Abstract
Objective:
To determine whether extremely low birth weight infants who receive enteral sterile water have a reduction in treated patent ductus arteriosus or death by 28 days compared to infants with routine management.
Study Design:
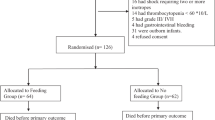
A total of 214 infants were enrolled and randomized by 36 h of age to receive up to 50 ml kg−1 per day of enteral sterile water (n=109) for 7 days or routine fluid management (n=104). Patent ductus arteriosus treatment was defined as either indomethacin treatment or surgical ligation.
Result:
The proportion of infants with a treated patent ductus arteriosus or death at <28 days of age was 63% in the sterile water group vs 64% in the control group (relative risk 0.99, 95% confidence interval 0.81 to 1.22). There were no differences in the proportion of infants in the sterile water group vs control group with a treated patent ductus arteriosus (55 vs 48%), death (21 vs 28%), necrotizing enterocolitis or death (24 vs 32%), or bronchopulmonary dysplasia or death at <28 days (80 vs 77%). Daily mean glucose levels were significantly higher (P=0.04) in control infants than sterile water infants.
Conclusion:
The use of sterile water did not decrease the incidence of patent ductus arteriosus or other adverse clinical outcomes. The role of enteral sterile water in the fluid management of extremely low birth weight infants remains uncertain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Stevenson JG . Fluid administration in the association of patent ductus arteriosus complicating respiratory distress syndrome. J Pediatr 1977; 90: 257–261.
Bell EF, Warburton D, Stonestreet BS, Oh W . Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. N Engl J Med 1980; 302: 598–604.
Bell EF, Acarregui M . Restricted versus liberal water intake for the prevention of morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2001; CD000503 Review.
Van Marter LJ, Leviton A, Allred EN, Pagano M, Kuban KC . Hydration during the first days of life and the risk of bronchopulmonary dysplasia in low birth weight infants. J Pediatr 1990; 116: 942–949.
Tammela OK, Koivisto ME . Fluid restriction for preventing bronchopulmonary dysplasia? Reduced fluid intake during the first weeks of life improves the outcome of low-birth-weight infants. Acta Paediatr 1992; 81: 207–212.
Kavvadia V, Greenough A, Dimitriou G, Hooper R . Randomised trial of fluid restriction in ventilated very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2000; 83: F91–F96.
Lorenz JM, Kleinman LI, Kotagal UR, Reller MD . Water balance in very-low-birth-weight infants: relationship to water and sodium intake and effect on outcome. J Pediatr 1982; 101: 423–432.
Gaylord MS, Lorch S, Lorch V, Wright P . The novel use of sterile water gastric drips for management of fluid and electrolyte abnormalities in extremely low birth weight infants. Neonatal Intensive Care 1995; 8: 44–48.
La Gamma EF, Ostertag SG, Birenbaum H . Failure of delayed oral feedings to prevent necrotizing enterocolitis. AJDC 1985; 139: 385–389.
Ostertag SG, LaGamma EF, Reisen CE, Ferrentino FL . Early enteral feeding does not affect the incidence of necrotizing enterocolitis. Pediatr 1986; 77: 275–280.
Berseth CL, Nordyke C . Enteral nutrients promote postnatal maturation of intestinal motor activity in preterm infants. Am J Physiol 1993; 264: G1046–G1051.
Olney CJ, Huseby V, Kennedy K, Morris BH . Sterile water gastric drip in extremely ow birth weight premature infants: a randomized trial. Am J Perinatol 2005; 22: 253–258.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R . New Ballard score expanded to include extremely premature infants. J Pediatr 1991; 119: 417–423.
Lane AT, Drost SS . Effects of repeated application of emollient cream to premature neonates' skin. Pediatrics 1993; 92: 415–419.
Nopper AJ, Horii KA, Sookdeo-Drost S, Wang TH, Mancini AJ, Lane AT . Topical ointment therapy benefits premature infants. J Pediatr 1996; 128: 660–669.
Campbell JR, Zaccaria E, Baker CJ . Systemic candidiasis in extremely low birth weight infants receiving topical petrolatum ointment for skin care: a case–control study. Pediatrics 2000; 105: 1041–1045.
Bell MJ, Ternberg JL, Feigin R, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Papile L, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights<1500 g. J Pediatr 1978; 92: 529–534.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007; 196: 147.e1–147.e8.
Bell EF, Acarregui MJ . Restricted versus liberal water intake for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2008; CD000503.
Dweck HS, Cassady G . Glucose intolerance in infants of very low birth weight. I. Incidence of hyperglycemia in infants of birth weights 1100 g or less. Pediatrics 1974; 53: 189–195.
Louik C, Mitchell AA, Epstein MF, Shapiro S . Risk factors for neonatal hyperglycemia associated with 10% dextrose infusion. AJDC 1985; 139: 783–786.
Pollak A, Cowett RM, Schwartz R, Oh W . Glucose disposal in low birth weight infants during steady state hyperglycemia: effects of exogenous insulin administration. Pediatrics 1978; 61: 546–549.
Kao LS, Morris BH, Lally KP, Stewart CD, Huseby V, Kennedy KA . Hyperglycemia and morbidity and mortality in extremely low birth weight infants. J Perinatol 2006; 26: 730–736. E-pub 24 August 2006.
Stevenson DK, Wright LL, Lemons JA, Oh W, Korones S, Papile L et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1993 through December 1994. Am J Obstet Gynecol 1998; 179: 1632–1639.
Lemons JA, Bauer CR, Oh W, Korones SB, Papile L, Stoll BJ et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995–December 1996. Pediatrics 2001; 107: url: http://www.pediatrics.org/cgi/content/full/107/1/e1.
Faustino EV, Apkon M . Persistent hyperglycemia in critically ill children. J Pediatr 2005; 146: 30–34.
Van Den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001; 345: 1359–1367.
Pittas AG, Siegel RD, Lau J . Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med 2004; 164: 2005–2011.
Acknowledgements
We appreciate the contributions of the research nurses, the staff in the NICUs, the infants and their families to this research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stewart, C., Morris, B., Huseby, V. et al. Randomized trial of sterile water by gavage drip in the fluid management of extremely low birth weight infants. J Perinatol 29, 26–32 (2009). https://doi.org/10.1038/jp.2008.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.111
Keywords
This article is cited by
-
Local growth charts for an Iranian child population aged 2–5 years in comparison with the World Health Organization Child Growth Standards
Egyptian Pediatric Association Gazette (2020)