Abstract
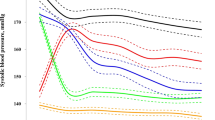
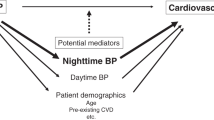
To compare the circadian variation of blood pressure (BP) between patients with intra-cerebral haemorrhage (ICH) and with cerebral infarction (CI), around-the-clock BP measurements were obtained from 89 hypertensive patients with ICH, from 63 patients with CI and from 16 normotensive volunteers. The single and population-mean cosinor yielded individual and group estimates of the MESOR (Midline Estimating Statistic Of Rhythm, a rhythm-adjusted mean value), circadian double amplitude and acrophase (measures of extent and timing of predictable daily change). Comparison shows that without any difference in BP MESOR, the circadian amplitude of systolic (S) BP was larger in ICH than CI patients (P<0.001), and both groups differed from the healthy volunteers in BP MESOR and pulse pressure (P<0.001) and in the circadian amplitude of SBP (P<0.005). The smaller population circadian amplitude of diastolic (D) BP of the ICH group (P=0.042) is likely related to a larger scatter of individual circadian acrophases in this group as compared with that in the other two groups, an inference supported by a smaller day–night ratio of DBP for ICH vs CI patients (P=0.007). Heart rate (HR) variability, gauged by the standard deviation (SD), was decreased in both patient groups as compared with that in healthy controls, more so among ICH than CI patients (P=0.025). Thus, patients with ICH had a higher incidence of abnormal circadian characteristics of BP than patients with CI, the major differences relating to a larger circadian amplitude of SBP, a smaller HR-SD, and a larger incidence of odd circadian acrophases of DBP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Kannel WB, Wolf PA, Verter J, McNamara PM . Epidemiologic assessment of the role of blood pressure in stroke: the Framingham study. JAMA 1970; 214: 301–310.
Scheinberg P . Dementia due to vascular disease: a multifactorial disorder. Stroke 1988; 19: 1291–1299.
Omae T, Ueda K . Hypertension and cerebrovascular disease: the Japanese experience. J Hypertens 1988; 6: 343–349.
Cornélissen G, Halberg F, Breus T, Syutkina EV, Baevsky R, Weydahl A et al. Non-photic solar associations of heart rate variability and myocardial infarction. J Atmos Solar-Terr Phys 2002; 64: 707–720.
Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G . Relationship of 24-h blood pressure mean and variability to severity of target-organ damage in hypertension. J Hypertens 1987; 5: 93–98.
Frattola A, Parati G, Cuspidi C, Albini F, Mancia G . Prognostic value of 24-h blood pressure variability. J Hypertens 1993; 11: 1133–1137.
Halberg F, Cornélissen G, Halberg J, Fink H, Chen C-H, Otsuka K et al. Circadian Hyper-Amplitude-Tension, CHAT: a disease risk syndrome of anti-aging medicine. J Anti Aging Med 1998; 1: 239–259.
Cornélissen G, Halberg F, Bakken EE, Singh RB, Otsuka K, Tomlinson B et al. 100 or 30 years after Janeway or Bartter, Healthwatch helps avoid ‘flying blind’. Biomed Pharmacother 2004; 58 (Suppl 1): S69–S86.
Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 1990; 81: 528–536.
Kuwajima I, Suzuki Y, Shimosawa T, Kanemaru A, Hoshino S, Kuramoto K . Diminished nocturnal decline in blood pressure in elderly hypertensive patients with left ventricular hypertrophy. Am Heart J 1992; 67: 1307–1311.
Shimada K, Kawamoto A, Matsubayashi K, Nishinaga M, Kimura S, Ozawa T . Diurnal blood pressure variations and silent cerebrovascular damage in elderly patients with hypertension. J Hypertens 1992; 10: 875–878.
Imai Y, Munakata M, Hashimoto J, Minami N, Sakuma H, Watanabe N et al. Age-specific characteristics of nocturnal blood pressure in a general population in a community of northern Japan. Am J Hypertens 1993; 6 (6 Pt 2): 179S–183S.
O’Brien E, Sheridan J, O’Malley K . Dippers and non-dippers. Lancet 1988; 2: 397.
Pickering TG, Shimbo D, Haas D . Ambulatory blood-pressure monitoring. N Engl J Med 2006; 354: 2368–2374.
Halberg F . Chronobiology: methodological problems. Acta Med Rom 1980; 18: 399–440.
Cornélissen G, Halberg F . Chronomedicine. In: Armitage P, Colton T (eds). Encyclopedia of Biostatistics, 2nd edn. John Wiley & Sons Ltd: Chichester, UK, 2005, pp 796–812.
Refinetti R, Cornélissen G, Halberg F . Procedures for numerical analysis of circadian rhythms. Biol Rhythm Res 2007; 38 (4): 275–325.
Bingham C, Arbogast B, Cornélissen Guillaume G, Lee JK, Halberg F . Inferential statistical methods for estimating and comparing cosinor parameters. Chronobiologia 1982; 9: 397–439.
Yamamoto Y, Akiguchi I, Oiwa K, Satoi H, Kimura J . Diminished nocturnal blood pressure decline and lesion site in cerebrovascular disease. Stroke 1995; 26: 829–833.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K . Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension 2001; 38: 852–857.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kimura J . Adverse effect of nighttime blood pressure on the outcome of lacunar infarct patients. Stroke 1998; 29: 570–576.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kasai T, Ozasa K . Twenty-fourhour blood pressure and MRI as predictive factors for different outcomes in patients with lacunar infarct. Stroke 2002; 33: 297–305.
Zakopoulos N, Stamatelopoulos S, Toumanidis S, Saridakis N, Trika C, Moulopoulos S . 24 h blood pressure profile affects the left ventricle independently of the pressure level. A study in untreated essential hypertension diagnosed by office blood pressure readings. Am J Hypertens 1997; 10: 168–174.
Timio M, Venanzi S, Lolli S, Lippi G, Verdura C, Monarca C et al. ‘Nondipper’ hypertensive patients and progressive renal insufficiency: a 3-year longitudinal study. Clin Nephrol 1995; 43: 382–387.
Phillips RA, Sheinart KF, Godbold JH, Mahboob R, Tuhrim S . The association of blunted nocturnal blood pressure dip and stroke in a multiethnic population. Am J Hypertens 2000; 13: 1250–1255.
Cornélissen G, Chen CH, Halberg F . Ambulatory blood-pressure monitoring. N Engl J Med 2006; 355 (8): 850.
Cornélissen G, Halberg F, Otsuka K, Singh RB, Chen CH . Chronobiology predicts actual and proxy outcomes when dipping fails. Hypertension 2007; 49: 237–239.
Cornélissen G, Schwartzkopff O, Halberg F, Otsuka K, Watanabe Y . 7-Day ambulatory monitoring for adults with hypertension and diabetes. Am J Kidney Dis 2001; 37: 878.
Otsuka K, Cornélissen G, Halberg F . Predictive value of blood pressure dipping and swinging with regard to vascular disease risk. Clin Drug Invest 1996; 11: 20–31.
Otsuka K, Cornélissen G, Halberg F, Oehlert G . Excessive circadian amplitude of blood pressure increases risk of ischemic stroke and nephropathy. J Med Eng Technol 1997; 21: 23–30.
Chen CH, Ting CT, Lin SJ, Hsu TL, Chou P, Kuo HS et al. Relation between diurnal variation of blood pressure and left ventricular mass in a Chinese population. Am J Cardiol 1995; 75: 1239–1243.
Staessen JA, Bieniaszewski L, O’Brien E, Gosse P, Hayashi H, Imai Y, et al., The ‘Ad Hoc’ Working Group. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. Hypertension 1997; 29: 30–39.
Casiglia E, Palatini P, Colangeli G, Ginocchio G, Di Menza G, Onesto C et al. 24 h rhythm of blood pressure and forearm peripheral resistance in normotensive and hypertensive subjects confined to bed. J Hypertens 1996; 14: 47–52.
Halberg F, Scheving LE, Lucas E, Cornélissen G, Sothern RB, Halberg E et al. Chronobiology of human blood pressure in the light of static (room-restricted) automatic monitoring. Chronobiologia 1984; 11: 217–247.
Tamura K, Wu J, Cornélissen G, Halberg F . Comparison of two consecutive ambulatory 24-h blood pressure and heart rate profiles in Japanese hospital staff. Chronobiologia 1989; 16: 189.
Johansson BB, Norrving B, Widner H, Wu J, Halberg F . Stroke incidence: circadian and circaseptan (about-weekly) variations in onset. Prog Clin Biol Res 1990; 341A: 427–436.
Shinagawa M, Kubo Y, Otsuka K, Ohkawa S, Cornélissen G, Halberg F . Impact of circadian amplitude and chronotherapy: relevance to prevention and treatment of stroke. Biomed Pharmacother 2001; 55 (Suppl 1): 125–132.
Gupta AK, Greenway FL, Cornélissen G, Pan W, Halberg F . Prediabetes is associated with abnormal circadian blood pressure variability. J Hum Hypertens 2008; 22 (9): 627–633.
Cornélissen G, Cugini P, Siegelova J, Fiser B, Halberg F . Cugini's minimal change hypertensive retinopathy, resolved chronobiologically while dipping fails, supports the concept of ‘pre-hypertension’. In: Halberg F, Kenner T, Fiser B, Siegelova J (eds). Proceedings, Noninvasive Methods in Cardiology 2007, Brno, Czech Republic, November 11–14, 2007 Department of Functional Diagnostics and Rehabilitation, Faculty of Medicine, Masaryk University (ISBN 978 80 7018 463 4): Brno, 2007, pp 55–61.
Acknowledgements
This study was supported by the National Nature Science Foundation of China and by CMB (No. 30470623; No. 30570902 to Z Wang; No. 30470684 to C Wan; No. 88-486 to Z Wang), by a grant from the National Institutes of Health (GM-13981 to Franz Halberg), and by the University of Minnesota Supercomputing Institute (to Germaine Cornélissen and Franz Halberg).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, Z., Li, W., Liu, Y. et al. Circadian blood pressure and heart rate characteristics in haemorrhagic vs ischaemic stroke in Chinese people. J Hum Hypertens 24, 165–174 (2010). https://doi.org/10.1038/jhh.2009.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.53