Abstract
Objective:
To compare neonatal outcomes of preterm infants (born at <32 weeks’ gestation) with focal/spontaneous intestinal perforation (SIP), necrotizing enterocolitis (NEC)-related perforation, NEC without perforation or no NEC/perforation.
Study Design:
Retrospective cohort study of 17 426 infants admitted to Canadian neonatal intensive care units during 2010 to 2013. The primary outcome was a composite of mortality or morbidity (bronchopulmonary dysplasia, severe retinopathy, periventricular leukomalacia or nosocomial infection). Association of intestinal perforation with neonatal outcome was evaluated using multivariate logistic regression.
Result:
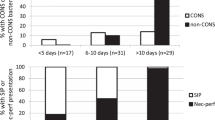
SIP was present in 178 (1.0%) infants, NEC-related perforation in 246 (1.4%) and NEC without perforation in 538 (3.1%). Any intestinal perforation was associated with higher odds of the composite outcome (adjusted odds ratio (AOR): 8.21, 95% confidence interval (95% CI) 6.26 to 10.8); however, the odds were significantly lower for focal/SIP compared with NEC-related perforation (AOR: 0.29, 95% CI 0.17 to 0.51).
Conclusion:
Of the two types of intestinal perforation, NEC-related perforation was associated with the highest risk of an adverse neonatal outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Attridge JT, Clark R, Walker MW, Gordon PV . New insights into spontaneous intestinal perforation using a national data set: (1) SIP is associated with early indomethacin exposure. J Perinatol 2006; 26: 93–99.
Buchheit JQ, Stewart DL . Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics 1994; 93: 32–36.
Novack CM, Waffarn F, Sills JH, Pousti TJ, Warden MJ, Cunningham MD . Focal intestinal perforation in the extremely-low-birth-weight infant. J Perinatol 1994; 14: 450–453.
Adderson EE, Pappin A, Pavia AT . Spontaneous intestinal perforation in premature infants: a distinct clinical entity associated with systemic candidiasis. J Pediatr Surg 1998; 33: 1463–1467.
Okuyama H, Kubota A, Oue T, Kuroda S, Ikegami R, Kamiyama M . A comparison of the clinical presentation and outcome of focal intestinal perforation and necrotizing enterocolitis in very-low-birth-weight neonates. Pediatr Surg Int 2002; 18: 704–706.
Pumberger W, Mayr M, Kohlhauser C, Weninger M . Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg 2002; 195: 796–803.
Attridge JT, Clark R, Gordon PV . New insights into spontaneous intestinal perforation using a national data set (3): antenatal steroids have no adverse association with spontaneous intestinal perforation. J Perinatol 2006; 26: 667–670.
Gordon P, Rutledge J, Sawin R, Thomas S, Woodrum D . Early postnatal dexamethasone increases the risk of focal small bowel perforation in extremely low birth weight infants. J Perinatol 1999; 19: 573–577.
Holland AJ, Shun A, Martin HC, Cooke-Yarborough C, Holland J . Small bowel perforation in the premature neonate: congenital or acquired? Pediatr Surg Int 2003; 19: 489–494.
Paquette L, Friedlich P, Ramanathan R, Seri I . Concurrent use of indomethacin and dexamethasone increases the risk of spontaneous intestinal perforation in very low birth weight neonates. J Perinatol 2006; 26: 486–492.
Alpan G, Eyal F, Vinograd I, Udassin R, Amir G, Mogle P et al. Localized intestinal perforations after enteral administration of indomethacin in premature infants. J Pediatr 1985; 106: 277–281.
Wadhawan R, Oh W, Vohr BR, Saha S, Das A, Bell EF et al. Spontaneous intestinal perforation in extremely low birth weight infants: association with indometacin therapy and effects on neurodevelopmental outcomes at 18-22 months corrected age. Arch Dis Child Fetal Neonatal Ed 2013; 98: F127–F132.
Meyer CL, Payne NR, Roback SA . Spontaneous, isolated intestinal perforations in neonates with birth weight less than 1,000 g not associated with necrotizing enterocolitis. J Pediatr Surg 1991; 26: 714–717.
Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol 2012; 32: 552–558.
Fisher JG, Jones BA, Gutierrez IM, Hull MA, Kang KH, Kenny M et al. Mortality associated with laparotomy-confirmed neonatal spontaneous intestinal perforation: A prospective 5-year multicenter analysis. J Pediatr Surg 2014; 49: 1215–1219.
Walsh MC, Kliegman RM . Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 1986; 33: 179–201.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123: 991–999.
Richardson DK, Gray JE, McCormick MC, Workman K, Goldmann DA . Score for Neonatal Acute Physiology: a physiologic severity index for neonatal intensive care. Pediatrics 1993; 91: 617–623.
Canadian Neonatal Network. Canadian Neonatal Network Abstractor's Manual. v 2.1.2, 1–94, 2014. Canadian Neonatal Network. Toronto, Canada. Available from http://www.canadianneonatalnetwork.org/portal/CNNHome/Publications.aspx (last accessed: 26 September 2014).
Bhatia AM, Stoll BJ, Cismowski MJ, Hamrick SE . Cytokine levels in the preterm infant with neonatal intestinal injury. Am J Perinatol 2014; 31: 489–496.
De Laet MH, Dassonville M, Johansson A, Lerminiaux C, Seghers V, Van den Eijnden S et al. Small-bowel perforation in very low birth weight neonates treated with high-dose dexamethasone. Eur J Pediatr Surg 2000; 10: 323–327.
Shorter NA, Liu JY, Mooney DP, Harmon BJ . Indomethacin-associated bowel perforations: a study of possible risk factors. J Pediatr Surg 1999; 34: 442–444.
Sharma R, Hudak ML, Tepas JJ III, Wludyka PS, Teng RJ, Hastings LK et al. Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol 2010; 30: 786–793.
Attridge JT, Clark R, Walker MW, Gordon PV . New insights into spontaneous intestinal perforation using a national data set: (2) two populations of patients with perforations. J Perinatol 2006; 26: 185–188.
Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg 2005; 241: 984–989.
Lai S, Yu W, Wallace L, Sigalet D . Intestinal muscularis propria increases in thickness with corrected gestational age and is focally attenuated in patients with isolated intestinal perforations. J Pediatr Surg 2014; 49: 114–119.
Merhar SL, Ramos Y, Meinzen-Derr J, Kline-Fath BM . Brain magnetic resonance imaging in infants with surgical necrotizing enterocolitis or spontaneous intestinal perforation versus medical necrotizing enterocolitis. J Pediatr 2014; 164: 410–412.
Attridge JT, Zanelli SA, Gurka MJ, Kaufman DA . Randomized controlled trials need stratification by types of acquired neonatal intestinal diseases. e-J Neonatol Res 2011; 1 (2): 59–64.
Gordon PV . Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res 2009; 65: 138–144.
Mintz AC, Applebaum H . Focal gastrointestinal perforations not associated with necrotizing enterocolitis in very low birth weight neonates. J Pediatr Surg 1993; 28: 857–860.
Tatekawa Y, Muraji T, Imai Y, Nishijima E, Tsugawa C . The mechanism of focal intestinal perforations in neonates with low birth weight. Pediatr Surg Int 1999; 15: 549–552.
Acknowledgements
We thank the staff of the Canadian Neonatal Network Coordinating Centre for their hard work, Mr Junmin Yang for statistical support and Dr Ruth Warre for providing editorial support during preparation of the manuscript. Although no funding was received specifically for this study, the Canadian Neonatal Network (CNN) received organizational support from the CNN Coordinating Centre, which is based at the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital, Toronto, Ontario, Canada. MiCare is supported by funding from the Canadian Institutes of Health Research and Mount Sinai Hospital, Toronto.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
Site investigators for the Canadian Neonatal Network
Prakesh S Shah (Director, Canadian Neonatal Network), Mount Sinai Hospital, Toronto, Ontario; Adele Harrison, Victoria General Hospital, Victoria, British Columbia; Anne Synnes, British Columbia Children’s Hospital, Vancouver, British Columbia; Zenon Cieslak, Royal Columbian Hospital, New Westminster, British Columbia; Todd Sorokan, Surrey Memorial Hospital, Surrey, British Columbia; Wendy Yee, Foothills Medical Centre, Calgary, Alberta; Khalid Aziz, Royal Alexandra Hospital, Edmonton, Alberta; Zarin Kalapesi, Regina General Hospital, Regina, Saskatchewan; Koravangattu Sankaran, Royal University Hospital, Saskatoon, Saskatchewan; Mary Seshia, Winnipeg Health Sciences Centre, Winnipeg, Manitoba; Ruben Alvaro, St Boniface General Hospital, Winnipeg, Manitoba; Sandesh Shivananda, Hamilton Health Sciences Centre, Hamilton, Ontario; Orlando Da Silva, London Health Sciences Centre, London, Ontario; Chuks Nwaesei, Windsor Regional Hospital, Windsor, Ontario; Kyong-Soon Lee, Hospital for Sick Children, Toronto, Ontario; Prakesh Shah, Mount Sinai Hospital, Toronto, Ontario; Michael Dunn, Sunnybrook Health Sciences Centre, Toronto, Ontario; Nicole Rouvinez-Bouali, Children’s Hospital of Eastern Ontario and Ottawa General Hospital, Ottawa, Ontario; Kimberly Dow, Kingston General Hospital, Kingston, Ontario; Ermelinda Pelausa, Jewish General Hospital, Montréal, Québec; Keith Barrington, Hôpital Sainte-Justine, Montréal, Québec; Christine Drolet, Centre Hospitalier Universitaire de Québec, Sainte Foy, Patricia Riley, Montréal Children’s Hospital, Montréal, Québec; Daniel Faucher, Royal Victoria Hospital, Montréal, Québec; Valerie Bertelle, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, Québec; Rody Canning, Moncton Hospital, Moncton, New Brunswick; Barbara Bulleid, Dr Everett Chalmers Hospital, Fredericton, New Brunswick; Cecil Ojah and Luis Monterrosa, Saint John Regional Hospital, Saint John, New Brunswick; Akhil Deshpandey, Janeway Children’s Health and Rehabilitation Centre, St John’s, Newfoundland; Jehier Afifi, IWK Health Centre, Halifax, Nova Scotia; Andrzej Kajetanowicz, Cape Breton Regional Hospital, Sydney, Nova Scotia; Shoo K Lee (Chairman, Canadian Neonatal Network), Mount Sinai Hospital, Toronto, Ontario.
Rights and permissions
About this article
Cite this article
Shah, J., Singhal, N., da Silva, O. et al. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol 35, 595–600 (2015). https://doi.org/10.1038/jp.2015.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.41
This article is cited by
-
Prophylactic indomethacin, antenatal betamethasone, and the risk of intestinal perforation in infants <28 weeks’ gestation
Journal of Perinatology (2023)
-
Interpretable prediction of necrotizing enterocolitis from machine learning analysis of premature infant stool microbiota
BMC Bioinformatics (2022)
-
Development of artificial neural networks for early prediction of intestinal perforation in preterm infants
Scientific Reports (2022)
-
Lipid enemas for meconium evacuation in preterm infants – a retrospective cohort study
BMC Pediatrics (2021)
-
Spontaneous intestinal perforation in premature infants: a national study
Journal of Perinatology (2021)