Abstract
Objective:
There is limited data characterizing the risk and impact of surgical site infection (SSI) in neonates; this makes it difficult to identify factors that increase neonatal SSI risk and to determine how SSI affects outcomes in this special population.
Study Design:
The American College of Surgeons National Surgical Improvement Program Pediatric (NSQIP-P) collected data on children undergoing surgery at children’s hospitals from 2012 to 2014. Neonates undergoing general surgical procedures were characterized with regard to demographic characteristics and comorbidities. Perioperative variables such as wound class, type of surgery and length of operation were also evaluated.
Results:
Seven thousand three hundred and seventy-nine neonates were identified in the NSQIP-P participant user file. The overall SSI rate was 2.6%. Only wound class and length of surgery were significantly associated with SSI. Furthermore, SSI was independently associated with longer length of stay, even after adjusting for covariates.
Conclusions:
This is the largest study to date analyzing SSI in neonates. We found that perioperative variables have a more significant impact on SSI than patient factors, suggesting that operation-related characteristics are influencing SSI. Furthermore, neonates with SSI are more likely to have prolonged hospitalizations even after adjusting for patient comorbidities.
Similar content being viewed by others
Introduction
Surgical site infections (SSIs) have a significant impact on postoperative morbidity and mortality as well as length and cost of hospitalization.1 Although risk factors for SSI are well-established in adults, these are less clear in children and infants.2, 3, 4 Neonates represent a special population that is thought to be at higher risk for infection due to their immature immune systems.5, 6, 7, 8, 9 Data characterizing the risk factors for and impact of SSI in neonates are limited,10, 11, 12, 13, 14, 15, 16 and the neonatal surgical population appears to be increasing.
Admissions to the neonatal intensive care unit are increasing nationwide. In 2012, neonatal intensive care unit admission rates ranged from 4% for normal birth weight infants to 84% for very low birth weight infants. From 2007 to 2012, the overall admission rate showed a relative increase of 23%.17 As care for neonates is advancing, the number of surgical interventions required in this group also increases.18 A considerable proportion of infants admitted to the neonatal intensive care unit require surgical interventions.
For this reason, it is increasingly important to further characterize SSI in this population. Previous studies suggest that perioperative factors are more important than patient factors.11, 12, 15, 16, 19 The primary aim of this study was to characterize the prevalence and risk factors for SSI in neonates using the American College of Surgeons National Surgical Quality Improvement Program-Pediatric (NSQIP-P) database. We also sought to evaluate how SSI impacts other perioperative complications and length of stay (LOS) in this population.
Methods
Data source
The NSQIP-P participant use file includes prospectively collected data on children undergoing surgery at any of the 64 participating children’s hospitals. Patients were randomly selected from a list of predefined Current Procedural Terminology (CPT) codes. The list of CPT codes is designed to capture procedures with higher postoperative complication rates. To minimize bias in patient selection, the first 35 cases are selected over an 8-day cycle. This process ensures that cases occurring on any day of the week will have an equal chance of being selected. Programs are required to submit data for 40 of the 46 8-day cycles occurring in 1 calendar year.20 Each participating hospital has a certified surgical clinical reviewer who reviews charts and follows up with patients to enter information in the database. All patients included have a 30-day follow-up, whether discharged or still in the hospital. The NSQIP-P database captures demographics, comorbidities and other preoperative risk factors, intraoperative variables and 30-day perioperative outcomes for children undergoing surgery. Data are routinely audited and excluded from the participant use file if it does not meet predefined criteria regarding case capture and accurate assignment of variables. This data set has been published for 2012, 2013 and 2014, and all 3 years were used in this study. The study protocol was evaluated by the Nemours institutional review board and deemed to be not human subject research and therefore did not require approval.
Case selection
We evaluated neonates undergoing major general surgery procedures. The NSQIP-P defines neonates as infants who were either delivered at term (>37 weeks) and had surgery within 29 days of birth or born prematurely (<37 weeks) and had surgery within 51 weeks postconceptual age.20 We included only cases designated as ‘inpatient’ and excluded patients with a postoperative LOS <1 day. These criteria helped us to exclude those cases observed for 24-h apnea monitoring after surgery, as the day of surgery is not included in the postoperative LOS calculation.
Variables
We characterized all neonates with regard to demographic characteristics, birth weight, prematurity, American Society of Anesthesiologists class and other comorbidities. We also evaluated perioperative variables such as wound class, type of surgery (anatomic location of operation) and length of operation (less than or greater than 1 h). Type of surgery was assigned by grouping CPT codes into one of the several anatomical categories. The composite outcome of SSI was assigned to any patient with a superficial, deep or organ space SSI. We chose to use the composite SSI variable rather than treating each type of SSI as an individual outcome variable as the overall event rate of 2.6% was low, but we did repeat the analyses with each type of SSI to better understand the variable impact of different types of SSIs. We also evaluated other perioperative outcomes, including postoperative complications, LOS and mortality. Postoperative complications evaluated include: bleeding requiring transfusion >25 cc kg−1 in the first 72 h postoperatively, reintubation, urinary tract infection, pneumonia, central line-associated bloodstream infection, sepsis, deep venous thrombosis, reoperation, readmission, still in hospital after 30 days, and death. Conditions that were present both preoperatively and postoperatively (such as sepsis or pneumonia) were not considered postoperative complications. Reoperation and readmission for any reason were captured in the database, not just for reasons related to the original operation. In addition, these events are captured regardless of whether they are planned or unplanned.
Statistical analysis
We evaluated the association between patient and perioperative variables and SSI using chi-squared or Fisher’s exact test, as appropriate. The distribution of the LOS was right skewed, therefore the median and interquartile range were used to summarize this variable. We tested associations between preoperative patient characteristics and comorbidities, perioperative variables and median LOS using Wilcoxon rank-sum test. All preoperative variables that were significantly associated with LOS and all complications significantly associated with SSI (P-value⩽0.05) were included in a multiple regression analysis to assess whether SSI was independently associated with increased LOS after adjusting for covariates. A Box-Cox transformation of the LOS variable with power parameter λ approaching 0, equivalent to a natural log transformation, modified this variable to a symmetric shape with a normal distribution. Stepwise backward variable selection was used. All statistical analyses were performed using SAS Enterprise Guide 5.1 (Cary, NC, USA).
Results
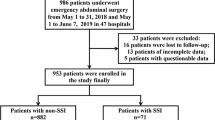
From 2012 to 2014, there were 9138 surgical cases in neonates entered into the NSQIP-P database. Of these, 1759 cases were excluded who had a postoperative LOS <1 day. After excluding those who did not have a stay in the hospital after surgery, 7379 surgical cases in neonates were included in our study. These had an overall SSI rate of 2.6% (193 cases). The majority of cases captured in the database involved infants who were born at >35 weeks gestation (N=5436) and at normal birth weight (N=4853). However, there were also 1000 cases in neonates born at <30 weeks gestation, and 1083 cases in neonates classified as very low birth weight (1 to 1.5 kg) or extremely low birth weight (<1 kg). No patient characteristics were significantly associated with SSI at a level of P=0.05 (Table 1). The patient characteristics that approached statistical significance include younger gestational age (P=0.08) and ventilator dependence (P=0.07).
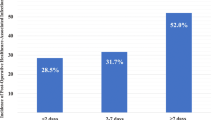
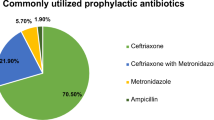
Variation in SSI rates according to perioperative variables are shown in Table 2. Abdominal cases accounted for about 90% of all neonatal general pediatric surgical cases that were captured in the database (N=6492). There were 5267 gastrointestinal cases. The anatomical location of surgery was not significantly associated with SSI (P=0.19). We found that SSI was significantly associated with higher wound class, with 4.4% of dirty/infected wound cases having an SSI vs 1.8% of clean cases (P=0.002). Longer duration of surgery was also found to be significant: operations that lasted >1 h saw a 3.1% rate of SSI vs 2.1% in those that lasted <1 h (P=0.01).
About 15% of neonates experienced at least one postoperative complication (Table 3). The most common complications were bleeding requiring transfusion of at least 25 cc kg−1 within 72 h of surgery, reintubation and SSI. Patients with SSI were more likely to experience other complications (Figure 1). Importantly, those with SSI were more likely to have postoperative sepsis (9.8% vs 1%, P<0.0001) and reoperation (21.2% vs 4.9%, P<0.0001). Neonates with SSI were also more likely than those without SSI to require readmission (15.5% vs 4.8%, P<0.0001) or to still be in the hospital at 30 days postoperatively (31.1% vs 14.9%, P<0.0001). Infants with SSI had a significantly longer LOS compared with those without SSI (median 21 days, interquartile range 9 to 42 days vs median 11 days, interquartile range 3 to 26 days, P<0.0001). In a multiple linear regression model adjusting for gender, birth weight, prematurity, ventilator status, operating room time, wound class, reintubation, reoperation, sepsis and American Society of Anesthesiologists class, SSI was independently associated with longer postoperative LOS. The difference in the average LOS for those with SSI vs those without was 2.0 days (s.e. 1.1).
Overall, we found that, of the total 193 SSIs, there were 142 superficial incisional SSIs, 16 deep incisional SSIs and 36 organ space SSIs. We repeated the bivariate analyses to determine whether patient comorbidities and/or operative characteristics were associated with each subtype of SSI, and we found that ventilator-dependent patients were more likely to have organ space SSIs (P=0.0009) and that higher wound class and longer operating room times, which were significantly associated with composite SSI, were associated with deep incisional SSI (P=0.0005) and organ space SSI (P<0.0001), respectively. We found that the association between each subtype of SSI and other postoperative complications showed a similar pattern to that of the composite SSI, except that organ space SSI was significantly associated with a greater number of other complications, including pneumonia (P<0.0001) and death (P=0.001). We repeated the multivariable linear regression evaluating association between superficial, deep and organ space SSI and increased LOS and found that both superficial and organ space infection remained significant after adjusting for covariates (similar to composite SSIs).
Discussion
With 7379 surgical cases from the NSQIP-P database, our study represents the largest present-day analysis of SSIs in neonates.15 The overall SSI rate of 2.6% was also lower than what is previously reported in neonates. Other studies had rates that ranged from 3.8% to 37%.10, 12, 13, 15, 16, 19 It seems possible that this difference could be a result of improvement in infection control over time, as the earliest study evaluated cases from 1975.19 However, it could be attributed to differences in case selection. For example, the study by Vu et al.16 selected cases for specifically contaminated and dirty wound classification, so it is not unexpected that their infection rate was higher. Furthermore, the rate of SSI in our study is comparable to the rate of SSI in older children.12, 21, 22
One might expect that the smaller and younger neonates would be more likely to experience SSI. However, this may not be the case. The only significant association we found between patient characteristics and SSI was that patients with ventilator dependence preoperatively were more likely to have organ space infections postoperatively. This may indicate that sicker patients are more likely to develop serious organ space infections, but no other patient characteristics were found to predispose patients to infection. Our findings somewhat surprisingly indicate that characteristics of the operation, rather than those of the individual patient, appear to be more important risk factors for SSI. This is similar to the conclusions of Horowitz et al.,12 who found that wound infections in children are more related to operative factors rather than the overall physiological status. Their study evaluated all pediatric age groups and included only 124 neonates, but this is also supported by other studies of neonates. Wound class and operating room time have most often been associated with higher rates of SSI,10, 11, 14, 19 while gestational age and birth weight are usually found to be insignificant.10, 11, 15, 19 This is consistent with our findings. In other neonatal SSI studies, mechanical ventilation and previous infection or positive culture were significantly associated with SSI.10, 13, 14, 16 Segal et al.15 also found type of surgery to be significant. These variables were not significantly associated with SSI in our study, but lower gestational age did approach statistical significance, and preoperative ventilator dependence was associated with organ space infection.
When considering neonates who experience SSIs, one would hypothesize that this is a generally sick group of patients and that the SSI alone is not likely to prolong their overall hospital course. Our findings did not confirm this hypothesis, as the NSQIP-P data showed that SSI was associated with higher rates of other complications and significantly longer LOS. Compared with neonates without SSI, those with SSI were more than twice as likely to still be in the hospital after 30 days; they were also four times as likely to need reoperation and almost 10 times as likely to develop sepsis. Furthermore, those with organ space infection also saw higher mortality rates. Although the causative relationship cannot be assumed, it seems plausible that SSI could lead to sepsis or reoperation. There is a paucity of data regarding complications associated with SSI, but Segal et al.15 also found that SSI was significantly associated with increased postoperative LOS. We found that SSI exerts an independent effect on LOS even after adjusting for patient characteristics, operative characteristics and other postoperative complications.
As a retrospective database study, our study has several limitations. We were unable to adjust for patient characteristics not captured in this data set, and it is possible that there are unmeasured variables that influence likelihood of SSI that were not captured. Given that our study indicates that intraoperative factors are significantly related to the development of SSIs, it is unfortunate that we were also unable to account for differences in operative technique or adherence to appropriate perioperative antibiotic dosing regimens that are likely to influence the rate of SSI. All of the operations in this data set were performed in children’s hospitals and results may not be generalizable to operations performed in infants in non-children’s hospitals. When considering the outcome variables of readmission and reoperation, it is important to consider that these events may have occurred for reasons unrelated to the original procedure or may have been planned and therefore should not necessarily be considered complications. The data set does not distinguish between planned and unplanned readmissions and reoperations. Also, the data set does not capture 100% of cases performed at participating institutions, so there is potential for sampling error. It is important to note, however, that the CPT codes included in sampling algorithm are chosen because they tend to have higher event rates, so if anything we would be likely to overestimate complication rates. Finally, the NSQIP-P participant use file does not include unique hospital identifiers, so we were unable to adjust for clustering effects within hospitals.
This study shows that perioperative variables have a more significant impact on SSI than patient factors, suggesting that risk factors for SSI in neonates should be modifiable. Systematic approaches to SSI prevention, including appropriate timing of perioperative antibiotics,23 maintenance of perioperative euthermia24 and adequate preoperative skin preparation,25 are likely to have a positive impact on even the most vulnerable patients. SSI is significantly and independently associated with longer LOS as well as postoperative bleeding, sepsis, pneumonia, reintubation, readmission and reoperation. These findings highlight the importance of optimizing the approach to perioperative neonatal care in order to minimize the incidence of SSI and thereby improve perioperative outcomes in this vulnerable population.
References
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ . The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999; 20: 725–730.
Wilson J . How to reduce the risk of surgical site infection. Nurs Times 2015; 111: 12–16.
Leaper D, Ousey K . Evidence update on prevention of surgical site infection. Curr Opin Infect Dis 2015; 28: 158–163.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR . Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999; 27: 97–132.
Kovarik J, Siegrist CA . Immunity in early life. Immunol Today 1998; 19: 150–152.
Chiswick ML Infection and defences in neonates.Br Med J (Clin Res Ed) 1983; 286: 1377–1378.
Velilla PA, Rugeles MT, Chougnet CA . Defective antigen-presenting cell function in human neonates. Clin Immunol 2006; 121: 251–259.
Miller ME . Phagocytosis in the newborn infant: humoral and cellular factors. J Pediatr 1969; 74: 255–259.
Klein Klouwenberg P, Bont L . Neonatal and infantile immune responses to encapsulated bacteria and conjugate vaccines. Clin Dev Immunol 2008; 2008: 628963.
Bojdo A, Sawicka E, Zak K, Offert B, Szamotulska K . Risk factors of surgical site infection in newborn infants. Med Wieku Rozwoj 2008; 12: 771–777.
Garcia HJ, Rodriguez-Medina X, Franco-Gutierrez M, Miranda-Novales G, Villegas-Silva R . Risk factors for surgical site infections in newborns in a neonatal intensive care unit. Rev Invest Clin 2005; 57: 425–433.
Horwitz JR, Chwals WJ, Doski JJ, Suescun EA, Cheau HW, Lally KP . Pediatric wound infections: a prospective multicenter study. Ann Surg 1998; 227: 553–558.
Lejus C, Dumont R, Gall CL, Guillaud C, Guen CG, Leclair MD et al. A preoperative stay in an intensive care unit is associated with an increased risk of surgical site infection in neonates. J Pediatr Surg 2013; 48: 1503–1508.
Rojo R, Fanjul M, Garcia-Casillas MA, Corona C, Tardaguila AR, Zornoza M et al. Surgical wound infections in newborns: analysis of risk factors. Cir Pediatr 2012; 25: 129–134.
Segal I, Kang C, Albersheim SG, Skarsgard ED, Lavoie PM . Surgical site infections in infants admitted to the neonatal intensive care unit. J Pediatr Surg 2014; 49: 381–384.
Vu LT, Vittinghoff E, Nobuhara KK, Farmer DL, Lee H . Surgical site infections in neonates and infants: is antibiotic prophylaxis needed for longer than 24 h? Pediatr Surg Int 2014; 30: 587–592.
Harrison W, Goodman D . Epidemiologic trends in neonatal intensive care, 2007-2012. JAMA Pediatr 2015; 169: 855–862.
Grover TR, Brozanski BS, Barry J, Zaniletti I, Asselin JM, Durand DJ et al. High surgical burden for infants with severe chronic lung disease (sCLD). J Pediatr Surg 2014; 49: 1202–1205.
Davenport M, Doig CM . Wound infection in pediatric surgery: a study in 1,094 neonates. J Pediatr Surg 1993; 28: 26–30.
ACS NSQIP Pediatric DATA USER GUIDE. American College of Surgeons 2015. Available at https://www.facs.org/quality-programs/pediatric/program-specifics/quality-support-tools/puf (accessed 12 December 2016).
Davis SD, Sobocinski K, Hoffmann RG, Mohr B, Nelson DB . Postoperative wound infections in a children’s hospital. Pediatr Infect Dis 1984; 3: 114–116.
Duque-Estrada EO, Duarte MR, Rodrigues DM, Raphael MD . Wound infections in pediatric surgery: a study of 575 patients in a university hospital. Pediatr Surg Int 2003; 19: 436–438.
Steinberg JP, Braun BI, Hellinger WC, Kusek L, Bozikis MR, Bush AJ et al. Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg 2009; 250: 10–16.
Tsuchida T, Takesue Y, Ichiki K, Uede T, Nakajima K, Ikeuchi H et al. Influence of peri-operative hypothermia on surgical site infection in prolonged gastroenterological surgery. Surg Infect (Larchmt) 2016; 17: 570–576.
Poulin P, Chapman K, McGahan L, Austen L, Schuler T . Preoperative skin antiseptics for preventing surgical site infections: what to do? ORNAC J 2014; 32 (12–15): 24–29.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP Pediatric are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gilje, E., Hossain, M., Vinocur, C. et al. Surgical site infections in neonates are independently associated with longer hospitalizations. J Perinatol 37, 1130–1134 (2017). https://doi.org/10.1038/jp.2017.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.107
This article is cited by
-
Factors associated with neonatal surgical site infection after abdominal surgery
Pediatric Surgery International (2022)