Abstract
CXCL14 is a chemokine that has previously been implicated in insulin resistance in mice. In humans, the role of CXCL14 in metabolic processes is not well established, and we sought to determine whether CXCL14 is a risk susceptibility gene important in fetal programming of metabolic disease. For this purpose, we investigated whether CXCL14 is differentially regulated in human umbilical cords of infants with varying birth weights. We found an elevated expression of CXCL14 in human low birth weight (LBW) cords, as well as in cords from nutritionally restricted Macaca fascicularis macaques. To further analyze the regulatory mechanisms underlying the expression of CXCL14, we examined CXCL14 in umbilical cord-derived mesenchymal stem cells (MSCs) that provide an in vitro cell-based system amenable to experimental manipulation. Using both whole frozen cords and MSCs, we determined that site-specific CpG methylation in the CXCL14 promoter is associated with altered expression, and that changes in methylation are evident in LBW infant-derived umbilical cords that may indicate future metabolic compromise through CXCL14.
Similar content being viewed by others
Introduction
Suboptimal development during early fetal life because of unfavorable environmental conditions in utero poses a risk for the later development of metabolic diseases such as type 2 diabetes mellitus, cardiovascular disease and obesity.1, 2 An adverse fetal environment can result in growth restriction but there is a large body of evidence showing that although fetal growth is a proxy for an adverse fetal environment, long-term consequences can occur in the absence of growth impairment. The factors contributing to the increased disease susceptibility in the affected children likely involve epigenetic mechanisms such as DNA methylation; changes known to be influenced by maternal nutrition.3 The early identification of children who have been epigenetically programmed by a less than optimal fetal environment could enable early preventive interventions. Indeed, it has previously been shown that epigenetic differences at birth independent of birth weight predict adiposity in later life.3
We previously studied the transcriptome and epigenome in umbilical cord tissue obtained from babies enrolled in the Singapore-based longitudinal cohort study GUSTO.4 Among the differentially expressed transcripts was CXCL14 that was found to be upregulated in umbilical cords from babies born with low birth weight (LBW) and at early gestational age.5 CXCL14 has been shown to mediate insulin sensitivity in fat and muscle tissue, among other pleiotropic functions.6, 7, 8, 9 It is thought that CXCL14 acts as a regulator of glucose metabolism via an as yet unidentified membrane receptor, establishing a cross-talk between CXCL14 and insulin pathway signaling that results in the inhibition of glucose uptake. In white adipose tissue, CXCL14 mediates insulin resistance via chemotactic recruitment of macrophages (reviewed in Hara and Nakayama7).
To determine whether CXCL14 is an early biomarker of metabolic dysfunction in the offspring, we utilized human and non-human primate (NHP) tissues to demonstrate variations in CXCL14 expression in association with altered maternal nutrition. We report that in addition to changes in CXCL14 expression, we found associated epigenetic changes within the CXCL14 gene consistent with altered epigenetic regulation at specific CpGs located proximal to the activator protein 1 (AP1) binding site in the promoter of the gene. Together, these results describe the potential for CXCL14 as a functionally relevant transcriptional and epigenetic biomarker of metabolic disease that is stably represented across different tissues and ages, and conserved across primate species.
Materials and methods
Clinical populations and sample collection
All umbilical cord specimens were derived from babies born at either the KK Women’s and Children’s Hospital (KKH) or the National University Hospital (NUH) in Singapore. These hospitals contribute all the subjects to the GUSTO birth cohort study.4 Written parental consent to participate in the study was given. Ethical approval was granted by the ethics boards of both KKH and NUH, the centralized Institute Review Board (CIRB) and Domain Specific Review Board (DSRB), respectively.
Umbilical cord-derived mesenchymal stem cells (UC-MSCs)
Umbilical cord specimens were obtained from infants born at the NUH. Ethics approval was granted by the NUH-DSRB and written parental consent and participation was obtained at antenatal checkups, with normal and small-for-gestational age (SGA) infants identified through regular ultrasound scans, and confirmed at birth, where SGA was defined as fetal growth between the 5th and <10th percentile. Primary MSC lines were derived from umbilical cord Wharton’s jelly following a normal delivery. The cords were collected and processed to retrieve MSCs according to a previously published protocol.10 The characterization of these cells has been described in more detail elsewhere.11 UC-MSC lines were maintained in medium (Dulbecco’s modified Eagle’s medium high glucose with 20% fetal bovine serum, 2 mmol l−1 L-glutamine, 1 × Insulin-Transferrin-Selenium G, 5 ng ml−1 basic fibroblast growth factor, 0.1 mmol l−1 b-ME, 1 × Antibiotic/antimycotic mix) and cultured for a maximum of 10 passages.
NHP caloric restriction cohorts
All animal procedures were approved by and conducted in compliance with the standards of the Agri-Food and Veterinary Authority of Singapore and the Singapore Health Services Institutional Animal Care and Use Committee (Singhealth IACUC #2008/SHS/418). Sexually mature macaques (Macaca fascicularis) were housed in groups of 1 male to 3 females to allow for natural breeding. Early pregnancy detection was achieved by regular ultrasound scans of female breeders. Measurement of the greatest length of the embryo was used to calculate the gestational age. After confirmation of pregnancy, dams were housed in individual cages in a screened roof compound with a daily temperature range of 26–32 °C and constant humidity of 84%. Food intake was individually monitored and regulated throughout pregnancy. Pregnant dams were randomly assigned into caloric restricted or control cohorts. Control dams had access to ad libitum food (Laboratory Fiber-Plus, Monkey Diet 5049, LabDiet, St Louis, MO, USA) throughout gestation, whereas nutrient-restricted animals were fed at 65% of control intake from gestational day 32 to 70, and 70% of control intake from gestational day 71 to the end of gestation (term gestation for this species under laboratory conditions is 154–170). Pregnancy was monitored by monthly ultrasound scans, and natural delivery attained for all births without human intervention.
5-Aza-2′-dC treatment of UC-MSCs
MSCs (passage 3) were grown in T75 flasks until confluence and subsequently split into 5 cm dishes. Then, 1 μl of 10 mM 5-aza-2′-deoxycytidine (5-aza-dC) stock in dimethyl sulfoxide was added to 2 ml of MSC medium everyday for 5 days to the treatment group. An equivalent volume of dimethyl sulfoxide was added to the control. At the end of 5 days, cells were harvested in TRIzol (Life Technologies, Carlsbad, CA, USA) for RNA extraction. Cell pellets were washed and frozen for DNA extraction.
RNA extraction
RNA extraction for human and NHP umbilical cords was similarly performed. Briefly, cord tissue was crushed in liquid nitrogen using a mortar and pestle. Crushed cord tissue was transferred to a sterile gentleMACS tube containing TRIzol reagent, and homogenized on the gentleMACS Dissociator (both, Miltenyi Biotech GmBH, Bergisch Gladbach, Germany). After centrifugation to remove cell debris, the supernatant was transferred to a clean tube, and 200 μl chloroform was added per 1 ml of TRIzol used. Samples were vortexed, then centrifuged and the aqueous phase transferred to a new tube. For human samples, an equal volume of isopropanol was added, and RNA left to precipitate overnight at −20 °C. The RNA pellet was retrieved by centrifugation, and washed twice in 70% ethanol, air-dried, and resuspended in 30 μl of RNAse-free water. For NHP samples, an equal volume of 70% ethanol was added to the aqueous phase, mixed gently and applied to an RNeasy mini column (Qiagen, Hilden, Germany). Wash steps were applied according to the manufacturer’s recommendation, an on-column DNAse removal step included and RNA was eluted in RNAse-free water. RNA from UC-MSC lines was prepared using a Qiagen RNEasy kit, according to the manufacturer’s instructions. In all samples, RNA integrity and concentration was determined using the Agilent 2100 Bioanalyzer RNA 6000 Nano Labchip (Agilent Technologies, Waldbronn, Germany), and RNA purity using a Nanodrop ND-8000 spectrophotometer (Thermo Fisher Scientific, Wilmington, DE, USA).
Quantitative PCR
Complementary DNA was prepared from total RNA, with MuLV-Reverse Transcriptase contained in the High Capacity cDNA Reverse Transcription Kit (Life Technologies). Quantitative PCR reactions were prepared in triplicate using Power SYBR Green Master Mix (Life Technologies) in a final reaction volume of 10 μl. Samples were run on an ABI7900 HT Sequence Detection System (Life Technologies), and primers were previously validated for similar primer efficiencies. Fold change was quantified using the relative Ct method, and group differences verified with Student’s t-test. Primer sequences are as follows:
Human sequences: CXCL14-F: 5′-GCACCAAGCGCTTCATCAA-3′ and CXCL14-R: 5′-TCGTAGACCCTGCGCTTCTC-3′; GAPDH-F: 5′-GGTGTGAACCATGAGAAGTATGACA-3′ and GAPDH-R: 5′-GGTGCAGGAGGCATTGCT-3′; ACTB-F: 5′-CGAGGCCCCCCTGAAC-3′ and ACTB-R: 5′-GTCTCAAACATGATCTGGGTCATC-3′.
M. fascicularis sequences: CXCL14-F: 5′-GTCAGCATGAGGCTCCTG-3′ and CXCL14-R: 5′-GTACTTTGGCTTCATTTCCAG-3′; ACTB-F: 5′-CTGACTACCTCATGAAGATCCTC-3′ and ACTB-R: 5′-TGTTGGCGTACAGGTCTTTAC-3′; GAPD-F: 5′-GTGAAGGTCGGAGTCAACG-3′ and GAPD-R: 5′-ATGGGTGGAATCATACTGGAAC-3′; RPL32-F: 5′-TCAAGGAGTTGGAAGTGCTG-3′ and RPL32-R: 5′-GGGTTGGTGACTCTGATGG-3′.
DNA extraction
DNA extraction for human and NHP umbilical cords was similarly performed. Briefly, cord tissue was crushed in liquid nitrogen using a mortar and pestle. Crushed cord tissue was transferred to a sterile gentleMACS tube containing 10 U ml−1 hyaluronidase in 1 × phosphate-buffered saline (Type 1S-hyaluronidase, Cat. no. H4506, Sigma Aldrich, St Louis, MO, USA) and incubated for 30 min at 37 °C with gentle shaking. Thereafter, an equal volume of TNES solution (50 mM Tris pH 7.5, 400 mM NaCl, 100 mM EDTA, 0.5% SDS) was added and homogenized on the gentleMACS dissociator (Miltenyi Biotech GmBH). Proteinase K to a final concentration of 0.1 mg ml−1 was added (Roche Holdings AG, Basel, Switzerland), and the sample incubated overnight at 55 °C. High-quality genomic DNA was precipitated with ethanol, and an additional phenol/chloroform step included, before the pelleted DNA was washed with 70% ethanol and resuspended in water. DNA was quantified using Quant-it Picogreen reagent (Life Technologies), purity assessed with a Nanodrop spectrophotometer, and integrity assessed by conventional gel electrophoresis.
Pyrosequencing analysis
Bisulfite conversion of genomic DNA was prepared using a EpiTect Bisulfite Kit (Qiagen) according to the manufacturer’s recommendations. Briefly, 500 ng of input genomic DNA was eluted in 20 μl, and 1 μl subsequently used in a PCR reaction for downstream pyrosequencing analysis, and included a biotinylated primer for capture of PCR products to the sepharose beads. PCR products were checked for a specific single band, and pyrosequencing was performed on a PyroMark Q24 machine (Qiagen) using 10–15 μl of PCR product in a standard reaction volume. Primer sequences are available on request.
Molecular cloning and transfection
A fragment of the CXCL14 promoter was amplified by PCR with primers containing flanking restriction sites for cloning into the pCpG-free vector (Cat. no. PCPGF-PROM, InvivoGen, San Diego, CA, USA) containing a human EF-1alpha promoter and a secreted CpG free allele of the murine embryonic alkaline phosphatase (mSEAP) reporter, genomic position of CXCL14 fragment: hg19, chr5(−): 134914698–134914809, 112 bp. This plasmid was subjected to site-directed mutagenesis using the QuikChange Multi Site-Directed Mutagenesis Kit (Agilent Genomics, Santa Clara, CA, USA) at specific CpGs of interest, as indicated in Figure 5a. Thereafter, the verified plasmids were transformed into GT115 Escherichia Coli-competent cells (InvivoGen), and purified plasmids obtained using the Qiagen Plasmid Midiprep Kit (Qiagen). Methylation of the plasmids was carried out by treating the plasmids with CpG methyltransferase, M.SssI (New England Biolabs, Ipswich, MA, USA) as per the manufacturer’s instructions.
HEK-293T cells were seeded at a density of 8 × 104 cells in each well of a 24-well plate in Dulbecco’s modified Eagle’s medium with 10% heat-inactivated fetal bovine serum. The cells were transfected the next day with 500 ng of pCpG-free plasmids (InvivoGen) per well for 48 h using Lipofectamine LTX (Invitrogen, Carlsbad, CA, USA). Transfection was performed according to the manufacturer’s instructions. After 48 h, 20 μl of supernatant from each well was used for detection and quantification of secreted embryonic alkaline phosphatase (mSEAP) activity using QUANTI-Blue (Cat. no. REP-QB1, InvivoGen), performed as per the manufacturer’s instructions.
MSCs were similarly transfected using Lipofectamine LTX (Invitrogen), but with an initial seeding density of 50 × 104 cells in a single well of a 12-well plate containing Dulbecco’s modified Eagle’s medium/10% heat inactivated fetal bovine serum. MSCs were transfected the next day with 1 μg of pCpG-free plasmids. After 96 h, 50 μl of supernatant from each well was used for quantification of secreted mSEAP activity using QUANTI-Blue.
Results
Elevated CXCL14 levels are observed in umbilical cord and cord-derived cells from low birth weight/SGA infants
The transcript abundance of CXCL14 was first measured in umbilical cords from infants with low and normal birth weights using quantitative PCR. Subjects selected were matched for maternal age, maternal body mass index and gender, and were of single ethnicity (Chinese, Table 1). In this study, we found that the relative levels of CXCL14 transcript were significantly elevated in infants belonging to the LBW category (birth weight <2500 g), although the fold change differences in the LBW infants varied across a wider spectrum than in normal birth weight infants. We also compared CXCL14 expression with additional newborn growth parameters, and found that elevated levels of CXCL14 were indeed associated with overall reduced growth, as measured by smaller head, abdominal and mid-arm circumference, as well as reduced body fat at birth (triceps and subscapular skinfold thickness). Particularly, increased CXCL14 levels were most significantly correlated with abdominal circumference, a proxy measure for central adiposity (Supplementary Figures 1A–E).
To consider whether the heterogeneity of umbilical cord tissue used might be a contributing factor, we also assessed CXCL14 expression levels in MSCs derived from the Wharton’s jelly of umbilical cords derived from normal and SGA infants (see Materials and methods). In both the LBW and SGA groups, an increase in CXCL14 expression was observed, with a median fold increase of approximately threefold in whole umbilical cords (Figure 1a) as well as UC-MSCs (Figure 1b).
CXCL14 levels are elevated in low birth weight infants. (a) RNA was extracted from whole umbilical cord tissue, and CXCL14 expression measured by quantitative PCR (qPCR). Each sample was measured in triplicate. Normal birth weight (BW)=48, low BW=12, P=0.00024. (b) CXCL14 expression was compared between umbilical cord-derived mesenchymal stem cell (UC-MSC) lines derived from normal and small-for-gestational-age infants (SGA, 5th—10th %tile for birth weight). Normal UC-MSCs=3, SGA UC-MSCs=3, Student’s t-test P=0.08.
Higher CXCL14 levels in NHPs with SGA background
To ascertain whether the changes in CXCL14 levels observed in human umbilical cord and UC-MSCs of LBW/SGA infants were robust, we also looked at CXCL14 levels in umbilical cords obtained from NHPs M. fascicularis that are commonly used to understand aspects of primate metabolic disease and reproduction.12 Normal dams were placed on global caloric restriction from day 35 of gestation to induce intrauterine growth restriction (IUGR) in the offspring, who had marginally reduced birth weights from control offspring (results not published). Umbilical cord levels of CXCL14 were measured between the induced SGA/IUGR and control offspring, with a clear indication that growth-restricted Macaca infants too had significantly elevated CXCL14 levels (Figure 2) to similar extents observed in human samples (Figure 1). Similar to what we observed in humans, CXCL14 expression levels in the Macaca neonates were also negatively correlated with reduced abdominal circumference at birth (Supplementary Figure 1F).
Elevated CXCL14 expression in non-human primates with intrauterine growth retardation (IUGR). CXCL14 levels were assessed from whole umbilical cords of Cynomolgus macaques (Macaca fascicularis) of normal or small-for-gestational-age (SGA)/IUGR background. In this model, growth restriction in offspring was induced by global maternal undernutrition from gestational day 35 to birth. Normal=11, IUGR=5, Student’s t-test P=0.024.
5-Aza-dC treatment of UC-MSCs induces elevated CXCL14 expression
In the context of tumorigenesis, depressed CXCL14 expression has been observed,13 and was attributed to epigenetic silencing, as the addition of the demethylating agent 5-aza-dC was shown to reactivate CXCL14 levels with a subsequent increase in CXCL14 chemoattractant activity.14 This was accompanied by the identification of promoter-bound CpGs that are hypermethylated in cancer cells.
We sought to see whether CXCL14 expression was also regulated by DNA methylation in our UC-MSC system. For this purpose, we treated two normal MSC lines with 5-aza-dC. As measured by quantitative PCR, CXCL14 expression was enhanced following the treatment, suggesting that DNA methylation is indeed implicated in the regulation of CXCL14 expression in cord-derived MSCs (Figure 3).
DNA methylation is involved in the regulation of CXCL14 expression. CXCL14 expression is increased in mesenchymal stem cells (MSCs) upon treatment with 5-aza-deoxycytidine (5-aza-dC). Results from each independently derived normal umbilical cord-derived MSC (UC-MSC) line show concordance in the direction and extent of change on 5-aza-dC treatment. Technical replicates/cell line=2, Student’s t-test P=0.06 (MSC line 1) and P<0.05 (MSC line 2).
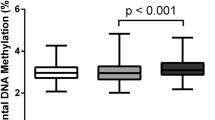
Decreased CXCL14 methylation within the promoter region in LBW individuals
In order to determine the DNA methylation status of the CXCL14 gene, we assessed selected CpG sites, including regions in the promoter, where methylation changes were previously reported,14 as well as in the gene body and the 3′-untranslated region. Intriguingly, at 5 of the 30 CpG sites analyzed (Figures 4a and b, CpG sites A–E), DNA methylation levels were significantly decreased in umbilical cords from LBW individuals. These five CpGs correspond primarily to locations within the 5′-untranslated region and the predicted bidirectional promoter located in an intragenic position ∼7 kb downstream of the canonical CXCL14 5′-untranslated region (Figure 4, specific positions shown in Figure 4a, CpGs D and E). Two of these five CpGs are proximal to an AP1 binding site within the promoter region (Figure 4a, CpGs B and C). AP1 binding at this site has previously been shown to affect CXCL14 expression levels,15 and includes a CpG site within the AP1 binding sequence itself (Figure 4a, CpG F). As such, we sought to see whether changes in DNA methylation at the two noncontiguous CpGs immediately downstream of the AP1 site were also reflected at the CpG site within the AP1 site, and whether DNA methylation variations in the LBW group might be associated with AP1 binding in order to regulate CXCL14 levels. We found that the CpG within the AP1 site showed no significant difference in methylation levels between normal and low birth weight subjects (Figure 4b, CpG F).
CpG methylation assessed across CXCL14 identifies variable methylation sites in human umbilical cords. (a) Map of CXCL14 locus with CpGs A–F shown in genomic context (CpGs A–F: filled diamonds). Also, 25 additional CpGs were analyzed in human umbilical cords of normal and low birth weight (BW) backgrounds, all by bisulfite pyrosequencing (relative positions shown as open diamonds). Five CpGs (A–E) differed between birth weight groups. CpG A is located close to a repetitive sequence slightly upstream of the CXCL14 5′-untranslated region (5′-UTR). CpGs B and C are located within the 5′−UTR next to an activator protein 1 (AP1) binding site; CpGs D and E, located at the 5′ end of a predicted bidirectional promoter that has its origins in the 3′−UTR of the CXCL14 reference sequence (*). CpG F is located within the reported AP1 site (TGAGTCACCG), the underline indicates the CG site (CpG-F) within the AP1 binding site, and in the vicinity of CpGs B and C. The organization of these CpG sites is more clearly seen in the expanded region shown, the coordinates given are for this expanded region that is also the region used in the reporter constructs shown in Figure 5. (b) CpG methylation at each of the five CpGs (A–E) described in (a) show a trend of decreased methylation in the low birth weight (LBW) group. Normal BW=12, low BW=7, Student’s t-test P-values as shown in individual panels. Genomic coordinates for each of the six CpGs are shown.
Mutagenesis of key CpGs within the CXCL14 promoter alters reporter expression
To verify that specific CpG methylation changes at two sites downstream of the CXCL14 AP1 binding site contribute directly to changes in CXCL14 expression, we utilized a reporter assay containing the CXCL14 region of interest spliced directly upstream of the EF-1alpha promoter and SEAP reporter gene in a CpG-free plasmid. Site-directed mutagenesis of the included CXCL14 region altered the AP1 proximal CpG or either of the two downstream CpGs to a non-CpG site, rendering each individual site no longer susceptible to methylation after the plasmid was treated with CpG methyltransferase M.SssI (Figure 5a).
Transient transfection of mutated CXCL14 promoter identifies two CpGs involved in regulating gene expression. (a) Summary of site-directed mutagenesis performed on a set of reporter plasmids containing a CXCL14 promoter fragment that includes the activator protein 1 (AP1) binding site and CpGs B and C. In each plasmid variant, individual CpG sites were mutated to remove the possibility of methylation when M.SssI was used. Reporter activity of the unmethylated and M.SssI-treated methylated plasmids was compared to determine the significance of each of the three CpGs in the region toward CXCL14 activity. (b) Transient transfection of CXCL14 in HEK293T cells. Reporter activity was normalized to empty vector controls for both methylated and unmethylated plasmid variants. Three replicates were performed for each transfection. Student’s t-test, *P<0.05, **P<0.001; n.s., not significant.
The in vitro methylated and unmethylated reporter plasmids were transfected into HEK293T cells and compared with empty vector controls. On methylation of the wild-type CXCL14 insert, expression of the reporter decreased by threefold (Figure 5b), in concordance with a typical role for suppressive methylation in the promoter region. Alteration of the AP1 binding site at a non-CpG location resulted in decreased expression to a level similar to that of the methylated wild-type construct, and methylation of the construct further reduced expression. The AP1 binding site of CXCL14 includes a CpG at the end. To consider whether methylation of this CpG might affect expression, we compared reporter expression of a mutated AP1-CpG to that of a mutated AP1 non-CpG vector. Expression levels were similar when both vectors were compared, either when unmethylated or after methylation in vitro. This suggests that loss of AP1 binding, and not methylation changes within the AP1 site, is the primary driver in suppressing CXCL14 expression. We earlier compared group-wise differences in methylation at the AP1-CpG (Figure 4, CpG F), and also did not find any significant differences in AP1-CpG methylation between normal and low birth weight individuals. We next compared constructs where either of the two CpGs (Figure 4, CpGs B and C) immediately downstream of the AP1 site were altered. Reporter levels were similar between the two CpG sites, suggesting that they may work cooperatively or also function as part of a larger binding site for an unknown factor. When compared with the wild-type construct, the unmethylated constructs showed a significant, although ∼12% increase in reporter expression. More notably, expression of the methylated constructs showed that reporter expression was no longer suppressed to a level found for the methylated wild-type construct, and enforced loss of methylation through site-directed mutagenesis at either of these two CpG sites resulted in reporter expression at levels approximately twofold higher than in the wild type. This suggests that methylation at either of the two CpG sites is mechanistically involved in the regulation of CXCL14 expression at the promoter. In line with this, we discovered that expression of CXCL14 is elevated in LBW individuals, with associated decrease in methylation at both CpGs B and C.
To ascertain whether this reporter activity might be cell-type specific, we also transfected an umbilical cord-derived MSC line with the same constructs, and had largely correspondent findings (Supplementary Figure 2). In UC-MSCs, AP1 binding is still required, and mutation of the binding site at the core or AP1-CpG both result in decreased reporter activity. Although CpGs B and C show similar trends, it is less clear whether there is coordinate activity between the two CpG sites, given that the extent of unmethylated reporter activity differs. In addition, reporter expression of methylated constructs for CpGs B and C show very subtle increases relative to the wild-type equivalent, and may suggest that additional CpG sites, such as those shown in Figure 4b, are implicated in regulating CXCL14 in this cell type.
Discussion
Using a variety of approaches, our data support an epigenetic mechanism playing a role in the regulation of CXCL14, a gene that encodes a chemokine known to function in monocytes and dendritic cell attraction,16, 17 that may also play a role in insulin regulation and obesity.18 Epidemiological surveys of metabolic dysfunction in adult humans suggest multiple risk factors such as suboptimal fetal nutrition enforcing adaptive response mechanisms leading to SGA neonates.19, 20, 21 Birth weight has often been used as a proxy for the quality of nutritional intake during the fetal period and an adversely low birth weight has typically been associated with a propensity for early catch-up growth and greater abdominal fat mass and elevated risk for subsequent metabolic disease.22, 23 In light of published studies on Cxcl14−/− mice that are resistant to the adverse effects of a high-fat diet,18 we surmised that changes to CXCL14 levels might be anticipated within a normal human population, as well as in a defined model of nutritionally induced growth restriction in NHPs.
In this study, we examined umbilical cords from human infants, and first found upregulated expression of CXCL14 in LBW individuals. This agrees with rodent data on Cxcl14 suggesting a role for this chemokine in weight gain, although particularly in female rodents over males. No such gender association for CXCL14 expression levels was found in our human umbilical cord data, but this would be better considered over a larger cohort analysis. Separately, it may be that this gender association is not conserved between the species. In our human umbilical cord data (Figure 1a), the difference in CXCL14 expression levels between low and normal birth weight groups is robust, but shows a larger range of variation in the LBW group. As additional factors besides birth weight would improve the discrimination between metabolic potentials of the individuals surveyed, we also considered other typical neonate anthropometric measures, and found that higher CXCL14 expression levels were indicative of generally smaller infants with lesser adiposity at birth. This may warrant additional consideration for employing CXCL14 expression levels as an indicator of an individual’s likely metabolic trajectory.
Human umbilical cords are one of the few birth tissues available for routine analysis, and present a snapshot of the gestational health of an infant. However, considering the complexity of multiple cell types in cord might also contribute to the variation seen in CXCL14 levels, we also analyzed UC-MSCs that originate from the cord’s Wharton’s jelly component.24 These multipotent cells potentially contribute to adipocyte and muscle cell lineages, and may provide a more direct comparison of CXCL14 levels in a single cell line that is relevant to known CXCL14 function in obesity-related insulin signaling. Reliably, we also obtained a similar mean (approximately threefold) level of CXCL14 increase in UC-MSCs from SGA infants (Figure 1b). This suggests that UC-MSCs may be successfully used to represent umbilical cords, with the added advantage of in vitro manipulation.
Because LBW/SGA designations have been used as proxy parameters, and are possible outcomes, but not causal for true intrauterine growth retardation, we proceeded to analyze umbilical cord specimens obtained from Cynomolgus macaques. The macaques were subjected to controlled nutritional restriction from early gestation onwards so as to develop IUGR in the offspring (Chng K et al, manuscript in preparation). We found a significantly increased level of CXCL14 in the SGA/IUGR offspring, despite the small number of samples inherent in an experimental primate study. Given the subtle phenotypic differences between the SGA/IUGR and normal offspring at birth (data not published), it is of note that early differences in CXCL14 levels are already recognizable at this stage.
Epigenetic mechanisms have a role in developmental plasticity25 and might also be at work in the regulation of CXCL14. To test this hypothesis, normal UC-MSCs were subjected to treatment with 5-aza-dC, a global nonspecific inhibitor of DNA methylation.26 Upon treatment, the UC-MSCs showed increased levels of CXCL14, suggesting that CXCL14 is an epigenetically regulated gene and that loss of DNA methylation may contribute to the increased CXCL14 expression observed in the umbilical cord specimens examined. Although multiple CpGs may be involved in DNA methylation-based control of the locus, we analyzed 30 sites across CXCL14, selected to represent CpGs proximal to the promoter, or other landmarks such as insulator binding sites, repetitive sequences and predicted alternative promoter sites. From this, five sites were found to significantly differ between low and normal birth weight groups. Interestingly, these sites all showed the same directionality of methylation change, with a decrease seen in LBW individuals. This may be coincidental, or otherwise represent a larger change in the methylation landscape across CXCL14 that increases the permittivity of chromatin, although in a more subtle manner than at a single site alone. Given the proximity of these CpG sites in cis, further analysis may consider whether these CpG sites work cooperatively, and perhaps show complementary looping that create novel enhancer binding sites.
AP1 binding was previously shown to increase CXCL14 expression.15 Of the 5 CpGs analyzed, 2 are located within 20 bp downstream of the published AP1 binding site. We investigated whether CpG methylation within the AP1 binding site was altered between birth weight groups, but we did not find a significant difference. This was supported by our reporter gene studies, where reporter activity was reduced similarly on mutagenesis of the AP1 binding site, regardless of whether the mutation was placed at the site core or on the CpG at the tail end of the binding site. At the mutated downstream CpG sites, reporter activity was increased over the controls when these sites could no longer be in vitro methylated, suggesting that DNA methylation at these specific sites were implicated in the regulation of the downstream promoter. These two CpG sites produced similar results in our reporter assay, and are likely part of the same functional region. In similar transfections of these constructs performed in an UC-MSC line, we note that the results recapitulate the major trends seen in HEK-293T cells, with differences potentially attributable to the presence of additional transcriptional regulatory mechanisms that may be more active in a multipotent cell line.
In conclusion, we have shown that CXCL14 expression levels are increased in specimens typically associated with a higher risk of developing metabolic disease. This is seen in both human and human-derived samples, and confirmed in a defined SGA/IUGR model using NHPs. The impaired fetal environment results in changes to CXCL14, and these may persist through time via epigenetic mechanisms. We have shown that DNA methylation is one such mechanism, although it is likely that additional epigenetic and transcriptional controls are at work, and further studies to probe for changes in histone modifications are pending. Our findings suggest that epigenetic regulation of CXCL14 expression has a developmental influence on pathways to insulin resistance and suggests approaches to both physiological and interventional studies.
References
Barouki, R., Gluckman, P. D., Grandjean, P., Hanson, M. & Heindel, J. J. Developmental origins of non-communicable disease: implications for research and public health. Environ. Health. 11, 42 (2012).
Hanson, M. A. & Gluckman, P. D. Developmental origins of health and disease: moving from biological concepts to interventions and policy. Int. J. Gynaecol. Obstet. 115, Suppl 1, S3–S5 (2011).
Godfrey, K. M., Sheppard, A., Gluckman, P. D., Lillycrop, K. A., Burdge, G. C., McLean, C. et al. Epigenetic gene promoter methylation at birth is associated with child's later adiposity. Diabetes 5, 1528–1534 (2011).
Soh, S. E., Tint, M. T., Gluckman, P. D., Godfrey, K. M., Rifkin-Graboi, A., Chan, Y. H. et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. Int. J. Epidemiol. (e-pub ahead of print 2 August 2013; doi:10.1093/ije/dyt125).
Stünkel, W., Pan, H., Chew, S. B., Tng, E., Tan, J. H., Chen, L. et al. Transcriptome changes affecting Hedgehog and cytokine signalling in the umbilical cord: implications for disease risk. PLoS ONE 7, e39744 (2012).
Hara, T. & Tanegashima, K. Pleiotropic functions of the CXC-type chemokine CXCL14 in mammals. J. Biochem. 151, 469–476 (2012).
Hara, T. & Nakayama, Y. CXCL14 and insulin action. Vitam. Horm. 80, 107–23 (2009).
Takahashi, M., Takahashi, Y., Takahashi, K., Zolotaryov, F. N., Hong, K. S., Iida, K. et al. CXCL14 enhances insulin-dependent glucose uptake in adipocytes and is related to high-fat diet-induced obesity. Biochem. Biophys. Res. Commun. 364, 1037–1042 (2007).
Nara, N., Nakayama, Y., Okamoto, S., Tamura, H., Kiyono, M., Muraoka, M. et al. Disruption of CXC motif chemokine ligand-14 in mice ameliorates obesity-induced insulin resistance. J. Biol. Chem. 282, 30794–30803 (2007).
Fong, C. Y., Subramanian, A., Biswas, A., Gauthaman, K., Srikanth, P., Hande, M. P. et al. Derivation efficiency, cell proliferation, freeze-thaw survival, stem-cell properties and differentiation of human Wharton’s jelly stem cells. Reprod. Biomed. 21, 391–401 (2010).
Sukarieh, R., Joseph, R., Leow, S. C., L, Y., Löffler, M., Aris, I. A. et alMolecular pathways reflecting poor intrauterine growth are found in Wharton’s jelly derived mesenchymal stem cells. Hum. Reprod. (in press).
Bauer, S. A., Arndt, T. P., Leslie, K. E., Pearl, D. L. & Turner, P. V. Obesity in rhesus and cynomolgus macaques: a comparative review of the condition and its implications for research. Comp. Med. 61, 514–526 (2011).
Tessema, M., Klinge, D. M., Yingling, C. M., Do, K., Van Neste, L. & Belinsky, S. A. Re-expression of CXCL14, a common target for epigenetic silencing in lung cancer, induces tumor necrosis. Oncogene 29, 5159–5170 (2010).
Song, E. Y., Shurin, M. R., Tourkova, I. L., Gutkin, D. W. & Shurin, G. V. Epigenetic mechanisms of promigratory chemokine CXCL14 regulation in human prostate cancer cells. Cancer Res. 70, 4394–4401 (2010).
Komori, R. 1, Ozawa, S., Kato, Y., Shinji, H., Kimoto, S. & Hata, R. Functional characterization of proximal promoter of gene for human BRAK/CXCL14, a tumor-suppressing chemokine. Biomed. Res. 31, 123–131 (2010).
Kurth, I., Willimann, K., Schaerli, P., Hunzike, T., Clark-Lewis, I. & Moser, B. Monocyte selectivity and tissue localization suggests a role for breast and kidney-expressed chemokine (BRAK) in macrophage development. J. Exp. Med. 194, 855–861 (2001).
Schaerli, P., Willimann, K., Ebert, L. M., Walz, A. & Moser, B. Cutaneous CXCL14 targets blood precursors to epidermal niches for Langerhans cell differentiation. Immunity 23, 331–342 (2005).
Tanegashima, K., Okamoto, S., Nakayama, Y., Taya, C., Shitara, H., Ishii, R. et al. CXCL14 deficiency in mice attenuates obesity and inhibits feeding behavior in a novel environment. PLoS One 5 (2010).
Gluckman, P. D. & Hanson, M. A. Maternal constraint of fetal growth and its consequences. Semin. Fetal Neonatal Med. 9, 419–425 (2004).
Gluckman, P. D. & Hanson, M. A. The consequences of being born small - an adaptive perspective. Horm. Res. 65 (Suppl 3), 5–14 (2006).
Kerkhof, G. F. & Hokken-Koelega, A. C. Rate of neonatal weight gain and effects on adult metabolic health. Nat. Rev. Endocrinol. 8, 689–692 (2012).
Meas, T., Deghmoun, S., Armoogum, P., Alberti, C. & Levy-Marchal, C. Consequences of being born small for gestational age on body composition: an 8-year follow-up study. J. Clin. Endocrinol. Metab. 93, 3804–3809 (2008).
Barker, D. J., Gluckman, P. D., Godfrey, K. M., Harding, J. E., Owens, J. A. & Robinson, J. S. Fetal nutrition and cardiovascular disease in adult life. Lancet 341, 938–941 (1993).
Batsali, A. K., Kastrinaki, M. C., Papadaki, H. A. & Pontikoglou, C. Mesenchymal stem cells derived from Wharton’s Jelly of the umbilical cord: biological properties and emerging clinical applications. Curr. Stem Cell Res. Ther. 8, 144–155 (2013).
Gluckman, P. D., Hanson, M. A. & Low, F. M. The role of developmental plasticity and epigenetics in human health. Birth Defects Res. C Embryo Today 93, 12–18 (2011).
Singh, V., Sharma, P. & Capalash, N. DNA methyltransferase-1 inhibitors as epigenetic therapy for cancer. Curr. Cancer Drug Targets. 13, 379–399 (2013).
Acknowledgements
We are grateful for the expert technical assistance of Rachel Chew, Tan Li Hua and Yhee Cheng Chng. We thank Professor Kenneth Kwek and the GUSTO study group for enabling the collection of umbilical cord tissue. This work is supported by the Translational Clinical Research (TCR) Flagship Program on Developmental Pathways to Metabolic Disease funded by the National Research Foundation (NRF) and administered by the National Medical Research Council (NMRC), Singapore (NMRC/TCR/004-NUS/2008). SICS Investigators are supported through Agency for Science Technology and Research (A*STAR) funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Rights and permissions
About this article
Cite this article
Cheong, C., Chng, K., Lim, M. et al. Alterations to DNA methylation and expression of CXCL14 are associated with suboptimal birth outcomes. J Hum Genet 59, 504–511 (2014). https://doi.org/10.1038/jhg.2014.63
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.63
This article is cited by
-
Transcriptome analysis of adenomyosis eutopic endometrium reveals molecular mechanisms involved in adenomyosis-related implantation failure and pregnancy disorders
Reproductive Biology and Endocrinology (2024)