Abstract
We have previously examined the clinical manifestations, treatments and prognosis of 177 patients with urea cycle disorders (UCDs) from January 1999 to March 2009 in Japan. In this study, we investigated the incidence of clinical manifestations in different peak blood ammonia level at onset in UCD patients, and examined the growth of OTCD (ornithine transcarbamylase deficiency) patients. The UCD patients who had a high peak blood ammonia level at onset showed significantly high incidence of convulsion and abnormal head computed tomography or magnetic resonance imaging. The patients also showed significantly high incidence of hemodialysis and liver transplantation. Choice of therapeutic agents for long-term treatment is not different between peak blood ammonia levels at the onset, except for the use of special amino-acid formulas. Growth retardation is not affected by high peak blood ammonia level at onset; however, 32% of male and 52% of female OTCD patients over 1 year old were plotted under the 10th percentile, and showed growth failure. The final height of the male and female OTCD patients were 166.2±5.5 and 150.3±7.2 cm, respectively. Although the prognosis of UCDs was improved significantly, it is considered that there are still many difficulties in the UCD patient's life.
Similar content being viewed by others
Introduction
The urea cycle is a metabolic pathway that eliminates excess endogenous and exogenous nitrogen by detoxification of ammonia into urea.1 OTCD (ornithine transcarbamylase deficiency) is an X-linked disorder, whereas CPSD (carbamoyl phosphate synthetase 1 deficiency), ASD (argininosuccinate synthetase deficiency), ALD (argininosuccinate lyase deficiency) and AGD (argininosuccinate synthase deficiency) are autosomal recessive disorders.2 Sodium benzoate and/or sodium phenylbutyrate are used as an alternate pathway treatment,3, 4 in addition to low protein diet, for the treatment of urea cycle disorders (UCDs). In all UCDs, except for AGD, there is arginine deficiency; therefore, l-arginine is provided as a treatment for all UCDs other than AGD.5 Treatment with essential amino acids and l-carnitine are recommended in these patients.6 Treatment with l-citrulline is recommended in patients with OTCD and CPSD in place of l-arginine.7, 8 Hemodialysis is more effective than peritoneal dialysis to remove blood ammonia.9 Cases in which the general condition of UCD patients cannot be controlled using medical therapy, liver transplantation becomes necessary.10 We previously studied the long-term outcome and treatment of UCD patients.11 As compared with previous studies, we found that the prognosis and neurological symptoms of the UCD patients improved with early treatment. Growth retardation is one of the common problems for those patients who may need food restriction. In Japanese OTCD patients, l-arginine treatment is revealed to reduce attacks of hyperammonemia and to increase their growth.5 In this study, we investigated the incidence of clinical manifestations in different peak blood ammonia level at onset in UCD patients, and examined growth of OTCD patients after long-term treatment.
Patients and methods
Study patients
The investigation using a questionnaire was described previously.11 In brief, of the 928 institutions, 668 (72%) responded, and of these 668 institutions, 125 had treated patients with UCD. A second questionnaire was then sent to these 125 institutions in 2009, of which 87 (70%) responded. A third short questionnaire was then sent to these 87 institutions in 2014, of which 81 (93%) responded. Although the questionnaire was filled by many doctors, the form of the questionnaire to check clinical symptoms, to fill in the laboratory data, would minimize the variability caused by a doctor's experience. The definition of clinical manifestations applied in this study was the same as that proposed in the previous studies.11, 12, 13 Cognitive evaluations to diagnose intellectual disability were performed by a pediatrician or child psychiatrist who treated patients with UCDs. The patient’s IQ was evaluated using standardized tests such as the Wechsler Intelligence Scale for Children (WISC) or the Wechsler Adult Intelligence Scale (WAIS). IQ under 70 was estimated as an intellectual disability.
This study was approved by the ethics committee of the Faculty of Life Science of Kumamoto University (Kumamoto, Japan).
Statistical analysis
Peak blood ammonia levels of the UCD patients were analyzed to estimate significant relationships between clinical manifestations and treatments using the Mann–Whitney U-test with IBM SPSS version 19 (IBM Corp., Armonk, NY, USA). To assess the relationship between peak blood ammonia level, clinical manifestations and treatments, the patients were divided into three groups according to their peak blood ammonia level: <180, 180–360 and >360 μmol l−1. A P-value <0.05 was considered statistically significant. The height of OTCD male and female patients was expressed in terms of mean±s.d. values.
Results
The relationship between peak blood ammonia levels, clinical manifestations and treatments are shown in Figure 1. The presence of convulsions and abnormal head computed tomography or magnetic resonance imaging was significantly higher in UCD patients with a peak blood ammonia level >360 μmol l−1. Growth retardation was found in two-third or more cases in the all peak blood ammonia level groups. Feeding disturbance was not found in the patients with peak blood ammonia level ⩽360 μmol l−1. Compared with other treatment methods, a significantly higher number of patients were treated with hemodialysis, liver transplantation and special amino-acid formulas when their peak blood ammonia levels exceeded 360 μmol l−1. Hemodialysis was performed for 71% of the patients who had ammonia levels >360 μmol l−1, which indicated poor prognosis.
Relationship between peak blood ammonia levels, clinical manifestations and treatments in patients with urea cycle disorder (UCD). The relationship between the number of UCD patients with (gray bars) or without (blank bars) manifestations and the peak blood ammonia levels are shown according to the following variables: (a) growth retardation, (b) feeding disturbance, (c) convulsion, (d) abnormal head CR or MRI image, (e) hemodialysis, (f) liver transplantation, (g) protein restriction, (h) special amino-acid formulas, (i) l-arginine, (j) sodium benzoate, (k) l-citrulline and (l) sodium phenylbutyrate.
l-Arginine and sodium benzoate were frequently used in all peak blood ammonia level groups. Less than 30% of the UCD patients in each peak blood ammonia level group were given l-citrulline and sodium phenylbutyrate. There was no significant relationship between the peak blood ammonia level and treatment with l-arginine, sodium benzoate, l-citrulline and sodium phenylbutyrate.
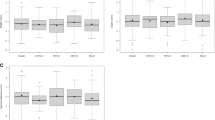
Figures 2a and b show the height of male and female OTCD patients. The height of 32% (10/31) of the male OTCD patients and 52% (24/46) of the female OTCD patients was below the 10th percentile. The mean height of male OTCD patients aged >17 years was 166.2±5.5 cm (n=10; Figure 2a and Table 1). The mean height of female OTCD patients aged >15 years was 150.3±7.2 cm (n=13; Figure 2b and Table 1). Average standard deviation of height in each age group was −0.79 to −1.04 in male OTCD patients, except adolescence period, which growth spurt may be different from the onset of puberty. Average standard deviation of height of female OTCD patients was −0.20 during childhood and −0.73 to −1.48 from school age to adult.
Stature of OTCD patients. This figure was constructed with the age of OTCD patients on the abscissa and the stature of patients with OTCD on the ordinate. Percentiles are based on data from Japanese 2000 growth reports provided by the Ministry of Health, Labor and Welfare in Japan. (a) Stature of male patients with OTCD. (b) Stature of female patients with OTCD.
Discussion
We have previously reported that an onset peak blood ammonia level <180 μmol l−1 is an indicator of good prognosis, and a level >360 μmol l−1 indicates a poor prognosis.11 In the present study, the presence or absence of clinical manifestations and treatment were evaluated according to these ammonia levels, and the characteristics of UCD patients with a higher ammonia level were determined. The presence of convulsions and abnormal head CT or MRI imaging was significantly greater in the UCD patients with a peak blood ammonia level >360 μmol l−1, which showed that the neurologic prognosis was clearly poor in these patients. More than 50% of the patients in each peak blood ammonia level group received protein restriction, which may have resulted in growth failure. Feeding disturbance occurred only in the part of patients with ammonia >360 μm, which indicated severe disturbance in UCDs. Protein restriction, prescription of l-arginine, l-citrulline and sodium benzoate were used for patients with UCD irrespective of the ammonia concentration in the blood. In Japan, l-arginine and sodium benzoate are frequently used for UCD treatment.11 At that time of our questionnaire, the government of Japan had not authorized l-citrulline, sodium benzoate and sodium phenylbutyrate for the treatment of patients with UCD. Sodium phenylbutyrate was eventually authorized in 2013.14 l-citrulline has been supplied as food from the Japanese Society for Inherited Metabolic Diseases since 2011.14 These additional treatment options may improve the prognosis of patients with UCD in the future.
Growth retardation is one of the common symptoms in UCD patients.1, 15, 16 This study revealed that 72% (47/65) of the UCD patients showed growth retardation based on the questionnaire, but the severity of growth failure was unclear. Further investigation of statures of OTCD patients showed that 32% of male patients were below the height 10th percentile, and the standard deviation of average height was −0.79 in the male patients. It shows us that growth failure of UCD patients may persist into adult. Surprisingly, 52% of female OTCD patients were below the height 10th percentile, and that the average height of the female patient who reached adulthood was 150.3 cm. This estimated final height was ~10 cm lower compared with that of the average height of Japanese adult female.12 Moreover, the degree of growth failure was aggravated during school age to adult compared with childhood. After the onset, OTCD female patients were often associated with a poor prognosis.15, 17, 18 To evaluate the state and prognosis of the OTCD female patients, characteristics of growth failure in this research may be a convenient and useful index. A secondary mitochondria block by OTCD, a brain damage by hyperammonemia, a protein restriction and metabolic instability might cause the growth retardation.5, 19
Difference in the onset of puberty and parental heights sometimes complicates the analysis. The difference in s.d. value in these ages may reflect the difference of the onset of puberty. However, the s.d. value over 17 years in boys and over 15 years in girls are consistent with those of 6–10-year- old boys and 6–9-year-old girls. These result suggested that the growth failure would be an outcome of difficult treatment of OTCD. Parental heights are important for predicted height. However, the parental heights were not available in this survey. It is sometimes inevitable in rare diseases that final heights are evaluated to compare the difference in s.d. value between the average heights of patients and healthy individuals.5 Because the cases were limited, averages of final heights were shown to indicate influence of UCDs in this study. Future prospective study may be necessary with a patient registration system such as JaSMIn (Japan Registration System for Metabolic and Inherited Diseases, http://www.jasmin-mcbank.com/).
This study has a few limitations. It is a retrospective study with some biases including hospitals and diagnosis. However, this study revealed the relationship between peak blood ammonia level and clinical manifestation, and also evaluated the growth failure in OTCD patients, who may often have to be treated with food and protein restriction. These finding may bring us careful treatment for UCD patients.
References
Brusilow, S. W. & Horwich, A. L. in The Metabolic and Molecular Bases of Inherited Disease 8th edn (eds Scriver, C. R., Beaudet, A. L., Sly, W. S. & Valle, D.) 1909 (McGraw-Hill, New York, NY, USA, 2001).
Matsuda, I. & Tanase, S. The ornithine transcarbamylase (OTC) gene: mutations in 50 Japanese families with OTC deficiency. Am. J. Med. Genet. 71, 378–383 (1997).
Brusilow, S. W., Valle, D. L. & Batshaw, M. New pathways of nitrogen excretion in inborn errors of urea synthesis. Lancet 2, 452–454 (1979).
Brusilow, S.W. Phenylacetylglutamine may replace urea as a vehicle for waste nitrogen excretion. Pediatr. Res. 29, 147–150 (1991).
Nagasaka, H., Yorifuji, T., Murayama, K., Kubota, M., Kurokawa, K., Murakami, T. et al. Effects of arginine treatment on nutrition, growth and urea cycle function in seven Japanese boys with late-onset ornithine transcarbamylase deficiency. Eur. J. Pediatr. 165, 618–624 (2006).
Leonard, J. V. The nutritional management of urea cycle disorders. J. Pediatr. 138, S40–S44 (2001).
Feillet, F. & Leonard, J. V. Alternative pathway therapy for urea cycle disorders. J. Inherit. Metab. Dis. 21, 101–111 (1998).
Batshaw, M. L., MacArthur, R. B. & Tuchman, M. Alternative pathway therapy for urea cycle disorders: twenty years later. J. Pediatr. 138, S46–S54 (2001).
Schaefer, F., Straube, E., Oh, J., Mehls, O. & Mayatepek, E. Dialysis in neonates with inborn errors of metabolism. Nephrol. Dial. Transplant. 14, 910–918 (1999).
Uemoto, S., Yabe, S., Inomata, Y., Nishizawa, H., Asonuma, K., Egawa, H. et al. Coexistence of a graft with the preserved native liver in auxiliary partial orthotopic liver transplantation from a living donor for ornithine transcarbamylase deficiency. Transplantation 63, 1026–1028 (1997).
Kido, J., Nakamura, K., Mitsubuchi, H., Ohura, T., Takayanagi, M., Matsuo, M. et al. Long-term outcome and intervention of urea cycle disorders in Japan. J. Inherit. Metab. Dis. 35, 777–785 (2012).
Kido, J., Nakamura, K., Matsumoto, S., Mitsubuchi, H., Ohura, T., Shigematsu, Y. et al. Current status of hepatic glycogen storage disease in Japan: clinical manifestations, treatments and long-term outcomes. J. Hum. Genet. 58, 285–292 (2013).
Smit, G. P. The long-term outcome of patients with glycogen storage diseases. J. Inherit. Metab. Dis. 13, 411–418 (1990).
Nakamura, K., Kido, J., Mitsubuchi, H. & Endo, F. Diagnosis and treatment of urea cycle disorders in Japan. Pediatr. Int. 56, 506–509 (2014).
Maestri, N. E., Brusilow, S. W., Clissold, D. B. & Bassett, S. S. Long-term treatment of girls with ornithine transcarbamylase deficiency. N. Engl. J. Med. 335, 855–859 (1996).
Matsuda, I., Nagata, N., Matsuura, T., Oyanagi, K., Tada, K., Narisawa, K. et al. Retrospective survey of urea cycle disorders: Part 1. Clinical and laboratory observations of thirty-two Japanese male patients with ornithine transcarbamylase deficiency. Am. J. Med. Genet. 38, 85–89 (1991).
Nassogne, M. C., Héron, B., Touati, G., Rabier, D. & Saudubray, J. M. Urea cycle defects: management and outcome. J. Inherit. Metab. Dis. 28, 407–414 (2005).
Uchino, T., Endo, F. & Matsuda, I. Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J. Inherit. Metab. Dis. 21, 151–159 (1998).
Häberle, J., Boddaert, N., Burlina, A., Chakrapani, A., Dixon, M., Huemer, M. et al. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J. Rare Dis. 7, 32 (2012).
Acknowledgements
This study was supported, in part, by a Grant-in-Aid for the Promotion of Science and Ministry of Education, Culture, Sports, Science and Technology; a Grant-in-Aid for Pediatric Research from the Ministry of Health, Labor and Welfare; and a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology; and a Grant-in-Aid for the research on rare and intractable diseases, Health and Labor Sciences Research. We thank Drs T Ohura, M Takayanagi, M Matsuo, M Yoshino, Y Shigematsu, T Yorifuji, M Kasahara and R Horikawa for data collection and discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nakamura, K., Kido, J., Matsumoto, S. et al. Clinical manifestations and growth of patients with urea cycle disorders in Japan. J Hum Genet 61, 613–616 (2016). https://doi.org/10.1038/jhg.2016.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2016.17
This article is cited by
-
Long-term effects of medical management on growth and weight in individuals with urea cycle disorders
Scientific Reports (2020)