Abstract
Background:
Nasal intermittent positive pressure ventilation (NIPPV) is becoming more important as a mode of ventilation in premature neonates predisposed to development of bronchopulmonary dysplasia (BPD). To the best of our knowledge, there have been no detailed studies characterizing neonates who fail NIPPV.
Objective:
To determine the differences between neonates who are successfully extubated to NIPPV and those who require re-intubation from NIPPV, and the impact of timing of NIPPV failure on BPD rates.
Study Design:
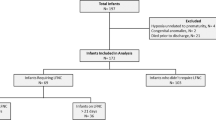
This was a retrospective cohort study in which we included infants with gestational age (GA) ⩽28 weeks and birth weight ⩽1000 g. χ2-test, analysis of variance and multivariate logistic regression models were used.
Results:
Two hundred and forty infants were studied; 180 failed NIPPV and of those, 33 (18%), 39 (22%) and 108 (60%) failed NIPPV within 0 to 6 h, ⩾6 to 24 h and ⩾24 h, respectively. Female sex and increased weight were protective against NIPPV failure (adjusted odds ratio (95% confidence interval): 0.28 (0.14 to 0.58), 0.04 (0.01 to 0.22)). Increased GA at extubation and female sex were both associated with increased time to failure (P=0.008, <0.001, respectively). Apnea was more likely the cause for failure ⩾24 h (P=0.015), whereas increased work of breathing/fraction of inspired oxygen requirements were more significant when NIPPV failure occurred earlier (P=0.001). Neonates who failed NIPPV within 24 h did not have any association with likelihood of developing BPD or severity of BPD, after adjusting for confounding variables.
Conclusion:
Significant differences in neonatal characteristics may help identify which neonates are more likely to fail NIPPV, and their timing of failure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bhandari V . Hyperoxia-derived lung damage in preterm infants. Semin Fetal Neonatal Med 2010; 15: 223–229.
The STOP-ROP Multicenter Study Group. Supplemental Therapeutic Oxygen for Prethreshold Retinopathy Of Prematurity (STOP-ROP), a randomized, controlled trial. I: Primary outcomes. Pediatrics 2000; 105: 295–310.
Gupta S, Sinha SK, Donn SM . Ventilatory management and bronchopulmonary dysplasia in preterm infants. Semin Fetal Neonatal Med 2009; 14: 367–373.
Thomson MA, Yoder BA, Winter VT, Martin H, Catland D, Siler-Khodr TM et al. Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am J Res Crit Care Med 2004; 169: 1054–1062.
Cherukupalli K, Larson JE, Rotschild A, Thurlbeck WM . Biochemical, clinical, and morphologic studies on lungs of infants with bronchopulmonary dysplasia. Pediatr Pulmonol 1996; 22: 215–229.
Bhandari V, Finer NN, Ehrenkranz RA, Saha S, Das A, Walsh MC et al. Synchronized nasal intermittent positive-pressure ventilation and neonatal outcomes. Pediatrics 2009; 124: 517–526.
Meneses J, Bhandari V, Alves JG . Nasal intermittent positive-pressure ventilation vs nasal continuous positive airway pressure for preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. Arch Pediatr Adolesc Med 2012; 166: 372–376.
Kirpalani H, Millar D, Lemyre B, Yoder BA, Chiu A, Roberts RS et al. A trial comparing noninvasive ventilation strategies in preterm infants. N Engl J Med 2013; 369: 611–620.
Bhandari V . The potential of non-invasive ventilation to decrease BPD. Semin Perinatol 2013; 37: 108–114.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics 2012; 130: 587–597.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163: 1723–1729.
Bhandari V . Nasal intermittent positive pressure ventilation in the newborn: review of literature and evidence-based guidelines. J Perinatol 2010; 30: 505–512.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A . Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol 2003; 23: 451–456.
Dumpa V, Northrup V, Bhandari V . Type and timing of ventilation in the first postnatal week is associated with bronchopulmonary dysplasia/death. Am J Perinatol 2011; 28: 321–330.
Anonymous: An international classification of retinopathy of prematurity. Pediatrics 1984; 74: 127–133.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92: 529–534.
Bell MJ TJ, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T . Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Volpe J . (ed.). Intracranial Hemorrhage: Germinal Matrix-intra-Ventricular Hemorrhage of the Premature Infant WB Saunders: Philadelphia, 2001, pp 435–447.
Fischer D, Weiss K, Buxmann H, Bremerich DH, Schloesser RL . Does short-term ventilation for semielective surgery influence the course of bronchopulmonary dysplasia in preterms? Klinische Padiatr 2009; 221: 310–311.
Ramanathan R, Sekar KC, Rasmussen M, Bhatia J, Soll RF . Nasal intermittent positive pressure ventilation after surfactant treatment for respiratory distress syndrome in preterm infants <30 weeks' gestation: a randomized, controlled trial. J Perinatol 2012; 32: 336–343.
Stefanescu BM, Murphy WP, Hansell BJ, Fuloria M, Morgan TM, Aschner JL . A randomized, controlled trial comparing two different continuous positive airway pressure systems for the successful extubation of extremely low birth weight infants. Pediatrics 2003; 112: 1031–1038.
Buzzella B, Claure N, D'Ugard C, Bancalari E . A randomized controlled trial of two nasal continuous positive airway pressure levels after extubation in preterm infants. J Pediatr 2014; 164: 46–51.
Davis P, Davies M, Faber B . A randomised controlled trial of two methods of delivering nasal continuous positive airway pressure after extubation to infants weighing less than 1000 g: binasal (Hudson) versus single nasal prongs. Arch Dis Child Fetal Neonatal Ed 2001; 85: F82–F85.
Khalaf MN, Brodsky N, Hurley J, Bhandari V . A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics 2001; 108: 13–17.
Jackson JK, Vellucci J, Johnson P, Kilbride HW . Evidence-based approach to change in clinical practice: introduction of expanded nasal continuous positive airway pressure use in an intensive care nursery. Pediatrics 2003; 111: e542–e547.
Manzar S, Nair AK, Pai MG, Paul J, Manikoth P, Georage M et al. Use of nasal intermittent positive pressure ventilation to avoid intubation in neonates. Saudi Med J 2004; 25: 1464–1467.
Kulkarni A, Ehrenkranz RA, Bhandari V . Effect of introduction of synchronized nasal intermittent positive-pressure ventilation in a neonatal intensive care unit on bronchopulmonary dysplasia and growth in preterm infants. Am J Perinatol 2006; 23: 233–240.
Owen LS, Morley CJ, Davis PG . Neonatal nasal intermittent positive pressure ventilation: a survey of practice in England. Arch Dis Child Fetal Neonatal Ed 2008; 93: F148–F150.
Sai Sunil Kishore, Dutta M, Kumar SP . Early nasal intermittent positive pressure ventilation versus continuous positive airway pressure for respiratory distress syndrome. Acta Paediatr 2009; 98: 1412–1415.
Kieran EA, Walsh H, O'Donnell CP . Survey of nasal continuous positive airways pressure (NCPAP) and nasal intermittent positive pressure ventilation (NIPPV) use in Irish newborn nurseries. Arch Dis Child Fetal Neonatal Ed 2011; 96: F156.
Medeiros SK, Carvalho WB, Soriano CF . Practices of use of nasal intermittent positive pressure ventilation (NIPPV) in neonatology in northeastern Brazil. J Pediatr (Rio J) 2012; 88: 48–53.
Dani C, Bresci C, Lista G, Martano C, Messina F, Migliori C et al. Neonatal respiratory support strategies in the intensive care unit: an Italian survey. Eur J Pediatr 2013; 172: 331–336.
Szymankiewicz M, Vidyasagar D, Gadzinowski J . Predictors of successful extubation of preterm low-birth-weight infants with respiratory distress syndrome. Pediatr Crit Care Med 2005; 6: 44–49.
Clark MT, Vergales BD, Paget-Brown AO, Smoot TJ, Lake DE, Hudson JL et al. Predictive monitoring for respiratory decompensation leading to urgent unplanned intubation in the neonatal intensive care unit. Pediatric Res 2013; 73: 104–110.
Dimitriou G, Fouzas S, Vervenioti A, Tzifas S, Mantagos S . Prediction of extubation outcome in preterm infants by composite extubation indices. Pediatr Crit Care Med 2011; 12: e242–e249.
Williamson JR, Bliss DW, Paydarfar D . Forecasting respiratory collapse: Theory and practice for averting life-threatening infant apneas. Respir Physiol Neurobioll 2013; 189: 223–231.
Vanhaesebrouck P, Allegaert K, Bottu J, Debauche C, Devlieger H, Docx M et al. The EPIBEL study: outcomes to discharge from hospital for extremely preterm infants in Belgium. Pediatrics 2004; 114: 663–675.
Farstad T, Bratlid D, Medbo S, Markestad T . Bronchopulmonary dysplasia - prevalence, severity and predictive factors in a national cohort of extremely premature infants. Acta Paediatr 2011; 100: 53–58.
Boezen HM, Jansen DF, Postma DS . Sex and gender differences in lung development and their clinical significance. Clin Chest Med 2004; 25: 237–245.
Nielsen HC, Kirk WO, Sweezey N, Torday JS . Coordination of growth and differentiation in the fetal lung. Exp Cell Res 1990; 188: 89–96.
Engoren M, Courtney SE, Habib RH . Effect of weight and age on respiratory complexity in premature neonates. J Appl Physiol 1985; 106 (3): 766–773.
Zhao J, Gonzalez F, Mu D . Apnea of prematurity: from cause to treatment. Eur J Pediatrics 2011; 170: 1097–1105.
Tang S, Zhao J, Shen J, Hu Z, Shi Y . Nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure in neonates: a systematic review and meta-analysis. Indian Pediatr 2013; 50: 371–376.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Mehta, P., Berger, J., Bucholz, E. et al. Factors affecting nasal intermittent positive pressure ventilation failure and impact on bronchopulmonary dysplasia in neonates. J Perinatol 34, 754–760 (2014). https://doi.org/10.1038/jp.2014.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.100
This article is cited by
-
Peri-extubation settings in preterm neonates: a systematic review and meta-analysis
Journal of Perinatology (2024)
-
Cardiorespiratory measures shortly after extubation and extubation outcomes in extremely preterm infants
Pediatric Research (2023)
-
A Three-Arm Randomized, Controlled Trial of Different Nasal Interfaces on the Safety and Efficacy of Nasal Intermittent Positive-Pressure Ventilation in Preterm Newborns
Indian Journal of Pediatrics (2022)
-
Should we still use vitamin A to prevent bronchopulmonary dysplasia?
Journal of Perinatology (2016)