating evidence suggest that C/EBPδ might have an important role in macrophage function, and we recently showed that migration of macrophages upon Klebsiella-induced pneumonia was significantly decreased in C/EBPδ-deficient mice.24 In the current study, we did, however, not observe any difference in macrophage numbers in obstructed kidneys of wild-type and C/EBPδ-deficient mice. Consequently, C/EBPδ does not limit renal fibrosis during obstructive nephropathy by modifying macrophage recruitment. Alternatively, C/EBPδ could modify macrophage function during UUO. However, macrophage-dependent TGF-β production, a key process in UUO-induced fibrosis, is not affected by C/EBPδ in vitro. Indeed, TGF-β production is similar in wild-type and C/EBPδ-deficient bone marrow-derived macrophages and/or tubular epithelial cells (unpublished data). Overall, C/EBPδ-driven processes in macrophages do not seem to explain the observed difference in UUO-induced fibrosis.
As already touched upon, another hallmark of the development of renal fibrosis is microvasculature injury,40 and disruption of the endothelial integrity may potentiate fibrosis after obstruction of the ureter.6, 7 Interestingly, C/EBPδ limits UUO-induced vascular leakage as evident from a significant increase in edema in obstructed kidneys from C/EBPδ-deficient mice as compared with wild-type mice. It is tempting to speculate that C/EBPδ-dependent prevention of vascular barrier disruption indeed limits subsequent interstitial fibrosis, but ongoing studies are needed to prove or refute this hypothesis.
It is well established that αSMA levels are increased during UUO. Indeed, we also observed increased levels of αSMA both on the mRNA and protein level, but the increase was similar in wild-type and C/EBPδ-deficient obstructed kidneys (Supplementary Figure 1). This is in contrast to recent data that αSMA is regulated by C/EBPδ in Habu-venom-induced glomerulonephritis.29 More importantly, the authors also state, but do not show, that αSMA mRNA levels are reduced in C/EBPδ-deficient mice during UUO. At this moment, we do not have a proper explanation for these seemingly contradictory results, although it is difficult to compare our data with these unpublished observations, as no experimental details are available.
Overall, we show that C/EBPδ limits UUO-induced renal fibrosis by a mechanism not related to the proliferation/apoptosis balance or infiltration of macrophages. Irrespective of the actual mechanism, however, we pinpoint C/EBPδ as a key factor in the prevention of renal interstitial fibrosis.
References
Wynn TA . Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. J Clin Invest 2007;117:524–529.
Becker GJ, Hewitson TD . The role of tubulointerstitial injury in chronic renal failure. Curr Opin Nephrol Hypertens 2000;9:133–138.
Liu Y . Cellular and molecular mechanisms of renal fibrosis. Nat Rev Nephrol 2011;7:684–696.
Bascands JL, Schanstra JP . Obstructive nephropathy: Insights from genetically engineered animals. Kidney Int 2005;68:925–937.
Eddy AA . Molecular basis of renal fibrosis. Pediatr Nephrol 2000;15:290–301.
Ohashi R, Shimizu A, Masuda Y et al. Peritubular capillary regression during the progression of experimental obstructive nephropathy. J Am Soc Nephrol 2002;13:1795–1805.
Rouschop KM, Claessen N, Pals ST et al. CD44 disruption prevents degeneration of the capillary network in obstructive nephropathy via reduction of TGF-beta 1-induced apoptosis. J Am Soc Nephrol 2006;17:746–753.
Iwano M, Neilson EG . Mechanisms of tubulointerstitial fibrosis. Curr Opin Nephrol Hypertens 2004;13:279–284.
Klahr S, Morrissey J . Obstructive nephropathy and renal fibrosis. Am J Physiol Renal Physiol 2002;283:F861–F875.
Strutz F, Neilson EG . New insights into mechanisms of fibrosis in immune renal injury. Springer Semin Immunopathol 2003;24:459–476.
Gobe GC, Axelsen RA . Genesis of renal tubular atrophy in experimental hydronephrosis in the rat—role of apoptosis. Lab Invest 1987;56:273–281.
Klahr S . Obstructive nephropathy. Kidney Int 1998;54:286–300.
Lopez-Hernandez FJ, Lopez-Novoa JM . Role of TGF-beta in chronic kidney disease: an integration of tubular, glomerular and vascular effects. Cell Tissue Res 2012;347:141–154.
Zeisberg M, Neilson EG . Mechanisms of tubulointerstitial fibrosis. J Am Soc Nephrol 2010;21:1819–1834.
Lekstrom-Himes J, Xanthopoulos KG . Biological role of the CCAAT/enhancer-binding protein family of transcription factors. J Biol Chem 1998;273:28545–28548.
Gery S, Tanosaki S, Hofmann WK et al. C/EBPdelta expression in a BCR-ABL-positive cell line induces growth arrest and myeloid differentiation. Oncogene 2005;24:1589–1597.
Ikezoe T, Gery S, Yin D et al. CCAAT/enhancer-binding protein delta: a molecular target of 1,25-dihydroxyvitamin D3 in androgen-responsive prostate cancer LNCaP cells. Cancer Res 2005;65:4762–4768.
Pawar SA, Sarkar TR, Balamurugan K et al. C/EBP beta targets cyclin D1 for proteasome-mediated degradation via induction of CDC27/APC3 expression. Proc Natl Acad Sci USA 2010;107:9210–9215.
Stein T, Salomonis N, Nuyten DS et al. A mouse mammary gland involution mrna signature identifies biological pathways potentially associated with breast cancer metastasis. J Mammary Gland Biol Neoplasia 2009;14:99–116.
Thangaraju M, Rudelius M, Bierie B et al. C/EBPdelta is a crucial regulator of pro-apoptotic gene expression during mammary gland involution. Development 2005;132:4675–4685.
O'Rourke J, Yuan R, DeWille J . CCAAT/enhancer-binding protein-delta C/EBP-delta is induced in growth-arrested mouse mammary epithelial cells. J Biol Chem 1997;272:6291–6296.
Sivko GS, DeWille JW . CCAAT/enhancer binding protein delta C/EBP delta regulation and expression in human mammary epithelial cells: I. ‘Loss of function’ alterations in the C/EBP delta growth inhibitory pathway in breast cancer cell lines. J Cell Biochem 2004;93:830–843.
Gigliotti AP, Johnson PF, Sterneck E et al. Nulliparous CCAAT/enhancer binding protein delta C/EBP delta knockout mice exhibit mammary gland ductal hyperlasia. Exp Biol Med Maywood 2003;228:278–285.
Duitman J, Hoogendijk AJ, Groot AP et al. CCAAT-enhancer binding protein delta C/EBPdelta protects against Klebsiella pneumoniae-induced pulmonary infection: potential role for macrophage migration. J Infect Dis 2012;206:1826–1835.
Chang LH, Huang HS, Wu PT et al. Role of macrophage CCAAT/enhancer binding protein delta in the pathogenesis of rheumatoid arthritis in collagen-induced arthritic mice. Plos ONE 2012;7:e45378.
Ko CY, Chang LH, Lee YC et al. CCAAT/enhancer binding protein delta CEBPD elevating PTX3 expression inhibits macrophage-mediated phagocytosis of dying neuron cells. Neurobiol Aging 2012;33:e11–e25.
Yan C, Johnson PF, Tang H et al. CCAAT/enhancer-binding protein delta is a critical mediator of lipopolysaccharide-induced acute lung injury. Am J Pathol 2012;182:420–430.
Balamurugan K, Sharan S, Klarmann KD et al. FBXW7alpha attenuates inflammatory signalling by downregulating C/EBPdelta and its target gene Tlr4. Nat Commun 2013;4:1662.
Takeji M, Kawada N, Moriyama T et al. CCAAT/Enhancer-binding protein delta contributes to myofibroblast transdifferentiation and renal disease progression. J Am Soc Nephrol 2004;15:2383–2390.
Sterneck E, Paylor R, Jackson-Lewis V et al. Selectively enhanced contextual fear conditioning in mice lacking the transcriptional regulator CCAAT/enhancer binding protein delta. Proc Natl Acad Sci USA 1998;95:10908–10913.
Rouschop KMA, Sewnath ME, Claessen N et al. CD44 deficiency increases tubular damage but reduces renal fibrosis in obstructive nephropathy. J Am Soc Nephrol 2004;15:674–686.
Vilaysane A, Chun J, Seamone ME et al. The NLRP3 inflammasome promotes renal inflammation and contributes to CKD. J Am Soc Nephrol 2010;21:1732–1744.
Duitman J, Schouten M, Groot AP et al. CCAAT/enhancer-binding protein delta facilitates bacterial dissemination during pneumococcal pneumonia in a platelet-activating factor receptor-dependent manner. Proc Natl Acad Sci USA 2012;109:9113–9118.
Pulskens WP, Rampanelli E, Teske GJ et al. TLR4 promotes fibrosis but attenuates tubular damage in progressive renal injury. J Am Soc Nephrol 2010;21:1299–1308.
Bijlsma MF, Leenders PJ, Janssen BJ et al. Endogenous hedgehog expression contributes to myocardial ischemia-reperfusion-induced injury. Exp Biol Med Maywood 2008;233:989–996.
Farris AB, Colvin RB . Renal interstitial fibrosis: mechanisms and evaluation. Curr Opin Nephrol Hypertens 2012;21:289–300.
Grgic I, Campanholle G, Bijol V et al. Targeted proximal tubule injury triggers interstitial fibrosis and glomerulosclerosis. Kidney Int 2012;82:172–183.
Agrawal S, Hofmann WK, Tidow N et al. The C/EBP delta tumor suppressor is silenced by hypermethylation in acute myeloid leukemia. Blood 2007;109:3895–3905.
Tang D, Sivko GS, DeWille JW . Promoter methylation reduces C/EBP delta CEBPD gene expression in the SUM-52PE human breast cancer cell line and in primary breast tumors. Breast Cancer Res Treat 2006;95:161–170.
Kim W, Moon SO, Lee SY et al. COMP-angiopoietin-1 ameliorates renal fibrosis in a unilateral ureteral obstruction model. J Am Soc Nephrol 2006;17:2474–2483.
Acknowledgements
This study was supported by grant C06.2198 from the Dutch Kidney foundation to JD. We thank Dr Esta Sterneck for providing the C/EBPδ-deficient mice, and Joost Daalhuisen and Marieke ten Brink for technical assistance with the mouse experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
CCAAT-enhancer-binding protein delta (C/EBPδ) deficiency results in a more profound fibrotic response upon unilateral ureteral obstruction that does not depend on an altered proliferation/apoptosis balance or on a differential inflammatory response in the obstructed kidney. Modulating C/EBPδ expression could consequently be a potential anti-fibrotic strategy in patients with chronic kidney disease.
Supplementary information
Rights and permissions
About this article
Cite this article
Duitman, J., Borensztajn, K., Pulskens, W. et al. CCAAT-enhancer binding protein delta (C/EBPδ) attenuates tubular injury and tubulointerstitial fibrogenesis during chronic obstructive nephropathy. Lab Invest 94, 89–97 (2014). https://doi.org/10.1038/labinvest.2013.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2013.127
Keywords
This article is cited by
-
An anti-inflammatory role for C/EBPδ in human brain pericytes
Scientific Reports (2015)