Abstract
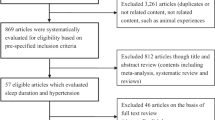
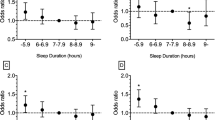
The objective of this study was to explore the age- and sex-dependent association between sleep duration and incident hypertension in a Chinese population. The Kailuan prospective cohort study recruited 101 510 participants. Those participants were followed for an average of 3.98 years and the data obtained from 32 137 participants out of 101 510 were analyzed in this study. Sleep duration was categorized as five groups of⩽5, 6, 7, 8 and ⩾9 h. Cox proportional-hazards models were used to analyze the association of sleep duration with incident hypertension. The 3.98 years’ follow-up data showed that 12 732 out of 32 137 participants developed hypertension. Short duration of sleep (⩽5 h per night) was associated with an increased risk of hypertension in woman (hazard ratio (HR) 1.27; 95% confidence interval (CI) 1.02 to 1.58) and participants aged <60 years (HR 1.11; 95% CI 1.02–1.21), when compared with the group reported with 7 h of sleep per day. This study suggested that short sleep duration could cause an increased risk of hypertension in Chinese females and population aged <60 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hajjar I, Kotchen TA . Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA 2003; 290 (2): 199–206.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42 (6): 1206–1252.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ . Selected major risk factors and global and regional burden of disease. Lancet 2002; 360 (9343): 1347–1360.
Lawes CM, Vander Hoorn S, Rodgers A . Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371 (9623): 1513–1518.
Wolk R, Gami AS, Garcia-Touchard A, Somers VK . Sleep and cardiovascular disease. Curr Prob Cardiol 2005; 30 (12): 625–662.
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 2003; 26 (2): 380–384.
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 2006; 29 (8): 1009–1014.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006; 47 (5): 833–839.
Kohatsu ND, Tsai R, Young T, Vangilder R, Burmeister LF, Stromquist AM et al. Sleep duration and body mass index in a rural population. Arch Intern Med 2006; 166 (16): 1701–1705.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB . Association between reduced sleep and weight gain in women. Am J Epidemiol 2006; 164 (10): 947–954.
Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB . Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep 2005; 28 (10): 1289–1296.
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE et al. A prospective study of sleep duration and mortality risk in women. Sleep 2004; 27 (3): 440–444.
Lusardi P, Mugellini A, Preti P, Zoppi A, Derosa G, Fogari R . Effects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjects. Am J Hypertens 1996; 9 (5): 503–505.
Kato M, Phillips BG, Sigurdsson G, Narkiewicz K, Pesek CA, Somers VK . Effects of sleep deprivation on neural circulatory control. Hypertension 2000; 35 (5): 1173–1175.
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 2004; 43 (4): 678–683.
Lusardi P, Zoppi A, Preti P, Pesce RM, Piazza E, Fogari R . Effects of insufficient sleep on blood pressure in hypertensive patients: a 24- h study. Am J Hypertens 1999; 12 (1 Pt 1): 63–68.
Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M, Heshmat R, Motlagh ME et al. The association of sleep duration and cardiometabolic risk factors in a national sample of children and adolescents: the CASPIAN III study. Nutrition 2013; 29 (9): 1133–1141.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S . Sleep quality and elevated blood pressure in adolescents. Circulation 2008; 118 (10): 1034–1040.
Paciencia I, Barros H, Araujo J, Ramos E . Association between sleep duration and blood pressure in adolescents. Hypertens Res 2013; 36 (8): 747–752.
Guo X, Zheng L, Li Y, Yu S, Liu S, Zhou X et al. Association between sleep duration and hypertension among Chinese children and adolescents. Clin Cardiol 2011; 34 (12): 774–781.
Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension 2007; 50 (4): 693–700.
Kim SJ, Lee SK, Kim SH, Yun CH, Kim JH, Thomas RJ et al. Genetic association of short sleep duration with hypertension incidence—a 6-year follow-up in the Korean genome and epidemiology study. Circulation J 2012; 76 (4): 907–913.
Wang A, Liu X, Guo X, Dong Y, Wu Y, Huang Z et al. Resting heart rate and risk of hypertension: results of the Kailuan cohort study. J Hypertens 2014; 32 (8): 1600–1605 Discussion 5.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep 2008; 31 (8): 1087–1096.
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 2005; 111 (5): 614–621.
Prinz PN . Age impairments in sleep, metabolic and immune functions. Exp Gerontol 2004; 39 (11-12): 1739–1743.
Martinez-Garcia MA, Campos-Rodriguez F, Catalan-Serra P, Soler-Cataluna JJ, Almeida-Gonzalez C, De la Cruz Moron I et al. Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment: a prospective observational study. Am J Respir Crit Care Med 2012; 186 (9): 909–916.
Stranges S, Dorn JM, Cappuccio FP, Donahue RP, Rafalson LB, Hovey KM et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. J Hypertens 2010; 28 (5): 896–902.
Spiegel K, Leproult R, Van Cauter E . Impact of sleep debt on metabolic and endocrine function. Lancet 1999; 354 (9188): 1435–1439.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141 (11): 846–850.
Yan YX, Dong J, Wu LJ, Shao S, Zhang J, Zhang L et al. Associations between polymorphisms in the glucocorticoid-receptor gene and cardiovascular risk factors in a Chinese population. J Epidemiol 2013; 23 (5): 389–395.
Yan YX, Dong J, Liu YQ, Zhang J, Song MS, He Y et al. Association of suboptimal health status with psychosocial stress, plasma cortisol and mRNA expression of glucocorticoid receptor alpha/beta in lymphocyte. Stress 2015; 18 (1): 29–34.
Gao J, Sun H, Liang X, Gao M, Zhao H, Qi Y et al. Ideal cardiovascular health behaviors and factors prevent the development of hypertension in prehypertensive subjects. Clin Exp Hypertens 2015; 37: 1–6.
Li Z, Yang X, Wang A, Qiu J, Wang W, Song Q et al. Association between ideal cardiovascular health metrics and depression in Chinese population: a cross-sectional study. Sci Rep 2015; 5: 11564.
Kario K . Obstructive sleep apnea syndrome and hypertension: mechanism of the linkage and 24- h blood pressure control. Hypertens Res 2009; 32 (7): 537–541.
Acknowledgements
We thank all study participants, their relatives, the members of the survey teams at the 11 regional hospitals of the Kailuan Medical Group, and the project development and management teams at the Beijing Tiantan hospital and the Kailuan Group.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Song, Q., Liu, X., Wang, X. et al. Age- and gender-specific associations between sleep duration and incident hypertension in a Chinese population: the Kailuan study. J Hum Hypertens 30, 503–507 (2016). https://doi.org/10.1038/jhh.2015.118
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2015.118
This article is cited by
-
Sleep duration, hypnotic drug use, and risk factors: cross- sectional study
Scientific Reports (2023)
-
The association between sleep duration and hypertension: a meta and study sequential analysis
Journal of Human Hypertension (2021)
-
Effects of sleep deprivation on endothelial function in adult humans: a systematic review
GeroScience (2021)
-
Sleep and hypertension
Sleep and Breathing (2020)
-
Correlation between sleep duration and hypertension: a dose-response meta-analysis
Journal of Human Hypertension (2019)