Abstract
Objective:
To increase the percentage of eligible infants engaging in safe sleep practices (SSP) in two level III neonatal intensive care units (NICUs) in the Boston, Massachusetts area.
Study design:
On the basis of eligibility criteria (⩾34 weeks or ⩾1800 g without acute medical conditions), all infants were eligible for two sleep practices: SSP or NICU therapeutic positioning (NTP) depending on their gestational age, weight, clinical illness and need for therapeutic interventions. Compliance with SSP was defined as: (1) supine positioning, (2) in a flat crib with no incline, (3) without positioning devices and (4) without toys, comforters or fluffy blankets. NTP comprised usual NICU care. Nursing education was comprised of a web-based learning module and in-person teaching sessions with a study team member. Double-sided crib cards (SSP one side and NTP on the other) were attached to the bedside of every infant. Pre- and postintervention audits of all infants were carried out at both study sites. We compared compliance across all time points using generalized estimating equations to account for correlated data (SAS v9.3, Cary, NC, USA).
Result:
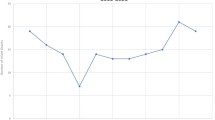
Of 755 cases, 395 (52.3%) were assessed to be eligible for SSP. From the pre- to post-intervention period, there was a significant improvement in overall compliance with SSP (25.9 to 79.7%; P-value<0.001). Adherence to each component of SSP also improved significantly following the intervention.
Conclusion:
Safe infant sleep practices can be integrated into the routine care of preterm infants in the NICU. Modeling SSP to families far in advance of hospital discharge may improve adherence to SSP at home and reduce the risk of sleep-related morbidity and mortality in this vulnerable population of infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Centers for Disease Control and Prevention. Sudden unexpected infant death and sudden infant death syndrome. Accessed on 31 March 2015. http://www.cdc.gov/sids/data.htm#resources.
Task Force on Sudden Infant Death Syndrome Task Force on Sudden Infant Death Syndrome, Moon RY . SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics 2011; 128 (5): 1030–9.
Malloy MH . Prematurity and sudden infant death syndrome: United States 2005–2007. J Perinatol 2013; 33 (6): 470–475.
Grazel R, Phalen AG, Polomano RC . Implementation of the American Academy of Pediatrics recommendations to reduce sudden infant death syndrome risk in neonatal intensive care units: an evaluation of nursing knowledge and practice. Adv Neonatal Care 2010; 10 (6): 332–342.
Vernacchio L, Corwin MJ, Lesko SM, Vezina RM, Hunt CE, Hoffman HJ et al. Sleep position of low birth weight infants. Pediatrics 2003; 111 (3): 633–640.
Hwang SS, Barfield WD, Smith RA, Morrow B, Shapiro-Mendoza CK, Prince CB et al. Discharge timing, outpatient follow-up, and home care of late-preterm and early-term infants. Pediatrics 2013; 132 (1): 101–108.
Gelfer P, Cameron R, Masters K, Kennedy KA . Integrating “Back to Sleep” recommendations into neonatal ICU practice. Pediatrics 2013; 131 (4): e1264–1270.
Smith VC, Hwang SS, Dukhovny D, Young S, Pursley DM . Neonatal intensive care unit discharge preparation, family readiness and infant outcomes: connecting the dots. J Perinatol 2013; 33 (6): 415–421.
Report of the Secretary’s Advisory Committee on Infant Mortality (SACIM): Recommendations for Department of Health and Human Services (HHS) Action and Framework for a National Strategy. January 2013. Available at http://www.hrsa.gov/advisorycommittees/mchbadvisory/InfantMortality/About/natlstrategyrecommendations.pdf (accessed on 9 July 2014).
Collaborative Improvement and Innovation Network to Reduce Infant Mortality. Available at http://mchb.hrsa.gov/infantmortality/coiin/index.html (accessed on 9 July 2014).
Shapiro-Mendoza CK, Colson ER, Willinger M, Rybin DV, Camperlengo L, Corwin MJ . Trends in infant bedding use: National Infant Sleep Position study, 1993–2010. Pediatrics 2015; 135 (1): 10–17.
Acknowledgements
We acknowledge the Program for Patient Safety and Quality from Boston Children’s Hospital for their generous grant that funded this initiative. We also acknowledge the Discharge Committee Members at South Shore Hospital who contributed to the development and implementation of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hwang, S., O'Sullivan, A., Fitzgerald, E. et al. Implementation of safe sleep practices in the neonatal intensive care unit. J Perinatol 35, 862–866 (2015). https://doi.org/10.1038/jp.2015.79
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.79
This article is cited by
-
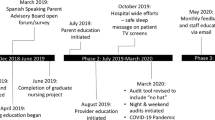
Early and consistent safe sleep practices in the neonatal intensive care unit: a sustained regional quality improvement initiative
Journal of Perinatology (2024)
-
Understanding the barriers and facilitators to safe infant sleep for mothers of preterm infants
Journal of Perinatology (2021)
-
As easy as ABC: evaluation of safe sleep initiative on safe sleep compliance in a freestanding pediatric hospital
Injury Epidemiology (2019)
-
What Do Pediatricians Tell Parents About Bed-Sharing?
Maternal and Child Health Journal (2018)
-
Implementing a Statewide Safe to Sleep Hospital Initiative: Lessons Learned
Journal of Community Health (2018)