Abstract
Objective:
To determine if increasing delivery room temperature to that recommended by the World Health Organization results in increased admission temperatures of preterm infants.
Study Design:
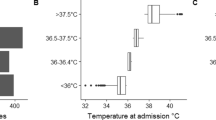
Admission rectal temperatures of newborns ⩽32 weeks gestation delivered in rooms with temperature set at 24 to 26 °C were compared with those of similar newborns delivered in rooms with temperature set at 20 to 23 °C.
Result:
Premature newborns delivered in rooms with mean temperature 25.1±0.6 °C (n=43), compared with those delivered in rooms with mean temperature 22.5±0.6 °C (n=48), had a lower incidence (34.9% vs 68.8%, P<0.01) of admission rectal temperature <36 °C and higher admission rectal temperatures (36.0±0.9 °C vs 35.5±0.8 °C, P<0.01). This difference persisted after adjustment for birth weight and 5 min Apgar score.
Conclusion:
Increasing delivery room temperatures to that recommended by the World Health Organization decreases cold stress in premature newborns.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Lyon AJ, Pikaar ME, Badger P, McIntosh N . Temperature control in very low birthweight infants during first five days of life. Arch Dis Child 1997; 76: F47–F50.
American Academy of Pediatrics, American Heart Association. Resuscitation of babies born preterm In Kattwinkel J (ed). Textbook of Neonatal Resuscitation. 6th edn. American Academy of Pediatrics: Elk Grove Village, IL, 2011.
Laptook AR, Salhab W, Bhaskar B . The Neonatal Research Network. Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatr 2007; 119: e643–e649.
Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR . The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatr 2000; 106: 659–671.
Loughead MK, Loughead JL, Reinhart MJ . Incidence and physiologic characteristics of hypothermia in the very low birth weight infant. Pediatr Nurs 1997; 23: 11–15.
Silverman WA, Fertig JW, Berger AP . The influence of the thermal environment upon survival of newly born preterm infants. Pediatr 1958; 22: 876–885.
Narendran V, Hoath SB . Thermal management of the low birth weight infant: A cornerstone of neonatology. J Pediatr 1999; 134: 529–531.
Knobel RB, Wimmer JE, Holbert D . Heat loss prevention for preterm infants in the delivery room. J Perinatol 2005; 25: 304–308.
World Health Organization (WHO). Thermal control of the newborn: a practical guide. Maternal Health and Safe Motherhood Programme (WHO/FHE/MSM/93.2). WHO: Geneva, 1996.
Kent AL, Williams J . Increasing ambient operating theatre temperature and wrapping in polyethylene improves admission temperature in premature infants. J Pediatr Child Health 2008; 44: 325–331.
Parry G, Tucker J, Tarnow-Mordi W . for the UK neonatal staffing study collaborative group. CRIB II: an update of the clinical risk index for babies score. Lancet 2003; 361: 1789–1791.
McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S . Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database Syst Rev 2010; 3: CD004210.
Vohra S, Frent G, Campbell V, Abbott M, Whyte R . Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr 1999; 134: 547–551.
Vohra S, Roberts RS, Zhang B, Janes M, Schmidt B . Heat loss prevention (HeLP) in delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very premature infants. J Pediatr 2004; 145: 750–753.
Trevisanuto D, Doglioni N, Cavallin F, Parotto M, Micaglio M, Zanardo V . Heat loss prevention in very preterm infants in delivery rooms: a prospective, randomized, controlled trial of polyethylene caps. J Pediatr 2010; 156: 914–917.
Rohana J, Khairina W, Boo NY, Shareena I . Reducing hypothermia in preterm infants with polyethylene wrap. Pediatr Int 2011; 53: 468–474.
Perlman JM, Wyllie J, Kattwinkel J, Atkins DL, Chameides L, Goldsmith JP et al. International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Part 11: neonatal resuscitation. Circulation 2010; 122: S516–S538.
Soll RF, Pfister RH . Evidence-based delivery room care of the very low birth weight infant. Neonatology 2011; 99: 349–354.
Silverman WA, Agate FJ, Fertig JW . A sequential trial of the nonthermal effect of atmospheric humidity on survival of newborn infants of low birth weight. Pediatr 1963; 31: 719–724.
Lyon AJ, Freer Y . Goals and options in keeping preterm babies warm. Arch Dis Child Fetal Neonatal Ed 2011; 96: F71–F74.
Acknowledgements
We would like to thank the staff of the Obstetrical and Neonatal Departments of the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical College for their invaluable cooperation in this study and Dr Ian Holzman for advice and critical review of the manuscript.
Author contributions
The results of this study were presented, in part, at the annual Pediatric Academic Society meeting in Boston, 28 April to 2 May 2012. This study was supported by a research grant from the Neonatal Resuscitation Program of American Academy of Pediatrics and a grant from Wenzhou City Bureau of Science and Technology, China (H20090074). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All listed authors are fully involved in the preparation of this manuscript and have approved this final version.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jia, YS., Lin, ZL., Lv, H. et al. Effect of delivery room temperature on the admission temperature of premature infants: a randomized controlled trial. J Perinatol 33, 264–267 (2013). https://doi.org/10.1038/jp.2012.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2012.100
Keywords
This article is cited by
-
Thermoregulation for very preterm infants in the delivery room: a narrative review
Pediatric Research (2024)
-
Multi-modal body part segmentation of infants using deep learning
BioMedical Engineering OnLine (2023)
-
Use of access port covers in transport incubators to improve thermoregulation during neonatal transport
Scientific Reports (2023)
-
Thermoregulation and golden hour practices in extremely preterm infants: an international survey
Pediatric Research (2023)
-
Factors associated with hypothermia within the first 6 hours of life in infants born at ≥340 weeks’ gestation: a multivariable analysis
BMC Pediatrics (2022)