Abstract
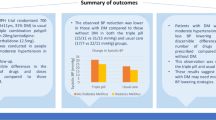
Most patients inadvertently miss an occasional dose of antihypertensive therapy, and hence drugs that provide sustained blood-pressure (BP) reduction beyond the 24-h dosing interval are desirable. The primary objective of this study was to compare the 24-h mean ambulatory BP reductions from baseline after a simulated missed dose of the direct renin inhibitor aliskiren, irbesartan or ramipril. In this double-blind study, 654 hypertensive patients (24-h mean ambulatory diastolic BP (MADBP) ⩾85 mm Hg) were randomized 1:1:1 to once-daily aliskiren 150 mg, irbesartan 150 mg or ramipril 5 mg. Doses were doubled after 2 weeks. At day 42, patients were again randomized equally within each group to receive 1 day of placebo (‘missed dose’) on either day 42 or day 49. Patients with a successful 24-h ambulatory BP measurement at baseline and on day 42/49 were included in the analyses. The 24-h mean ambulatory systolic BP (MASBP)/MADBP reductions from baseline after a missed dose of aliskiren 300 mg (9.3/7.0 mm Hg) were similar to irbesartan 300 mg (9.5/7.3 mm Hg) and significantly larger than ramipril 10 mg (7.1/5.0 mm Hg, P⩽0.008). Loss of BP-lowering effect with aliskiren in the 24 h after a missed dose (1.0/0.7 mm Hg for 24–48-h vs 0–24-h MASBP/MADBP) was significantly lower than with irbesartan (3.6/2.2 mm Hg, P<0.01) or ramipril (4.0/2.6, P<0.0001). This equates to maintenance of 91/91% of the MASBP/MADBP-lowering effect with aliskiren, greater than irbesartan (73/77%) or ramipril (64/65%). The incidence of adverse events was similar across treatments (32.9–36.0%), although ramipril treatment was associated with an increased incidence of cough (ramipril, 6.1%; aliskiren, 0.5%; irbesartan, 1.8%). Aliskiren 300 mg provided a sustained BP-lowering effect beyond the 24-h dosing interval, with a significantly smaller loss of BP-lowering effect in the 24–48 h period after dose than irbesartan 300 mg or ramipril 10 mg.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Burnier M . Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens 2006; 19: 1190–1196.
Egan BM, Lackland DT, Cutler NE . Awareness, knowledge, and attitudes of older Americans about high blood pressure: implications for health care policy, education, and research. Arch Intern Med 2003; 163: 681–687.
Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003; 348: 2407–2415.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M . Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336: 1114–1117.
Frampton JE, Curran MP . Aliskiren: a review of its use in the management of hypertension. Drugs 2007; 67: 1767–1792.
Limoges D, Dieterich H-A, Yeh C-M, Vaidyanathan S, Howard D, Dole WP . A study of dose-proportionality in the pharmacokinetics of the oral direct renin inhibitor aliskiren in healthy subjects. Int J Clin Pharmacol Ther 2008; 46: 252–258.
Waldmeier F, Glaenzel U, Wirz B, Oberer L, Schmid D, Seiberling M et al. Absorption, distribution, metabolism, and elimination of the direct renin inhibitor aliskiren in healthy volunteers. Drug Metab Dispos 2007; 35: 1418–1428.
Oh BH, Mitchell J, Herron JR, Chung J, Khan M, Keefe DL . Aliskiren, an oral renin inhibitor, provides dose-dependent efficacy and sustained 24-h blood pressure control in patients with hypertension. J Am Coll Cardiol 2007; 49: 1157–1163.
Andersen K, Weinberger MH, Egan B, Constance CM, Ali MA, Jin J et al. Comparative efficacy and safety of aliskiren, an oral direct renin inhibitor, and ramipril in hypertension: a 6-month, randomized, double-blind trial. J Hypertens 2008; 26: 589–599.
Elliott HL, Elawad M, Wilkinson R, Singh SP . Persistence of antihypertensive efficacy after missed doses: comparison of amlodipine and nifedipine gastrointestinal therapeutic system. J Hypertens 2002; 20: 333–338.
Myers MG, Leenen FH . The impact of one or two missed doses on the duration of action of combined perindopril and indapamide. J Hum Hypertens 2007; 21: 86–93.
White WB, Lacourciere Y, Davidai G . Effects of the angiotensin II receptor blockers telmisartan versus valsartan on the circadian variation of blood pressure: impact on the early morning period. Am J Hypertens 2004; 17: 347–353.
Lacourciere Y, Asmar R . A comparison of the efficacy and duration of action of candesartan cilexetil and losartan as assessed by clinic and ambulatory blood pressure after a missed dose, in truly hypertensive patients: a placebo-controlled, forced titration study. Candesartan/Losartan Study Investigators. Am J Hypertens 1999; 12: 1181–1187.
Goyal D, Chong AY, Watson RL, Prasad N, Watson RD . Assessment of single versus twice daily dosing of ramipril by ambulatory blood pressure monitoring in patients similar to those included in the HOPE study. J Hum Hypertens 2007; 21: 525–530.
Azizi M, Menard J . Combined blockade of the renin–angiotensin system with angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists. Circulation 2004; 109: 2492–2499.
Uresin Y, Taylor AA, Kilo C, Tschope D, Santonastaso M, Ibram G et al. Efficacy and safety of the direct renin inhibitor aliskiren and ramipril alone or in combination in patients with diabetes and hypertension. J Renin Angiotensin Aldosterone Syst 2007; 8: 190–198.
Wood JM, Maibaum J, Rahuel J, Grutter MG, Cohen NC, Rasetti V et al. Structure-based design of aliskiren, a novel orally effective renin inhibitor. Biochem Biophys Res Commun 2003; 308: 698–705.
Danser AH, Charney A, Feldman DL, Nussberger J, Fisher N, Hollenberg N . The renin rise with aliskiren: it's simply stoichiometry. Hypertension 2008; 51: e27–e28 (Letter).
Acknowledgements
PP, WJ and ES participated in the writing of the study protocol, approved the final protocol, participated in the collection, analysis and interpretation of data as well as in the writing of the paper, and also approved the final paper. JB, CB and DLK participated in the design of the study and in the writing of the study protocol, approved the final protocol, supported the undertaking of the study, participated in the analysis and interpretation of the data as well as in the writing of the paper, and also approved the final paper. The authors take full responsibility for the content of the paper but thank Dr Richard White (Oxford PharmaGenesis™ Ltd) for assistance in collating the comments of the authors and editing the final paper. This work was funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
List of principal investigators
Brazil: Heno F Lopes, Osvaldo Kohlmann, Andrea Brandao, Virginia de Abreu, Lilian da Costa, Mario Torus Neves; Canada: Guy Chouinard, Guy Tellier, John Li, Brian Zidel, John C Fulop, Frederick F Jardine; Germany: Claudia Ulbrich, Reiner T Lehmann, Eberhardt Meier, Bjoern Paschen, Peder-Lars Stahnke, Eva Borbas, Hilmar Boeneke, Ernst Radermacher, Claus-Werner Blauth, Anton Strobel, Eckhard Massmann, Juergen Merke, Sigrid Gessner, Hans-Joachim Ulmer, Josef Junggeburth, Ludger Luetticke; Hungary: Tamas Forster, Janos Penzes, Judit Simon, Akos Kalina, Denes Pall, Emoke Csupor; Italy: Lucio Mos, Paolo Palatini, Flavio Scanferla, Valter Donadon, Massimo Santonastaso, Mario Sprovieri, Roberto Fogari, Natale Antonio Varì, Enrico Agabiti-Rosei, Roberto Pedrinelli, Maurizio Destro, Antonio Vinciguerra, Giuseppe Lembo, Claudio Ferri, Giuseppe Licata, Pier Giuseppe Agostoni, Giuseppe Guzzardi, Raffaele De Caterina, Claudio Borghi; Netherlands: Hans Prak, Peter Coenen, Harry Van Mierlo, AFE Bots, Hugo Rol, Robertus Costongs, Paulus Meurs, Willibrordus de Backer, Adriaan de Jong; Norway: Jørn Gronert, Asgeir Græsdal, Hans Olav Høivik, Sigbjørn Elle, Lasse G Gøranson, Dan Nørager, Charlotte Jacobsen, Russia: Eugene Shlyakhto, Inna Brodskaya, Tatiana Tyurina, Elena Baranova, Tatiana Novikova, Marina Balliuzek; Slovakia: Jan Murin, Jozef Semetko, Dagmar Okalova, Mikulas Szakacs, Viliam Bugan, Marian Snincak; Spain: Isabel Irizar, Ander Larrazabal, Francisco Valls Roca, Jose L Lafuente, Ana Puertas, Jose Abellan Aleman, Fernando Hernandez, Josefina Olivan, Pablo Gomez, Antonio Ortega, Carlos Calvo Gomez, Josep Lluis Fernandez Roure, Arturo Saenz Fernandez, Isidro Lopez, Jose A Dura Garcia, Jose Tolosana.
Rights and permissions
About this article
Cite this article
Palatini, P., Jung, W., Shlyakhto, E. et al. Maintenance of blood-pressure-lowering effect following a missed dose of aliskiren, irbesartan or ramipril: results of a randomized, double-blind study. J Hum Hypertens 24, 93–103 (2010). https://doi.org/10.1038/jhh.2009.38
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.38
Keywords
This article is cited by
-
How drug onset rate and duration of action affect drug forgiveness
Journal of Pharmacokinetics and Pharmacodynamics (2024)
-
What should patients do if they miss a dose? A systematic review of patient information leaflets and summaries of product characteristics
European Journal of Clinical Pharmacology (2021)
-
In silico profiling of systemic effects of drugs to predict unexpected interactions
Scientific Reports (2018)
-
Efficacy, safety, and tolerability of antihypertensive therapy with aliskiren/amlodipine in clinical practice in Austria. The RALLY (Rasilamlo long lasting efficacy) study
Wiener klinische Wochenschrift (2015)
-
Renin Inhibitors and Cardiovascular and Renal Protection: An Endless Quest?
Cardiovascular Drugs and Therapy (2013)