Abstract
Objective:
To identify characteristics associated with definitive peritoneal drainage (PD) in the extremely low birth weight infant diagnosed with spontaneous intestinal perforation (SIP). We also sought to determine whether patients requiring a second operation (salvage laparotomy) following PD are at increased risk of adverse hospital outcomes, including increased times to full enteral feedings and decreased 30-day survival.
Study Design:
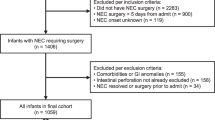
We performed a retrospective chart review of infants with a birth weight <1000 g who underwent PD for SIP at a single tertiary neonatal unit from 2003 to 2012. Infants with signs of necrotizing enterocolitis on abdominal plain films, including pneumatosis intestinalis, portal venous gas or fixed, dilated small loops of bowel were excluded from the study. Perinatal and perioperative data and short-term neonatal outcomes prior to hospital discharge were collected. Comparison was made between two groups: infants treated with definitive PD vs infants requiring salvage laparotomy. Data were analyzed using independent samples t-test and Cochrane–Mantel–Haenszel.
Result:
Eighty-nine infants who fit all inclusion criteria were identified during the study period. PD was definitive in 67 (75.3%) patients. Patients who had definitive PD vs those who required salvage laparotomy were significantly more likely to present at a later day of life (9.6±5.3 vs 5.6±2.7, P<0.0001) and to have a lower birth weight (724.6 g±132.5 vs 809.2 g±143.1, P=0.02). The administration of indomethacin or ibuprofen prior to the diagnosis of SIP was also associated with definitive PD (74.6% vs 50%, P=0.03). Comparison of feeding outcomes revealed that the time to achieve full enteral feeds was significantly longer for those who underwent a salvage laparotomy (95.9±30.2 vs 60.4±30.4 days, P<0.005). Short-term survival (>30 days) was not significantly different between the two groups.
Conclusion:
PD was definitive therapy for the majority of neonates included in this study who were referred for surgical evaluation of SIP. Our data point to trends in being able to identify infants with SIP who are at risk for salvage laparotomy following PD, and thus, adverse nutritional outcomes. Larger, prospective studies are needed to further evaluate this specific patient population and identify those patients who are likely to succeed with PD following the diagnosis of SIP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol 2012; 32: 552–558.
Gordon PV, Attridge JT . Understanding clinical literature relevant to spontaneous intestinal perforations. Am J Perinatol. 2009; 26: 309–316.
Wadhawan R, Oh W, Vohr BR, Saha S, Das A, Bell EF et al. Spontaneous intestinal perforation in extremely low birth weight infants: association with indometacin therapy and effects on neurodevelopmental outcomes at 18-22 months corrected age. Arch Dis Child Fetal Neonatal Ed 2013; 98: F127–F132.
Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol 2014; 34: 64–70.
Aschner JL, Deluga KS, Metlay LA, Emmens RW, Hendricks-Munoz KD . Spontaneous focal gastrointestinal perforation in very low birth weight infants. J Pediatr 1988; 113: 364–367.
Buchheit JQ, Stewart DL . Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics 1994; 93: 32–36.
Meyer CL, Payne NR, Roback SA . Spontaneous, isolated intestinal perforations in neonates with birth weight less than 1,000g not associated with necrotizing enterocolitis. J Pediatr Surg 1991; 26: 714–717.
Mintz AC, Applebaum H . Focal gastrointestinal perforations not associated with necrotizing enterocolitis in very low birth weight neonates. J Pediatr Surg 1993; 28: 857–860.
Okuyama H, Kubota A, Oue T, Kuroda S, Ikegami R, Kamiyama M . A comparison of the clinical presentation and outcome of focal intestinal perforation and necrotizing enterocolitis in very-low-birth-weight neonates. Pediatr Surg Int 2002; 18: 704–706.
Pumberger W, Mayr M, Kohlhauser C, Weninger M . Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg 2002; 195: 796–803.
Gordon PV . Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res 2009; 65: 138–144.
Holland AJ, Shun A, Martin HC, Cooke-Yarborough C, Holland J . Small bowel perforation in the premature neonate: congenital or acquired? Pediatr Surg Int 2003; 19: 489–494.
Hwang H, Murphy JJ, Gow KW, Magee JF, Bekhit E, Jamieson D . Are localized intestinal perforations distinct from necrotizing enterocolitis? J Pediatr Surg 2003; 38: 763–767.
Tatekawa Y, Muraji T, Imai Y, Nishijima E, Tsugawa C . The mechanism of focal intestinal perforations in neonates with low birth weight. Pediatr Surg Int 1999; 15: 549–552.
Alpan G, Eyal F, Vinograd I, Udassin R, Amir G, Mogle P et al. Localized intestinal perforations after enteral administration of indomethacin in premature infants. J Pediatr 1985; 106: 277–281.
Kuhl G, Seyberth HW . Intestinal perforations after enteral administration of indomethacin in premature infants. J Pediatr 1986; 108: 327–328.
Nagaraj HS, Sandhu AS, Cook LN, Buchino JJ, Groff DB . Gastrointestinal perforation following indomethacin therapy in very low birth weight infants. J Pediatr Surg 1981; 16: 1003–1007.
Wolf WM, Snover DC, Leonard AS . Localized intestinal perforation following intravenous indomethacin in premature infants. J Pediatr Surg 1989; 24: 409–410.
Ein SH, Marshall DG, Girvan D . Peritoneal drainage under local anesthesia for perforations from necrotizing enterocolitis. J Pediatr Surg 1977; 12: 963–967.
Janik JS, Ein SH . Peritoneal drainage under local anesthesia for necrotizing enterocolitis (NEC) perforation: a second look. J Pediatr Surg 1980; 15: 565–566.
Cass DL, Brandt ML, Patel DL, Nuchtern JG, Minifee PK, Wesson DE . Peritoneal drainage as definitive treatment for neonates with isolated intestinal perforation. J Pediatr Surg 2000; 35: 1531–1536.
Lessin MS, Luks FI, Wesselhoeft CW, Gilchrist BF, DeLuca FG . Peritoneal drainage as definitive treatment for intestinal perforation in infants with extremely low birth weight (< 750g). J Pediatr Surg 1998; 33: 370–372.
Morgan LJ, Shochat SJ, Hartman GE . Peritoneal drainage as primary management of perforated Nec in the very-low-birth-weight infant. J Pediatr Surg 1994; 29: 310–315.
Dimmitt RA, Meier AH, Skarsgard ED, Halamek LP, Smith BM, Moss RL . Salvage laparotomy for failure of peritoneal drainage in necrotizing enterocolitis in infants with extremely low birth weight. J Pediatr Surg 2000; 35: 856–859.
Rovin JD, Rodgers BM, Burns RC, McGahren ED . The role of peritoneal drainage for intestinal perforation in infants with and without necrotizing enterocolitis. J Pediatr Surg 1999; 34: 143–147.
Emil S, Davis K, Ahmad I, Straus A . Factors associated with definitive peritoneal drainage for spontaneous intestinal perforation in extremely low birth weight neonates. Eur J Pediatr Surg 2008; 18: 80–85.
Moss RL, Dimmitt RA, Barnhart DC, Sylvester KG, Brown RL, Powell DM et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis and perforation. N Engl J Med 2006; 354: 2225–2234.
Rees CM, Eaton S, Kiely EM, Wade AM, McHugh K, Pierro A . Peritoneal drainage or laparotomy for neonatal bowel perforation? A randomized controlled trial. Ann Surg 2008; 248: 44–51.
Rao SC, Basani L, Simmer K, Samnakay N, Deshpande G . Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Database Syst Rev 2011; 15CD006182.
Tam AL, Camberos A, Applebaum H . Surgical decision making in necrotizing enterocolitis and focal intestinal perforation: predictive value of radiologic findings. J Pediatr Surg 2002; 37: 1688–1691.
Gollin G, Abarbanell A, Baerg JE . Peritoneal drainage as definitive management of intestinal perforation in extremely low-birth-weight infants. J Pediatr Surg 2003; 38: 1814–1817.
Demestre X, Ginovart G, Figueras-Aloy J, Porta R, Krauel X, Garcia-Alix A et al. Peritoneal drainage as primary management in necrotizing enterocolitis: a prospective study. J Pediatr Surg 2002; 37: 1534–1539.
Baird R, Puligandla PS St, Vil D, Dube S, Laberge JM . The role of laparotomy for intestinal perforation in very low birth weight infants. J Pediatr Surg 2006; 41: 1522–1525.
Camberos A, Patel K, Applebaum H . Laparotomy in very small premature infants with necrotizing enterocolitis or focal intestinal perforation: postoperative outcome. J Pediatr Surg 2002; 37: 1692–1695.
Eicher C, Seitz G, Bevot A, Moll M, Goelz R, Arand J et al. Surgical management of extremely low birth weight infants with neonatal bowel perforation: a single-center experience and a review of the literature. Neonatology 2012; 101: 285–292.
Hunter CJ, Chokshi N, Ford HR . Evidence vs experience in the surgical management of necrotizing enterocolitis and focal intestinal perforation. J Perinatol 2008; 28 (Suppl 1): S14–S17.
Shorter NA, Liu JY, Mooney DP, Harmon BJ . Indomethacin-associated bowel perforations: a study of possible risk factors. J Pediatr Surg 1999; 34: 442–444.
Sharma R, Tepas JJ 3rd, Mollitt DL, Pieper P, Wludyka P . Surgical management of bowel perforations and outcome in very low-birth-weight infants (< or =1,200g). J Pediatr Surg 2004; 39: 190–194.
Tepas JJ 3rd, Sharma R, Hudak ML, Garrison RD, Pieper P . Coming full circle: an evidence-based definition of the timing and type of surgical management of very low-birth-weight (<1000g) infants with signs of acute intestinal perforation. J Pediatr Surg 2006; 41: 418–422.
Chan KY, Leung FW, Lam HS, Tam YH, To KF, Cheung HM et al. Immunoregulatory protein profiles of necrotizing enterocolitis versus spontaneous intestinal perforation in preterm infants. PloS One 2012; 7: e36977.
Bhatia AM, Stoll BJ, Cismowski MJ, Hamrick SE . Cytokine levels in the preterm infant with neonatal intestinal injury. Am J Perinatol 2014; 31: 489–496.
Uceda JE, Laos CA, Kolni HW, Klein AM . Intestinal perforations in infants with a very low birth weight: a disease of increasing survival?. J Pediatr Surg 1995; 30: 1314–1316.
Stokes SM, Iocono JA, Draus JM . Peritoneal drainage as the initial management of intestinal perforation in premature infants. Am Surg 2014; 80: 851–854.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jakaitis, B., Bhatia, A. Definitive peritoneal drainage in the extremely low birth weight infant with spontaneous intestinal perforation: predictors and hospital outcomes. J Perinatol 35, 607–611 (2015). https://doi.org/10.1038/jp.2015.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.23
This article is cited by
-
Comparison of preoperative and intraoperative surgeon diagnosis and pathologic findings in spontaneous intestinal perforation vs necrotizing enterocolitis
Journal of Perinatology (2024)
-
Successful conservative treatment of intestinal perforation in VLBW and ELBW neonates: a single centre case series and review of the literature
BMC Pediatrics (2019)
-
Delayed diagnosis of spontaneous intestinal perforation among very low birth weight neonates: A single center experience
Journal of Perinatology (2019)
-
Management of neonatal spontaneous intestinal perforation by peritoneal needle aspiration
Journal of Perinatology (2018)