Abstract
Objective:
Unplanned extubation events (UPEs) in neonates are hazardous to patient safety. Our goal was to reduce UPE rate (#UPEs per 100 ventilator days) by 50% in 12 months at our 25-bed level III inborn unit.
Study Design:
Baseline data were gathered prospectively for 7 months. Three Plan-Do-Study-Act (PDSA) cycles targeting main causes of UPEs were developed over the next 20 months. Causes of UPEs were analyzed using Pareto charts; and a U control chart was created with QI Charts©. Standard rules for detecting special cause variation were applied.
Result:
Mean UPE rate decreased from 16.1 to 4.5 per 100 ventilator days, a 72% decrease, exceeding our goal. Analysis of U-chart demonstrated special cause variation, with eight consecutive points below the mean. Improvement was sustained throughout the study period.
Conclusion:
UPEs in neonates can be reduced with process standardization and frontline staff education, emphasizing vigilant endotracheal tube (ETT) maintenance.
Similar content being viewed by others
Introduction
Unplanned extubation events (UPEs) in neonates are considered as a serious hazard to patient safety and have been associated with a wide range of serious life threatening consequences. Risks associated with UPE in neonates include laryngeal or tracheal injury with scarring, barotrauma, periods of inadequate oxygenation, pneumothorax, ventilator-associated pneumonia and intraventricular hemorrhage.1 UPEs in neonates have also been associated with a longer ventilation time and hospital length of stay.2, 3 However, data on outcomes of UPE, best prevention strategies in preterm and term newborns in the neonatal intensive care unit (NICU) and target rates of UPEs in this population are limited. The incidence of UPEs within NICUs is not well defined, and studies have reported rates ranging from 0.14 to 5.3 UPE per 100 ventilator days.4 These rates are significantly higher than the ones reported for the pediatric population (0.11 to 2.27 UPE per 100 ventilator days).5 Neonates are considered to be at higher risk for UPEs because of the challenges of securing an artificial airway on a small face with immature skin, longer intubation times, use of uncuffed endotracheal tubes (ETTs) and lack of routine use of sedation and paralysis while mechanically ventilated.2, 3, 4 Quality improvement studies have shown that a multi-pronged approach can reduce the rate of UPEs in the NICU.1, 3, 6, 7 There is a lack of randomized control trials addressing the best method to secure the ETT in neonates despite the high incidence of UPEs and the significant risks associated with these events. Therefore, more information is needed about strategies to reduce incidence of UPEs in the newborn population. We sought to determine our baseline unplanned extubation rate, and instituted a quality improvement initiative to reduce UPEs in our level III NICU.
Methods
Human subjects’ protection
The Institutional Review Board of Drexel University College of Medicine granted an exemption because it was implemented to improve quality of patient care and develop best practices; therefore, parental consent was not required.
Setting
This quality improvement initiative was performed at Hahnemann University Hospital, an academic, urban hospital in Philadelphia, PA, USA with a 25-bed Level III NICU. Hahnemann University Hospital has on average 2000 deliveries each year, and 350 admissions to the NICU.
Planning the intervention
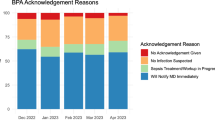
Baseline data were collected prospectively from March 2012 to October 2012, and a Pareto chart was created (Figure 1) to determine the most common factors leading to UPEs in our NICU. The Pareto diagram was presented to the Quality Improvement Committee of our NICU, a multidisciplinary team including: the unit’s medical director, nursing leadership and nursing educators. Based on feedback from this committee and analysis of the baseline period data, a key driver diagram was created and a series of process changes were developed to lower the UPE rate (Figure 2). Implementation of these better practices occurred sequentially by performing several Plan-Do-Study-Act (PDSA) cycles (Table 1).
Pareto chart for reasons noted for unplanned extubation events (UPEs) during baseline period from March to October 2012. Number of UPE is shown on the left vertical axis. Right vertical axis shows the cumulative percentage for each reason noted for UPE. Loose tape, patient movement and excessive secretions represented 84% of the reasons noted for UPE.
The initial bundle of process changes was introduced in November 2012. The primary driver of UPEs determined by our baseline data was loose tape exacerbated by excessive secretions. Therefore, we chose to focus on the ETT securing method in the first PDSA cycle. Based on a literature search and an informal survey of the area’s NICUs, we opted for the double Y-configuration, using a different tape (Kendall/Covidien, 1′ standard porous tape, Covidien, Minneapolis, MN, USA), securing the tube in a central position, and using Mastisol liquid adhesive (Ferndale Laboratories, Ferndale, MI, USA) on a Duoderm base (ConvaTec, Bridgewater, NJ, USA). Next, to ensure all nurses were trained on this standardized taping method, a series of hands-on training sessions and skills workshops with mannequins were completed over the first cycle’s 4-month period (November 2012 to February 2013). Bedside cards with ETT size and appropriate depth of insertion were also employed to aid staff with ETT maintenance. These cards were introduced to assist nursing staff and respiratory therapists with documentation, routine checks of ETT position, and to determine the need to re-secure the tube.
After introducing the new standardized ETT fixation method (PDSA cycle 1), subsequent UPEs were reviewed by the principal investigator each week. Initial failures in establishing the new method were studied by the improvement team. Analysis of the events and discussion with the staff revealed that the nursing staff as a whole did not feel comfortable with the taping method due to a lack of familiarity. Therefore, there were many different styles of securing the ETT being utilized. To increase familiarity and establish process standardization of the ETT securement method, the Quality Improvement Committee designed a more intensive education of the staff, with a hands-on in-service with a mannequin, which occurred in March 2013 (PDSA cycle 2). In addition, every nurse in the NICU had to be certified as proficient in the taping method by the nursing educator. The taping protocol was included in the training of newly hired nurses. A special educational session was also conducted with the neonatal fellows and nurse practitioners so they could become proficient in teaching the taping protocol, and be able to monitor compliance with the standardized method in the future. During this second PDSA cycle, we also initiated nurse education about the importance of ETT maintenance. The second most common associated factor with unplanned extubation based on the Pareto chart (Figure 1) was patient movement. Therefore, we emphasized consistent vigilance about proper ETT maintenance, which consisted of: documenting the ETT position at each care time, proactively reinforcing the ETT tape job and mandating that two staff members be present when handling an intubated patient during weighing, bathing, getting ready for kangaroo care and repositioning of the baby.
In June 2013, a new electronic medical record was introduced at our hospital. A place to document ETT position, re-taping, suctioning and UPEs in the electronic medical record was developed. Education on documentation of UPEs in the newly acquired electronic medical record was performed, including cards with step-by-step instructions taped on every computer on wheels. Both respiratory therapists and nursing staff were responsible to document artificial airway data on the computerized system. Medical records were audited on a monthly basis by the principal investigator and nurse educator to ensure compliance with proper documentation in the EMR of all intubated infants. Continuous staff education was provided by neonatal fellows, neonatal attendings and nurse educators during March to November 2013. Monthly data were on display in the NICU and provided positive reinforcement. This positive reinforcement led to a culture shift, where the nurses considered the taping method ‘their method’, which was a critical turning point in this initiative. Finally, from December 2013 to May 2014 (PDSA cycle 3), real-time analysis of each UPE was performed by the principal investigators by discussing and reviewing each event with the health-care providers present when it occurred. When an event occurred the principal investigators were notified by the neonatal fellow or nurse practitioner and the case was reviewed with the caretakers involved as soon as possible, usually within 48 h of the event. The circumstance in which the event happened, suspected contributing factors, as well as potential better practices were discussed. When a new admission was intubated or ETT needed re-taping, neonatal fellows and nurse practitioners would directly supervise taping technique to monitor compliance with taping protocol and give feedback to the staff and would communicate their observations to the principal investigators.
Planning the study of the intervention
Our study consisted of an observational time series in which sequential interventions were developed and introduced. Our outcome measure was UPE rate, which was calculated per month as the number of UPEs per 100 ventilator days. UPE was defined as accidental ETT dislodgement or removal at a time not ordered by a physician.1, 2, 7 We included all neonates admitted to the NICU who were intubated and mechanically ventilated for ⩾12 h, as others have done.3 We decided to focus on those infants intubated for 12 h or greater, as these are the infants who truly demonstrate a need for intubation and mechanical ventilation. Infants who were transferred or who died at less than 12 h of life were excluded. A data collection sheet was developed to document all UPEs, which included the suspected reason and the clinical scenario when the event occurred. Additional data included for each UPE were the time of the event, patient’s gestational age, day of life the event occurred, sex, weight, mode of ventilation and if re-intubation was required. Neonatal fellows, neonatal nurse practitioners and/or pediatric residents would complete the sheet with the help of the bedside nurse when a UPE occurred. Data on total ventilator days were collected from patients’ medical records.
Statistical analysis
To determine whether there was improvement after each intervention, statistical process control analyses were performed and rules for detecting special cause were applied.8 There was a different number of ventilated patients and ventilator days per month with unequal opportunity for an event. Therefore, a U-chart was created to analyze statistical process control. Means and upper and lower control limits were calculated using QI charts, Scoville Associates; 2009. Statistical analysis was performed using the Shapiro-Wilk W test for normality and non-parametric Wilcoxon signed-rank test. Analyses were performed with the JMP statistical analysis program (SAS, Cary, NC, USA). P-values <0.05 were considered to be statistically significant.
Results
After sequential process changes were developed in our NICU, our mean UPE rate decreased from 16.1 UPEs per 100 ventilator days to 4.5 UPEs per 100 ventilator days at the end of November 2013, a 72% decrease from baseline period, exceeding our goal of 50% reduction within 12 months (Figure 3). Criteria for special cause variation were established with eight consecutive points below the mean.8 During the 27-month study period, 66 infants were intubated and mechanically ventilated for ⩾12 h, for a total of 662 ventilator days. All babies were intubated orally, except one infant who was briefly intubated nasally. Median birth weight, gestational age, sex and number of ventilator days for patients with and without UPEs for the entire study period are shown in Table 2. Forty-seven percent (n=31) of the mechanically ventilated babies had birth weights less than 1000 g. Infants with and without UPEs were significantly different in all variables, except sex. Patients who had UPEs were of a lower birth weight, younger gestational age and had more ventilator days when compared to patients with no events (Table 2).
Control chart (U-chart) for unplanned extubation rate (number of unplanned extubation events (UPEs) per 100 ventilator days) from March 2012 to May 2014. Monthly UPE rate is depicted by the dotted line. Mean UPE rate throughout the study period is depicted by the solid black line. The dashed lines represent the upper and lower control limits (UCL and LCL; 3 standard deviations above and below the mean, respectively). Mean UPE rate was 15.9 during baseline period and decreased to 4.5 during cycle 2 in April 2013. There were unequal sample sizes each month.
Throughout the 7-month baseline period of March 2012 to October 2012, there were 273 infants admitted to the NICU. A total of 31 infants were intubated during this time, of which 26 were mechanically ventilated for ⩾12 h, totaling 414 ventilator days. From the intubated patients mechanically ventilated for ⩾12 h, 16 infants experienced a UPE. Three infants had a single event and 13 infants had more than one event. There were 66 UPEs during this time. The U-chart depicts the monthly UPE rate for the duration of the study period. UPE rates, number of ventilator days and number of patients in each birth weight subgroup throughout the study are shown in Table 3. Infants with birth weight <1000 g contributed the greatest number of ventilator days (359 vent days; mean 21.1 vent days/infant), most UPEs (60) and the most UPEs per infant (mean 3.5 UPEs/infant). Seventy-five percent of the patients who had UPEs during the baseline period required re-intubation.
Introduction of the new standardized taping method began in November 2012 during a nursing skills workshop. There were 579 admissions to the NICU from November 2012 to May 2014 after the first bundle of better practices was introduced (postbaseline). During this time, a total of 75 infants were intubated, of which 42 were mechanically ventilated for ⩾12 h, for a total of 248 ventilator days. Fourteen of the thirty-three excluded infants were either transferred out to our referral Level IV NICU or died before 12 h of life. Of the remaining 19 infants, the majority (13/19) were in the 29- to 36-week gestational age category, and were quickly extubated after admission to the NICU. There were 11 infants who had a total of 20 UPEs during the 20-month postbaseline period. Seventy-five percent of infants who had a UPE required re-intubation, consistent with the baseline period. The monthly UPE rate was above the mean during November 2012 to February 2013 (PDSA cycle 1), resulting in a slight increase in the mean UPE rate after the first process changes were introduced (Figure 3). UPE rate increased from 15.9 to 17.5 during this time. After discussions with bedside nurses and nursing leadership, it was determined that there was a need for a targeted education session, which occurred in March 2013 (PDSA cycle 2). Contributing factors to the continued high UPE rate were the large group of newly hired nurses not present for the initial education session, and a decrease in the number of mechanically ventilated infants, which prevented nurses from becoming more facile with the taping procedure. Staff members were continuously reminded of the importance of adhering to the new taping protocol and better practices for ETT maintenance. Nurse champions worked with the senior nursing staff on changing the culture to a focus on a team effort of proper maintenance of the ETT.
Therefore, PDSA cycle 2 focused on an intensive hands-on in-service by the nurse educator with all nursing staff about the standardized ETT fixation method, as well as a new emphasis on the ETT maintenance, whereby artificial airway data had to be documented in the electronic medical record. Positive reinforcement of improvement in the UPE rate was provided by posters displayed in the nursing lounge. The control chart shows significant improvement during PDSA cycle 2, in which we achieved a rate of zero for four consecutive months (May to August 2013), as well as 8 consecutive months (April to November 2013) in which the UPE rate was below the mean, demonstrating special cause variation (Figure 3). In December 2013, we were able to calculate a decreased mean and upper control limit, demonstrating improvement over time. These results were displayed in the NICU for positive reinforcement. To sustain improvement, PDSA cycle 3 (December 2013 to May 2014) focused on real-time analysis of each UPE, with each member of the team present when an event occurred.
The UPE rate among infants with birth weight less than 1000 g decreased by 66% (Table 3). It is difficult to have an accurate assessment of those infants who weigh 1000 to 2499 g or ⩾2500 g because there were less ventilator days in these groups. There was no difference in the incidence of UPEs between the day and the night shift, and no difference between modes of ventilation (conventional ventilator versus high-frequency oscillator). Most events occurred during patient care (for example, repositioning, weighing, suctioning, transferring from isolette to warmer and changing bedding). Some events occurred during re-taping of tube (6 events), kangaroo care (3 events) and during a lumbar puncture (1 event).
Discussion
UPE is the fourth most common adverse event in North American NICUs.9 The UPE rate in our level III NICU was unknown, and we sought to identify the baseline rate and associated factors and circumstances of UPEs. Based on analysis of our baseline period, the primary reasons for UPEs were loose tape, patient movement and excessive secretions, which is consistent with other quality improvement and observational studies.1, 2, 3, 4, 7 It is challenging to develop strategies to safely anchor and stabilize an uncuffed ETT without compromising skin integrity in the neonatal population because they have a small face with a large amount of secretions.
There are a wide variety of methods and commercially available devices for ETT fixation. Systematic reviews analyzing literature for both the pediatric and adult populations have not been able to make best practice recommendations about which method of ETT fixation is superior for the prevention of UPE.5, 10 There is a paucity of data in the neonatal population as well; according to the most recent systematic reviews on the subject, there is not enough data to support the use of one device or particular ETT securement method for mechanically ventilated neonates.4, 11 Merkel et al.7 described a successful quality improvement project in the NICU using a commercially available device to secure the ETT. Initially, there was not a significant impact on the number of UPEs after introduction of this device in their NICU; in order to attain improvement, they report requiring multiple educational sessions with frontline health-care professionals in order to familiarize staff with the new device.
There were three key factors to the improvement in the UPE rate in our unit. First, we standardized the ETT taping method. Since the literature for neonates ultimately had no clear recommendation for a specific ETT fixation method, we chose to implement a simplified method, without a commercial device, to aid in rapid training of staff and achieve standardization of practice in our NICU. Our study is consistent with previous work, indicating that standardization of the ETT stabilizing method is the major driver in a successful quality improvement initiative to improve UPE rate, rather than the specific method employed to secure the ETT.4, 5, 6, 7, 11
The second key driver in the improvement initiative was a change in the unit’s culture to a proactive attitude, whereby prevention of UPEs was considered as a team effort. We found, not unlike other quality improvement initiatives, that this culture change was not easy.6, 7 A critical turning point in the process standardization was the nurses considering the taping method ‘their method’. The dramatic decrease in the UPE rate during PDSA cycle 2 played an important role in providing positive reinforcement of how a group effort could truly effect change in our NICU. Emphasis on the importance of consistent attention to ETT maintenance was critical.
The third key driver in the improvement initiative was intensive education, which was required for nursing staff to become accustomed to a different method and new materials. Hands-on in-service sessions of all staff members, including neonatal fellows and nurse practitioners, as well as training of newly hired nurses, proved to be beneficial in our UPE rates. Real-time analysis of each event helped to identify potential better practices and monitor compliance with the established process changes, while simultaneously improving staff awareness about the problem at hand.
There are several limitations to our study. First, there were differences in the patient population during the baseline period versus post-PDSA cycle 1. The number of infants admitted with birth weights <1000 g, the group most likely to require mechanical ventilation for a more prolonged time, was significantly lower during the rest of the study period compared with baseline. Carvalho et al.3 showed that the most significant predictor of UPE was a longer mechanical ventilation time.3 It is difficult to ascertain to what degree the reduced number of very low birth weight infants, who have the highest risk of UPE, might have contributed to the overall reduction in our UPE rate. Second, our baseline UPE rate is much higher than what has been published previously, and so it could be argued that improvement was easier. Our unit is a 25-bed level III NICU, with less intubated infants because of increased use of non-invasive ventilation and early extubation, resulting in a smaller denominator in the UPE rate calculation. These practices also contributed to the large number of infants who were excluded from analysis because they were intubated for less than 12 h. Our NICU’s size and acuity is average for a level III NICU. Previous studies have been in large, level IV NICUs, where there are significant surgical populations receiving sedation and narcotics, which is not the practice in our unit.
One of the difficulties for accurate benchmarking of unplanned extubations in neonates is an inconsistent definition of a UPE. In our study, we defined a UPE as any accidental ETT dislodgement or removal at a time not ordered by a physician, a definition used by others.1, 7 However, there is discussion that a broader definition of UPE might be important to capture those infants who had the ETT removed without clear evidence of dislodgement because an infant is subjected to the additional risks of a subsequent intubation.12 Upon review of all the UPEs in our study, there were five events during the baseline period that were attributed to a plugged tube, and the patients’ ETT was removed without confirmation of dislodgement due to an acute decompensation. Based on the definition used for this quality improvement initiative, these events were not considered as a UPE. Among these five patients with ‘plugged tubes’, actual occlusion of the tube was confirmed in only one of the cases, an observation noted by others.12
The present study shows that the key drivers to the significant improvement in our UPE rate were achieved by process standardization, intensive staff education and shifting the unit’s culture to one of constant vigilance. There was an overall 72% decrease in UPE rate, which exceeded our goal of a 50% reduction. Infants with birth weight <1000 g showed significant improvement in the UPE rate. Further investigations should be conducted to determine the most appropriate definition of UPE and to develop interventions to avoid UPE in the neonatal population.
References
Loughead JL, Brennan RA, DeJulio P, Camposeo V, Wengert J, Cooke D . Reducing accidental extubation in neonoates. Jt Comm J Qual Patient Saf 2008; 34 (3): 164–170 125.
Veldman A, Trautschold T, Weib K, Fischer D, Bauer K . Characteristics and outcomes of unplanned extubation in ventilated preterm and term newborns on a neonatal intensive care unit. Paediatr Anaesth 2006; 16 (9): 968–973.
Carvalho FL, Mezzacappa MA, Calil R, Machado Hda C . Incidence and risk factors of accidental extubation in a neonatal intensive care unit. J Pediatr (Rio J) 2010; 86 (3): 189–195.
Lucas da Silva PS, Reis ME, Aguiar VE, Fonseca MC . Unplanned extubation in the neonatal ICU: A systematic review, critical appraisal, and evidence-based recommendations. Respir Care 2013; 58 (7): 1237–1245.
Lucas da Silva PS, de Carvalho WB . Unplanned extubation in pediatric critically ill patients: A systematic review and best practice recommendations. Pediatr Crit Care Med 2010; 11 (2): 287–294.
Barber JA . Unplanned extubation in the NICU. J Obstet Gynecol Neonatal Nurs 2013; 42: 233–238.
Merkel L, Beers K, Lewis MM, Stauffer J, Mujsce DJ, Kresch MJ . Reducing unplanned extubations in the NICU. Pediatrics 2014; 133 (5): e1367–e1372.
Provost LP, Murray S . The Health Care Data Guide: Learning from Data for Improvement. Jossey-Bass Publishers: San Francisco, CA, USA, 2011; 107–136.
Sharek PJ, Horbar JD, Mason W, Bisarya H, Thurm CW, Suresh G et al. Adverse events in the Neonatal Intensive Care Unit: Development, testing, and findings of a NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics 2006; 118 (4): 1332–1340.
Gardner A, Hughes D, Cook R, Henson R, Osborne S, Gardner G . Best practice in stabilization of oral endotracheal tubes: a systematic review. Aust Crit Care 2005; 18 (4)158 160–165.
Lai M, Inglis GDT, Hose K, Jardine LA, Davies MW . Methods for securing endotracheal tubes in newborn infants. Cochrane Database Syst Rev 2014; 7: CD007805.
Meyers JM, Pinheiro J, Nelson MU . Unplanned extubation in NICU patients: are we speaking the same language? J Perinatol 2015; 35: 676–677.
Acknowledgements
We acknowledge all the nursing staff, neonatal fellows and neonatal nurse practitioners at Hahnemann University Hospital who contributed to the development and implementation of this quality improvement project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fontánez-Nieves, T., Frost, M., Anday, E. et al. Prevention of unplanned extubations in neonates through process standardization. J Perinatol 36, 469–473 (2016). https://doi.org/10.1038/jp.2015.219
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.219
This article is cited by
-
Use of an airway bundle to reduce unplanned extubations in a neonatal intensive care unit
Journal of Perinatology (2024)
-
Short-term complications and long-term morbidities associated with repeated unplanned extubations
Journal of Perinatology (2021)
-
Enhanced recovery after surgery (ERAS) protocols in neonates should focus on the respiratory tract
Pediatric Surgery International (2019)
-
Counting unplanned extubations: marked variation among neonatologists
Journal of Perinatology (2017)