Abstract
Objective:
To evaluate the way to identify severe gestational diabetes mellitus (GDM) according to the Ministry of Health (MOH) criteria associated with high risk of adverse pregnancy outcomes.
Study Design:
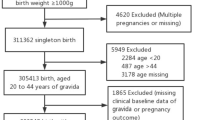
Medical records of 9803 pregnant women attending Peking University First Hospital were analyzed retrospectively. Participants diagnosed as GDM were divided into different groups according to the different number of oral glucose tolerance test (OGTT) results and the prepregnancy body mass index (BMI). Participants without GDM were included in group N. The incidence of adverse pregnancy outcomes was analyzed according to incremental differences in prepregnancy BMI and the number of abnormal OGTT result.
Result:
(1) There were 21.8% (2133/9803) women diagnosed as GDM. (2) The frequency of large for gestational age in group 2 (GDM with 2 or more abnormal OGTT value; 21.6%) was significantly higher than group 1 (GDM with only 1 abnormal OGTT value; 16.8%) and group N (13.2%), and there was also significant difference between group 1 and group N. (3) Risk of adverse pregnancy outcomes in GDM would be increased in women with prepregnancy body mass index ⩾24 kg m−2 in GDM. (4) Women with BMI <24 kg m−2 in group 1 have low risk of adverse pregnancy outcomes and seldom need insulin (1.3%) in pregnancy. (5) There were 1142 cases (53.5%) of severe GDM in this study and 991 cases (46.5%) of mild GDM.
Conclusion:
GDM women with ⩾2 abnormal OGTT values or only 1 abnormal OGTT value but with prepregnancy BMI ⩾24 kg m−2 should be recognized as severe GDM. We should pay more attention to and treat selectively with the severe GDM, especially in rural areas.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fan ZT, Yang HX, Gao XL, Lintu H, Sun WJ . Pregnancy outcome in gestational diabetes. Int J Gynaecol Obstet 2006; 94 (1): 12–16.
Ethridge JK Jr, Catalano PM, Waters TP . Perinatal outcomes associated with the diagnosis of gestational diabetes made by the international association of the diabetes and pregnancy study groups criteria. Obstet Gynecol 2014; 124 (3): 571–578.
HAPO Study Cooperative Research Group. The hyperglycemia and adverse pregnancy outcome (HAPO) study. Int J Gynaecol Obstet 2002; 78: 69–77.
The HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358: 1991–2002.
International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010; 33: 676–682.
Yang HX ; Medical Service Specialty Standard Committee of Ministry of Health. Diagnostic criteria for gestational diabetes mellitus (WS 331-2011). Chin Med J (Engl) 2012; 125: 1212–1213.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014; 37: S81–S90.
Wei Y, Yang H, Zhu W, Yang H, Li H, Yan J et al. International Association of Diabetes and Pregnancy Study Group criteria is suitable for gestational diabetes mellitus diagnosis: further evidence from China. Chin Med J (Engl) 2014; 127: 3553–3556.
Zhu WW, Yang HX, Wei YM, Yan J, Wang ZL, Li XL et al. Evaluation of the value of fasting plasma glucose in the first prenatal visit to diagnose gestational diabetes mellitus in China. Diabetes Care 2013; 36: 586–590.
Agarwal MM, Shah SM, Al Kaabi J . Gestational diabetes mellitus: confusion among medical doctors caused by multiple international criteria. J Obstet Gynaecol Res 2014; 41: 861–869.
Wang CS, Wei YM, Yang HX . Analysis of the effects of gestational diabetes mellitus based on abnormal blood glucose on pregnancy outcomes. Zhonghua Fu Chan Ke Za Zhi 2013; 48 (12): 899–902.
Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM. Weight gain during pregnancy: reexamining the guidelines. In: Rasmussen KM, Yaktine AL (eds). Pregnancy Weight Guidelines. National Academies Press (US): Washington, DC, 2009.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG et alInternational Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st). International standards for newborn weight, and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014; 384 (9946): 857–868.
Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association, Group of Pregnancy with Diabetes Mellitus, Chinese Society of Perinatal Medicine, Chinese Medical Association. Diagnosis and therapy guideline of pregnancy with diabetes mellitus. Zhonghua Fu Chan Ke Za Zhi 2014; 49 (8): 561–569.
Langer O . Obesity or diabetes: which is more hazardous to the health of the offspring? J Matern Fetal Neonatal Med 2015; 8: 1–5.
Schummers L, Hutcheon JA, Bodnar LM . Risk of adverse pregnancy outcomes by prepregnancy body mass index: a population-based study to inform prepregnancy weight loss counseling. Obstet Gynecol 2015; 125: 133–143.
Black MH, Sacks DA, Xiang AH . The relative contribution of prepregnancy overweight and obesity, gestational weight gain, and IADPSG-defined gestational diabetes mellitus to fetal overgrowth. Diabetes Care 2013; 36: 56–62.
Wahabi HA, Fayed AA, Alzeidan RA . The independent effects of maternal obesity and gestational diabetes on the pregnancy outcomes. BMC Endocr Disord 2014; 13: 14–47.
Vinturache A, Moledina N, McDonald S, Slater D, Tough S . Pre-pregnancy body mass index (BMI) and delivery outcomes in a Canadian population. BMC Pregnancy Childbirth 2014; 20: 14–422.
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J et al.; China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–1101.
Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline. Diabetes Res Clin Pract 2014; 103: 341–363.
Committee opinion no. 504: screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol 2011; 118: 751–753.
Acknowledgements
This project was supported by the Special Funds of the National Natural Science Foundation of China (Grant No. 81341020).
Author contributions
Wei Yu-mei searched the literature, collected and analyzed the data and drafted the report. Yan Jie contributed to modify the manuscript. Yang Hui-xia designed the study, contributed to discussion and reviewed and edited the manuscript. Professor Yang Hui-xia had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wei, Y., Yan, J. & Yang, H. Identification of severe gestational diabetes mellitus after new criteria used in China. J Perinatol 36, 90–94 (2016). https://doi.org/10.1038/jp.2015.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.151