Abstract
Objective:
To identify factors leading to readmission for tracheostomized, ventilator-dependent infants <2 years of age.
Study Design:
Retrospective cohort study of 117 tracheostomized, ventilator-dependent infants followed through 2 years of age.
Results:
Home ventilator use (at hospital discharge, 6 and 12 months of age), inhaled steroid use (at 12 and 24 months of age), oxygen dependence (at 6 and 12 months of age) and tracheostomy (at discharge, 6 and 12 months of age) were increased risks for rehospitalization. Equipment malfunction throughout the first 2 years also contributed to readmissions. Viral infection, with rhinovirus/enterovirus the most commonly identified pathogen, was the most common etiology for rehospitalization. Diuretic use and initial comorbid diagnoses were not associated with increased risk of rehospitalization.
Conclusion:
The risk for rehospitalization for infants requiring tracheostomy and ventilator support was affected by prolonged oxygen use, prolonged ventilator dependence, inhaled steroid use and equipment malfunction, and was equally distributed throughout the first 2 years of life.
Similar content being viewed by others
Introduction
Tracheostomy is being done for a wide variety of reasons in infants before their first discharge from the hospital after birth.1 Some infants are discharged with tracheostomy alone, but most are also dependent on ventilator support secondary to their underlying medical condition.2, 3, 4 In the past, infants had a tracheostomy placed primarily for upper airway abnormalities causing obstruction. However, as medical technology has improved over the past decade, survival of extremely premature infants has significantly increased and a larger portion of recent tracheostomy placements has been in this population because of severe bronchopulmonary dysplasia (BPD) and chronic lung disease (CLD) that require prolonged ventilatory support.5
In 2009, there were 21 541 children with preexisting tracheostomy rehospitalized in the United States, leading to health-care costs of ~$1.4 billion in 1 year.6 Taking care of these infants can be exhaustive at home, involving serious efforts from parents, home health nurses, physicians, social service providers and many others.7 After tracheostomy placement and discharge from the neonatal intensive care unit (NICU), management of these infants is variable, and there are no current national guidelines that address the care of this rapidly increasing, at-risk population.6 Children’s hospitals are quickly moving toward developing and strengthening dedicated teams to care for these patients through the first years of life to promote better outcomes, improve prognosis and decrease future inpatient health-care utilization that further increases the infant’s risk of nosocomial infections and affects the family’s social structure and finances.7
Our objective was to identify the factors that lead to rehospitalization of tracheostomized, ventilator-dependent infants in the NICU through their first 2 years of life. This will help future management teams better identify at-risk infants over time, decrease the mortality and morbidity in this population and minimize the health-care burden. Ultimately, assessing risk in this population will help physicians and their teams design protocols at the time of NICU discharge for long-term management, anticipate home nursing needs and help guide parental discharge education modules to improve the patient’s short-term and long-term outcomes.
Methods
At Children’s Mercy Hospital, once discharge criteria are met, parents and home caregivers are extensively trained and educated on the care of infants requiring chronic home invasive ventilation. The training and education was fairly close to American Thoracic Society clinical practice guidelines.8 At least two caregivers are specifically trained on pulmonary care and assessment, tracheostomy care, emergency response, ventilator training, infection control practices, oxygen and medication administration, tracheal suctioning, pulmonary toilette and use of monitoring devices. A local durable medical equipment company provides for all the equipment and supplies at home. In addition, parents/family caregivers are required to stay with their child for at least 48 h in the parent care unit, where they care for their child independently within the physical confines of the intensive care unit. After hospital discharge, 24/7 private duty nursing and physician access via phone are provided. Regular follow-up visits are scheduled in the multidisciplinary infant home ventilator clinic.
Our data were obtained from the Center for Infant and Pulmonary Disorders (CIPD), located at Children’s Mercy Kansas City (CMH) in Kansas City, MO, USA. The CIPD houses the Infant Pulmonary Disorders Data Repository that provided de-identified data for this study with CMH institutional review board approval. Inclusion criteria for this study included any infant who received tracheostomy and ventilator support before the first discharge from the NICU regardless of underlying diagnosis. Infants who were readmitted at a later date for tracheostomy with or without ventilator dependence were excluded from this study. There were 117 infants born between 1 January 2008 and 30 September 2015 who met these criteria. Of these infants, 80% were >2 years old and 20% were 18 months to 2 years old by 30 September 2015. Diagnoses were obtained by the ICD-9 and ICD-10 (The International Classification of Diseases, Ninth and Tenth Revision) codes in the electronic health records. Abstracted data were entered into the CIPD database by two abstractors to minimize transcribing error.
A retrospective cohort study was designed to assess the factors that led to readmission to the pediatric inpatient ward, pediatric intensive care unit or NICU in this population through the first 2 years of life. The primary categorical outcome variable was rehospitalization. Categorical variables evaluated as potential risk factors for rehospitalization were: (1) the admission reason for rehospitalization (cardiac, gastrointestinal/feeding, pulmonary infectious, other pulmonary complications, equipment malfunction and other reasons (social, and so on)); (2) the underlying comorbid diagnosis of the patients (dysphagia, pulmonary hypertension, adrenal insufficiency, cardiac abnormalities, CLD, structural airway anomalies, reflux/dysphagia/feeding issues, neurological and other disorders (genetic, syndromic, craniofacial diagnosis)); and (3) clinical factors including oxygen dependence, ventilator dependence, inhaled steroid use and diuretic use at the time of NICU discharge, 6 months, 1 year and 2 years of age. Continuous variables included number of rehospitalizations between 0 and 12 months of age, number of rehospitalizations between 13 and 24 months of age, patient age at the time of tracheostomy placement and number of equipment malfunctions.
Data analysis
Statistical analysis used the SAS programming version 9.2 software package (SAS Institute, Cary, NC, USA) and SPSS 20 (IBM Corporation, Armonk, NY, USA). We first performed univariate analysis between the different identified risk factors (listed above) and rehospitalization by using either the χ2 or Fisher’s exact test. For equipment malfunction, which had a category of zero (equipment malfunction/no hospitalization), the exact test was used for analysis. The variables of interest were determined through medical record reviews of the NICU discharge summary, ‘6 months, 12 months and 24 months NICU home tracheostomy/ventilator clinic notes’ and subsequent emergency room and hospital discharge notes. A stepwise logistic regression was then performed using the following variables: age at tracheostomy placement; equipment malfunction; ventilator dependence at NICU discharge, 6 months and 1 year of age; diuretic use at 6 months and 1 year of age; inhaled steroid use at 6 months and 1 year of age; dysphagia; and pulmonary hypertension. The odds ratios (ORs) and 95% confidence intervals (CIs) were reported for each variable. Statistical significance was claimed with P<0.05 for the logistic regression model. The univariate analysis had both the P-values and the Bonferonni corrected P-values reported (that helped minimize confounding).
Results
Demographics
A total of 117 infants were identified as having tracheostomy and ventilator dependence in the NICU. Of these infants, 100 met the inclusion criteria for the study. Seventeen infants were excluded for reasons that included death before NICU discharge (6 patients), tracheostomy upon readmission to the NICU (2 patients) and prolonged hospitalization in the NICU without discharge at the end of the retrospective timeframe for the study (9 patients) (Figure 1). Four infants died before 2 years of age after their first discharge from nursery. Three infants were decannulated before 2 years of age after discharge from nursery. The cohort consisted of 51 male infants (51%) and 49 female infants (49%). Forty-three infants (43%) were born between 23 and 28 weeks of gestational age (GA), 15 infants (15%) were born between 28 and 34 weeks of GA, 15 infants (15%) were born between 35 and 38 weeks of GA and 27 infants (27%) were born between 38 and 42 weeks of GA. These infants received tracheostomy with varying degrees of ventilatory support for a wide variety of reasons, including BPD due to extreme prematurity, cardiac disease, upper airway structural abnormalities/obstruction, CLD, gastrointestinal or feeding problems, neurological problems and underlying genetic disease or syndrome. BPD (28%) and CLD without BPD (23%) were the major underlying diagnoses in our patient population (Figure 2).
Causes of rehospitalization
We assessed the common causes of rehospitalization based on the admission and discharge diagnosis. The most common cause of hospital readmissions was infectious etiology, specifically pulmonary infections (24%), followed by other pulmonary causes (respiratory failure/hypoxia with no infection) (22%), other causes (including social issues, apneic spells, cyanosis, BRUE (Briefly Resolved Unexplained Events, formerly ALTE), dehydration, failure to thrive and so on) (21%), gastrointestinal/feeding issues (14%), equipment malfunction (tracheostomy or gastrostomy-related malfunctions) (8%), admissions for surgery/procedure (8%) and cardiac issues (0.6%) (Figure 3).
Further analyses of pulmonary infections showed that viral infections were the major cause of readmissions (26%). On several occasions, viral infections with 2 or more viruses were present. Of all viral infections, rhinovirus/enterovirus (37%) was the most common virus isolated in this population, followed by respiratory syncytial virus (9%) (Figure 4). All patients in our cohort (100%) received Synagis (palivizumab, Medimmune, Gaithersburg, MD, USA) per national guidelines during the respiratory syncytial virus season to help decrease the risk of its infection.
Our findings showed that our patients’ medical needs increased over time (in terms of oxygen requirement and diuretic and inhaled corticosteroid use), plateaued at 12 months of age and then showed gradual, steady improvement (Figure 5). At 12 months of age, 42% had ventilator dependence, 25% were on a diuretic, 29% were on supplemental oxygen and 34% were on inhaled steroids (Figure 5).
Risk factors for rehospitalization
Univariate analysis was performed using either χ2 analysis or Fisher’s exact test to determine risk factors for rehospitalization (Table 1). Ventilator dependence at NICU discharge (OR=2.37, 95% CI 1.04 to 5.40, P=0.037), 6 months of age (OR=4.36, 95% CI 1.59 to 11.94, P=0.0027) and 12 months of age (OR=3.24, 95% CI 1.38 to 7.58, P=0.0058) was significantly associated with hospital readmission. Inhaled steroid use at 12 months of age (OR=2.87, 95% CI 1.13 to 7.28, P=0.022) and 24 months of age (OR=4.63, 95% CI 1.25 to 17.08, P=0.0139) was also significantly associated with increased rehospitalization rate. Oxygen dependence at 6 months of age (OR=3.38, 95% CI 1.04 to 10.9, P=0.034) and 12 months of age (OR=3.32, 95% CI 1.20 to 9.16) increased the rate of rehospitalization. Having a tracheostomy increased the rate of rehospitalization at 6 months of age (OR=9.37, 95% CI 3.52 to 24.89, P=0.0001), 12 months of age (OR=8.166, 95% CI 3.26 to 20.44, P=0.0001) and 24 months of age (OR=3.02, 95% CI 1.23 to 7.41), P=0.014). Equipment malfunction also increased the risk of readmission (OR=8.50, 95% CI 2.63 to ∞, P=0.002). We further looked at the specific equipment malfunctions from 2008 to 2014 that led to readmission and the most common reasons were tracheal plugging and tracheal dislodgement followed by ventilator/tubing malfunction, tracheostomy obstruction due to granuloma, G-tube dislodgement and cardiac pacemaker failure (Table 3 and Figure 6).
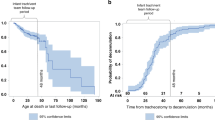
The analysis of variance trend test showed that the younger the patient at the time of tracheostomy, the greater the rate of readmission before 1 year of age (P=0.0390; Figure 7). A backward logistic regression model was then created for the outcome variable of rehospitalization (Table 2). Variables included in the model were age at tracheostomy procedure; ventilator dependence at NICU discharge, 6 months and 1 year of age; diuretic and inhaled steroid use at 6 months and 1 year of age; pulmonary hypertension; and dysphagia. This model showed that ventilator dependence at 6 months and 1 year increased the risk for rehospitalization (OR=29.199, 95% CI 1.985 to 429.442, P=0.0139; and OR=20.749, 95% CI 1.276 to 337.41, P=0.0331, respectively). We also examined the timing of readmissions in first 2 years of life (Figure 8). We found that 40% of readmissions were before 1 year of age, 40% were from 1 to 1.5 years of age and 20% were between 1.5 and 2 years of age.
Discussion
With advanced medical technology in health care, survival of extremely low birth infants with CLD has been increasing. Currently, no national guidelines and standardized care models are available for this population. These infants are frequently rehospitalized, causing ongoing family emotional and psychological stress. Frequent readmissions also increase the health-care burden, especially in intensive care units.9, 10 A few studies have been published about readmission of pediatric tracheostomized ventilator-dependent infants; however, not much has been reported in the literature about risk factors that lead to rehospitalizations in this population.11, 12 In our study we examined the factors leading to rehospitalizations in this population. Because these factors may be modifiable, identifying them may eventually help caregivers minimize these risks and decrease subsequent hospitalizations.
In our univariate analysis model, equipment malfunction was predominantly related to tracheostomy issues, 12 out of 14 total equipment malfunctions. (Figure 6). The incidence of equipment malfunction was equally distributed over the 2 years—indicating that family/nursing familiarity with equipment, which increases over time, was not a likely factor in this finding. The incidence of equipment malfunction did not change significantly over the time period of the study despite improved parental education, discharge planning and close follow-up in the clinic. However, of note, the cohort size increased by over 4 times during the period of the study and there was progressive diminution of private duty nursing support at home over time. Equipment malfunction rates stayed the same, suggesting that of the interventions may have affected the outcomes and further prospective investigation is warranted. The univariate analysis also showed that risk factors for readmission in this population included (1) being on a ventilator at discharge, 6 months and 1 year of age, (2) oxygen dependence at 6 months and 1 year of age and (3) dependence on inhaled corticosteroids at 1 and 2 years of age. Overall, increased respiratory support in terms of ventilator dependence, oxygen requirement and inhaled corticosteroid use affected readmission rate, indicating that these factors can be used to screen patients who may need closer outpatient supervision over time. Interestingly, diuretic use at any age and the underlying comorbid conditions of the patients were not associated with an increased rate of hospital readmission. Further studies in a larger sample size will be needed to further evaluate this finding. It will be interesting to see whether underlying comorbid conditions affect the rates of weaning off the ventilator support and time to decannulation. The singular importance of the need for home ventilatory support on clinical outcomes was further illustrated in our logistic regression model that showed that ventilator dependence at 6 months and 1 year of age was strongly associated with the risk of hospital readmission.
To our knowledge, this is the first study to examine the specific factors for readmission in this age group. There are several strengths to our study. Our sample size is large, n=100, our study adds to the scant literature available for this complex patient population and our study assessed multiple factors for risk of rehospitalization through the first 2 years of life. The patients included in this study were born recently (2008 to 2015), and this minimizes the variability of ventilator strategies used to support them. The infants were all cared for in our NICU, the only tertiary referral center for children with complex illness in this geographic area. The CIPD cohort was compared by Truog et al.13 with a national registry and found to have similar characteristics and outcomes. As our population has very specific and complex medical needs, the lost-to-follow-up rate was extremely low (2%); furthermore, although our retrospective review was limited to our electronic medical record system, over 86% of regional pediatric cases, and closer to 100% of high-risk cases (unpublished CMH demographic cases), are hospitalized at our center.
Our study also had multiple limitations that must be taken into account when evaluating these results. The medical records that were accessed for the study included hospital records within our system. Outside medical records from the primary care physician, other emergency room/urgent care centers outside our system and durable medical equipment companies were not accessible. Minor equipment-related issues handled exclusively by the durable medical equipment companies at home without the need for physician intervention were not documented in our hospital records and did not affect our data related to equipment malfunction. Cristea et al.14 reported that socioeconomic status might have some impact on mortality and outcome of the patients on home ventilation. These data were not available for this cohort but warrant further evaluation in future cohorts.14
Our analyses showed that viral infections were the most common cause of hospital readmissions in this population. Taylor et al.15 have shown that viral infections cause more respiratory morbidity in preterm infants than bacterial infections. NICU surveillance studies have shown that rhinovirus can be present in NICU patients before discharge without causing traditional respiratory signs.16 Rhinovirus/enterovirus was the most frequently isolated virus in our cohort, with respiratory syncytial virus being second. This finding was likely because of strict adherence to the national palivizumab guidelines in our home neonatal tracheostomy/ventilator clinic with all infants receiving palivizumab monoclonal antibodies before discharge and in the home neonatal tracheostomy/ventilator clinic when clinically indicated.
Most readmissions in our cohort happened within the first 1.5 years of life. Close outpatient vigilance for these infants, with the opportunity for timely evaluation in the outpatient setting, could prevent hospital readmissions. In our cohort, 3% of infants were decannulated by 2 years of age. Cristea et al.17 have reported that median age of decannulation in severe BPD specific population is 37 months, and hence we plan to continue to follow these infants and assess the median age of decannulation in our cohort based on their underlying diagnosis.17 In our cohort, mortality was 4% by 2 years of age and is consistent with DeMauro et al.18 who have shown that children with tracheostomy have significantly lower risk of mortality compared with children without tracheostomies, especially in extremely preterm infants. Wootten et al.19 in 2006 reported 20% mortality in the first year of life in this population. Gien et al.7 in 2015 reported that interdisciplinary ventilator care programs can improve survival in this population. We also assert that the same approach will be helpful in preventing readmission in these patients.
In conclusion, our study further adds to the sparse literature on a quickly expanding, high-risk patient population. Our study indicates the need for close vigilance of these patients in the first 1.5 years of life and identifies risk factors for rehospitalization, including ongoing ventilator support needs, ongoing oxygen needs and inhaled steroid use—all indicators of the severity of the underlying lung disease. Interestingly, underlying comorbid medical conditions did not seem to affect rehospitalization risk in our population, further strengthening the current clinical trend of having these patients followed in a neonatal and infant home ventilator clinic as their primary medical home with close subspecialist involvement instead of having them followed primarily by a generalist and other subspecialty clinics. Diuretic use also did not seem to affect rehospitalization risk. The primary readmission cause was viral illness, with rhinovirus/enterovirus being the most common, supporting the need for good preventive care strategies for the family on how to prevent the spread of viral infections in the home, strategies that should be started before NICU discharge.
References
Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC et al. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years' experience. Pediatrics 2013; 131 (5): e1491–e1496.
Walker P, Forte V . Failed extubation in the neonatal intensive care unit. Ann Otol Rhinol Laryngol 1993; 102 (7): 489–495.
Estournet-Mathiaud B . Tracheostomy in chronic lung disease: care and follow-up. Pediatr Pulmonol 2001; 23 (Suppl): 135–136.
Keszler M . State of the art in conventional mechanical ventilation. J Perinatol 2009; 29 (4): 262–275.
Isaiah A, Moyer K, Pereira KD . Current trends in neonatal tracheostomy. JAMA Otolaryngol Head Neck Surg 2016; 142 (8): 738–742.
Zhu H, Das P, Roberson DW, Jang J, Skinner ML, Paine M et al. Hospitalizations in children with preexisting tracheostomy: a national perspective. Laryngoscope 2015; 125 (2): 462–468.
Gien J, Kinsella J, Thrasher J, Grenolds A, Abman SH, Baker CD . Retrospective analysis of an interdisciplinary ventilator care program intervention on survival of infants with ventilator-dependent bronchopulmonary dysplasia. Am J Perinatol 2016; 34: 155–163.
Sterni LM, Collaco JM, Baker CD, Carroll JL, Sharma GD, Brozek JL et al. An Official American Thoracic Society Clinical Practice Guideline: Pediatric Chronic Home Invasive Ventilation. Am J Respir Crit Care Med 2016; 193 (8): e16–e35.
Berry JG, Goldmann DA, Mandl KD, Putney H, Helm D, O'Brien J et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Serv Res 2011; 11: 117.
Noyes J . Health and quality of life of ventilator-dependent children. J Adv Nurs 2006; 56 (4): 392–403.
Graf JM, Montagnino BA, Hueckel R, McPherson ML . Pediatric tracheostomies: a recent experience from one academic center. Pediatr Crit Care Med 2008; 9 (1): 96–100.
Kun SS, Edwards JD, Ward SL, Keens TG . Hospital readmissions for newly discharged pediatric home mechanical ventilation patients. Pediatr Pulmonol 2012; 47 (4): 409–414.
Truog WE, Nyp MF, Taylor J, Gratny LL, Escobar H, Manimtim WM et al. Infants born at <29 weeks: pulmonary outcomes from a hybrid perinatal system. J Perinatol 2014; 34: 59–63.
Cristea AI, Ackerman VL, Davis SD, Carroll AE, Downs SM, Yu Z et al. Median household income: association with mortality in children on chronic ventilation at home secondary to bronchopulmonary dysplasia. Pediatr Allergy Immunol Pulmonol 2015; 28 (1): 41–46.
Taylor JB, Go MA, Nyp MF, Legino J, Norberg M, Dai H et al. Rehospitalization in infants born <29 weeks' gestation during the first 2 years of life: risk assessment. Am J Perinatol 2016; 33: 24–33.
Bennett NJ, Tabarani CM, Bartholoma NM, Wang D, Huang D, Riddell SW et al. Unrecognized viral respiratory tract infections in premature infants during their birth hospitalization: a prospective surveillance study in two neonatal intensive care units. J Pediatr 2012; 161 (5): 814–818.
Cristea AI, Carroll AE, Davis SD, Swigonski NL, Ackerman VL . Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics 2013; 132 (3): e727–e734.
DeMauro SB, D'Agostino JA, Bann C, Bernbaum J, Gerdes M, Bell EF et al. Developmental outcomes of very preterm infants with tracheostomies. J Pediatr 2014; 164 (6): 1303–1310 e2.
Wootten CT, French LC, Thomas RG, Neblett WW 3rd, Werkhaven JA, Cofer SA . Tracheotomy in the first year of life: outcomes in term infants, the Vanderbilt experience. Otolaryngol Head Neck Surg 2006; 134 (3): 365–369.
Acknowledgements
The authors wish to thank Dr. Martha Montello and the Medical Writing Center at Children's Mercy-Kansas City.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Akangire, G., Manimtim, W., Nyp, M. et al. Factors leading to rehospitalization for tracheostomized and ventilator-dependent infants through 2 years of age. J Perinatol 37, 857–863 (2017). https://doi.org/10.1038/jp.2017.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.54
This article is cited by
-
Risk of death at home or on hospital readmission after discharge with pediatric tracheostomy
Journal of Perinatology (2023)
-
Respiratory, growth, and survival outcomes of infants with tracheostomy and ventilator dependence
Pediatric Research (2021)
-
Respiratory illness and respiratory syncytial virus hospitalization in infants with a tracheostomy following prophylaxis with palivizumab
European Journal of Clinical Microbiology & Infectious Diseases (2019)