Abstract
Objective:
To define the impact of care standardization on caffeine and cardiorespiratory monitoring at neonatal intensive care unit (NICU) discharge.
Study Design:
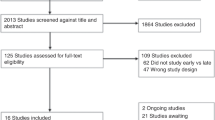
Electronic records were abstracted for infants aged 24–36 weeks gestation with birth weights appropriate for gestational age. Infants who died, transferred prior to discharge, had major pulmonary anomalies, required a home monitor for mechanical ventilation or had a family history of sudden infant death syndrome were excluded. Data and records were used to indicate when the new definition of clinically significant cardiopulmonary events (CSCPEs) and concurrent education was implemented. Preimplementation and postimplementation cohorts were compared.
Results:
Incidence fell from 74% diagnosed with apnea of prematurity at baseline to 49% diagnosed with CSCPE postimplementation (P<0.001). Infants discharged on caffeine reduced from 17% to 5% (P<0.001), and home monitor use also fell from 54% to 16% (P<0.001).
Conclusion:
Standardizing definitions and treatments reduced the use of caffeine and cardiorespiratory monitors upon NICU dismissal.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, Sept 29 to Oct 1, 1986. Pediatrics 1987; 79 (2): 292–299.
Stokowski LA . A primer on apnea of prematurity. Adv Neonatal Care 2005; 5 (3): 155–170; quiz 171–174.
Daily WJ, Klaus M, Meyer HB . Apnea in premature infants: monitoring, incidence, heart rate changes, and an effect of environmental temperature. Pediatrics 1969; 43 (4): 510–518.
Janvier A, Khairy M, Kokkotis A, Cormier C, Messmer D, Barrington KJ . Apnea is associated with neurodevelopmental impairment in very low birth weight infants. J Perinatol 2004; 24 (12): 763–768.
Barrington K, Finer N . The natural history of the appearance of apnea of prematurity. Pediatr Res 1991; 29 (4 Pt 1): 372–375.
Finer NN, Higgins R, Kattwinkel J, Martin RJ . Summary proceedings from the apnea-of-prematurity group. Pediatrics 2006; 117 (3 Pt 2): S47–S51.
Miller HC, Behrle FC, Smull NW . Severe apnea and irregular respiratory rhythms among premature infants; a clinical and laboratory study. Pediatrics 1959; 23 (4): 676–685.
Miller MJ, Martin RJ . Apnea of prematurity. Clin Perinatol 1992; 19 (4): 789–808.
Butler TJ, Firestone KS, Grow JL, Kantak AD . Standardizing documentation and the clinical approach to apnea of prematurity reduces length of stay, improves staff satisfaction, and decreases hospital cost. Jt Comm J Qual Patient Saf 2014; 40 (6): 263–269.
Hasibeder WR . Does standardization of critical care work? Curr Opin Crit Care 2010; 16 (5): 493–498.
Vermont Oxford Network. Past NICQ Collaboratives (cited 18 May 2015). Available from https://public.vtoxford.org/quality-education/quality-improvement-collaboratives/nicq-past-collaboratives.
Acknowledgements
We thank Jared Shaw, clinical systems analyst, for his assistance in accessing the data used in this manuscript. We also thank the team who led the implementation of these changes and the staff of the Neonatal Special Nurseries who initiated these changes and adapted their practices to the benefit of our patients. This work was funded by a grant from the Wichita Medical Research and Education Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Powell, M., Ahlers-Schmidt, C., Engel, M. et al. Clinically significant cardiopulmonary events and the effect of definition standardization on apnea of prematurity management. J Perinatol 37, 88–90 (2017). https://doi.org/10.1038/jp.2016.167
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.167
This article is cited by
-
Apnea, bradycardia and desaturation spells in premature infants: impact of a protocol for the duration of ‘spell-free’ observation on interprovider variability and readmission rates
Journal of Perinatology (2018)
-
Discharge without alarm(s)!
Journal of Perinatology (2018)


