Abstract
Bardet–Biedl syndrome (BBS) is a rare ciliopathy disorder that is clinically and genetically heterogeneous with 18 known genes. This study was performed to characterize responsible genes and mutation spectrum in a cohort of 14 Iranian families with BBS. Sanger sequencing of the most commonly mutated genes (BBS1, BBS2 and BBS10) accounting for ∼50% of BBS patients determined mutations only in BBS2, including three novel mutations. Next, three of the remaining patients were subjected to whole exome sequencing with 96% at 20 × depth of coverage that revealed novel BBS4 mutation. Observation of no mutation in the other patients represents the possible presence of novel genes. Screening of the remaining patients for six other genes (BBS3, BBS4, BBS6, BBS7, BBS9 and BBS12) revealed five novel mutations. This result represents another indication for the genetic heterogeneity of BBS and extends the mutational spectrum of the disease by introducing nine novel mutations in five BBS genes. In conclusion, although BBS1 and BBS10 are among the most commonly mutated genes in other populations like Caucasian, these two seem not to have an important role in Iranian patients. This suggests that a different strategy in molecular genetics diagnostic approaches in Middle Eastern countries such as Iran should be considered.
Similar content being viewed by others
Introduction
Bardet–Biedl syndrome (BBS, MIM no. 209900) is a rare genetic ciliopathy disorder in which different body systems are affected with a wide range of clinical symptoms. The clinical signs are divided into two categories: primary and secondary features. Primary features, hallmarks of the disorder, are the most prevalent signs, including rod–cone dystrophy leading to night blindness and eventually considerable blindness, polydactyly, obesity, hypogonadism, renal anomalies and mental retardation.1, 2 However, considering mental retardation as one of the cardinal features has been challenged.1, 3, 4 Secondary or minor features include speech disorder, diabetes mellitus, hearing loss, liver disease, Hirschprung disease, congenital heart defects, craniofacial abnormalities and many others. Owing to the observation of pleiotropy in BBS, clinical diagnosis is based on the presence of at least four primary features or three primary plus at least two secondary features.5, 6
The prevalence of this disorder is variable from approximately 1 in 125 000–160 000 in North America and Europe7, 8, 9 and 1 in 156 000 in Tunisia of North Africa10 to higher prevalence such as 1 in 17 000 among the Bedouins in Kuwait,11 1 in 13 000 in Newfoundland12 and 1 patient in every 3700 individual in The Faroe Islands,7, 13 suggesting the role of founder effect in these specific populations.
Classically, autosomal recessive pattern of inheritance has been considered for this disorder. However, regarding the variable penetrance and expressivity of the clinical symptoms observed in the patients, a more complex and also controversial pattern named ‘triallelic inheritance’ or ‘digenic trait’ has been proposed in <10% of the BBS families.14, 15
BBS is a heterogeneous ciliopathy disorder, with 18 known genes that account for about 80% of the cases. These include BBS1, BBS2, BBS3 (ARL6), BBS4, BBS5, BBS6 (MKKS), BBS7, BBS8 (TTC8), BBS9 (PTHB1), BBS10, BBS11 (TRIM32), BBS12, BBS13 (MKS1), BBS14 (CEP290), BBS15 (C2orf86), BBS16 (SDCCAG8), BBS17 (LZTFL1) and BBS18 (BBIP1).7, 14, 16, 17
Variations in the contribution of each gene in different reports, in addition to the presence of some clinically diagnosed BBS patients with no responsible mutations in the known genes, all together offers the possibility of other novel genes (the remaining 20%), not being identified yet. Now, it is clear that all these genes have a specific role in the ciliogenesis and maintenance of the cilium, mostly by forming BBSome complex (BBS1, BBS2, BBS4, BBS5, BBS7, BBS8 and BBS9) or being a part of chaperonin complex (BBS6, BBS10 and BBS12). BBS7 protein interacts with BBS2 and BBS9 proteins to form the BBSome core complex, which is an important intermediate complex during the sequential assembly of BBSome. These assembly reactions are stabilized and regulated by BBS chaperonic complex (BBS6, BBS12, BBS10 and CCT/TRiC). BBS3 (ARL6) is one of the GTP-binding proteins with an essential role in proper localization of BBSome. However, other genes are located in or at the distal end of basal bodies interacting with different signaling pathways; such as, sonic hedgehog and Wnt.1, 2, 6, 14, 18, 19 The recently identified genes BBS17 (LZTFL1) and BBS18 (BBIP1) have been presented with roles in BBSome entry into cilia for BBS17 and being the eighth subunit of the BBSome for BBS18, respectively.16, 17
All the 18 known genes in BBS account for about 80% of the clinically diagnosed cases. BBS1 and BBS10 are the most frequently mutated genes that account for about 23% and 20% of BBS patients in European and North American populations, respectively. However, some regional variations have been reported as patients originating from Middle East and North Africa are mostly mutated in BBS4, BBS5 and BBS8,14 and BBS4 is reported as the most prevalent gene among Turks and Pakistanis. There are several reports in Pakistani families with mutations in BBS1, BBS3, BBS10 and BBS12.7, 20, 21, 22 Owing to the high heterogeneity in BBS, a practical approach is needed for molecular diagnosis, which cannot be achieved unless prioritization based on the prevalence of pathogenic mutations.
The spectrum of BBS gene mutations in Middle Eastern countries, especially Iran, is not entirely clear, which indicates that more study is needed to determine a strategy for molecular diagnosis of this syndrome in populations. This study was performed to characterize responsible genes and mutation spectrum in a cohort of 14 Iranian families with BBS.
Materials and methods
Recruitment of the subjects and clinical diagnosis
Clinical examination was performed considering the presence of at least four cardinal signs or three primary features with expressing at least two minor symptoms as the inclusion criteria for BBS diagnosis.
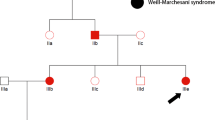
Fourteen unrelated patients with BBS, 13 of which were of various ethnic origins within Iran and 1 immigrant from Afghanistan were recruited in this study. In 7 out of 14 (50%) referred families, there were only one affected child, but the remaining families had more children (2 and 3) with BBS phenotype. Consanguinity was absent in two families (Table 1). Informed consent from all patients was obtained, according to the ethics committee recommendations. The genomic DNA of the patients was extracted from their blood’s white blood cells as described elsewhere.23 RNA extraction and establishment of Epstein–Barr virus-transformed lymphoblastoid cell lines were performed whenever it was required.24
Mutation analysis
Initial screening for the three most commonly mutated genes
Initially, mutation analysis of all the 14 patients was performed by screening the coding regions of the three most commonly mutated genes, including BBS1, BBS2 and BBS10. Primer3 (http://frodo.wi.mit.edu/primer3/) and Oligoanalyzer 3.1 (http://eu.idtdna.com/analyzer/applications/oligoanalyzer/) were used for designing 41 primer sets to cover all 36 coding exons of the three genes plus 50 bp from introns in the both sides of each exon.25 Conventional Sanger sequencing using Big Dye Terminators (Applied Biosystems 3130 Genetic Analyzer; Applied Biosystems, Foster City, CA, USA) was used for sequencing the amplified DNA amplicons. Mutation nomenclature was made according to the guidelines of Human Genome Variation Society (HGVS v.2.0) and checked with the use of Mutalyzer (https://mutalyzer.nl/). Functional effect of the novel missense mutations were evaluated using bioinformatics tools such as PolyPhen (http://genetics.bwh.harvard.edu/pph2/), SIFT (http://sift.jcvi.org/) and Conseq server (http://conseq.tau.ac.il/) if possible and also cosegregation analysis in the families.26, 27, 28
Exome sequencing
Next, three of the remaining patients were chosen and whole exome sequencing was performed. The Agilent SureSelect Human Exome Kit (v.4), (Agilent Technologies, Inc., Santa Clara, CA, USA) was used for target enrichment and the three sample DNAs were pooled together and used for paired-end sequencing of 100 cycles (generating 100 bp reads) on a single lane of Illumina HiSeq2000’s flow-cell (Illumina Inc., San Diego, CA, USA).
The sequence reads were aligned to the reference sequence of the human genome using Burrows–Wheeler transform algorithm. The Unified Genotyper module of the GATK package was used for calling both single-nucleotide polymorphisms and indels.29 Regions with at least eightfold depth of coverage were used for calling variants, and a different nucleotide from the reference sequence seen in at least 25% of the reads aligned to a given position were called as a variant.
Analysis was performed with more focus on all 18 known BBS genes for which the coverage was 96%, 97% and 97% at eightfold depth of coverage for the three samples. First, all the synonymous variants were removed. Then all the common variants (minor allele frequency >1%) reported in public databases were removed keeping our focus on rare variants only (minor allele frequency ⩽1). The dbNSFP database for predicting the functional effect of the missense variants was used.30 All missense variants predicted to be benign based on the dbNSFP database were removed from the list of variants. At last, confirmation of variants detected by exome sequencing was performed with Sanger sequencing of the specified region.
Final screening for mutation detection
Finally, six other BBS genes including BBS3, BBS4, BBS6, BBS7, BBS9 and BBS12, which account for about 20% of BBS patients, were screened in the remaining patients. Methods used for designing primers, sequencing and variant calling were the same as those used in the initial screening of three commonly mutated BBS genes. Eighty amplicons were sequenced for covering all 72 coding exons of the six BBS genes in this step.
To study the cosegregation of the detected variants, all the family members were analyzed for the specific variant, using Sanger sequencing. In cases of novel variants, additional 100 normal Iranian chromosomes were screened.
RT–PCR analysis
Total RNA was extracted from fresh blood using QIAamp RNA Blood Mini Kit (Qiagen, Hilden, Germany) or established Epstein–Barr virus-transformed lymphoblastoid cell lines with the help of RNeasy Mini Kit (Qiagen) and the following cDNA synthesis was carried out by QuantiTect Reverse Transcription Kit (Qiagen).
To investigate the effect of potentially splicing mutations on the expressed, novel variants located in or near splice sites were assessed by reverse transcription-polymerase chain reaction (RT–PCR) using primers designed to amplify the specified regions on cDNA to confirm the variant effect on the expression level. Amplified RT–PCR products were analyzed on 2% agarose gel and confirmed by Sanger sequencing of the purified bands with the help of QIAquick Gel Extraction Kit (Qiagen), according to the manufacturer’s protocol.
Results
Screening of the three most commonly mutated genes (BBS1, BBS2 and BBS10) results in the identification of causal mutations in BBS2 gene for four patients. That includes a nonsense mutation (p.Gln335*), two splicing variants (c.471G>C and c.1910+1G>T) and one frameshift insertion (c.256_278dup23). No mutation was found in BBS1 and BBS10 genes (Table 2).
RT–PCR analysis for the identified novel splicing mutation (c.1910+1G>T) in BBS2 gene revealed an unexpectedly 200 bp band, resulting in two alternatively spliced mRNA for BBS2 that is deletion of exon 14 and/or 15 for the mutated allele.31 Gel purification and Sanger sequencing of the cDNA products revealed that parents are heterozygous and the affected child is homozygous. Both alternatively spliced transcripts were observed in all members of the family and not the control samples. These clearly confirm the deleterious effect of this novel splicing mutation on BBS2 gene product (Figure 1).
(a) Sanger sequencing result on genomic level confirmed cosegregation of the splicing variant in the family. (b) Reverse transcription-polymerase chain reaction (RT–PCR) analysis for the novel identified splicing variant: c.1910+1 G>T in BBS2 gene. These entire bands were gel purified followed by sequencing. As schematically shown, the 481 bp band on gel electrophoresis indicated the presence of normal allele in parents as well as in the control sample, whereas there is no sign of amplification for the affected child. The second band, 368 bp, is the product of exon 15 skipping due to the abnormal splicing. The smallest band represents skipping of both exons 14 and 15 in all members of the family comparing to control samples. A full color version of this figure is available at the Journal of Human Genetics journal online.
Regarding the high conservation of the last guanine nucleotide and its possible role in splicing, the homozygous substitution in BBS2, c.471G>C (IVS3 ds G-C −1/p.T157T), is considered to have drastic impact on splicing machinery. As there was no further access to the family members, variant verification on RNA level was not feasible.
Whole exome sequencing for three of the patients revealed a novel BBS4 homozygous mutation (p.Gly277Arg) in one patient (Table 2). No pathogenic variation was identified in the coding regions of all the 18 known BBS genes in two other patients, suggesting possible presence of noncoding pathogenic variations in known genes or the possibility of novel genes for BBS phenotype in these patients.
In the final screening, direct sequencing of other six BBS genes resulted in the identification of causal mutations for seven other patients in BBS4, BBS7, BBS9 and BBS12. Those mutations include one deletion (c.77_220 del144) in BBS4, a compound heterozygous mutations (c.1342_1346 del CAGGC and p.Cys481*) in BBS7 in a non-consanguineous family, two splicing mutations in BBS9 (c.263+1G>A, c.1789+1G>A), one nonsense mutation (p.Arg386*) and one deletion (c.2019del) in BBS12 (Table 2).
RT–PCR analysis of the novel splicing mutation (c.263+1G>A) in BBS9 revealed neither exon skipping nor intron retention. This splice donor variant is reported as rs137962929 in dbSNP137 with a minor allele frequency of 0.0077 (Exome Variant Server, evs.gs.washington.edu/) and there is no report regarding its pathogenicity in HGMD mutation database causing BBS.32 RT–PCR products for all the family members, including parents, two affected children and one normal child, were not differentiable on agarose gel. Sanger sequencing of the PCR products revealed the addition of four nucleotides (ATAA) in mature mRNA in affected individuals leading to a premature stop codon (r.776_777 ins ATAA/ p.Gly89*), which cosegregates in the family. It should be noted that previous sequencing of the genomic regions did not reveal any insertion, proposing the disturbance in splicing machinery. The inserted ATAA could be originated from the third intron between these two exons, which has at least 14 ATAA repeats in its sequence, as well as at the beginning of the third exon’s sequence (Figure 2).
(a) Sanger sequencing on genomic level revealed c.263+1G>A in BBS9. (b) Reverse transcription-polymerase chain reaction (RT-PCR) analysis for the novel identified splicing variant: c.263+1G>A in BBS9 gene. The amplified products in the affected individual showed the same size as the control sample. (c) Sanger sequencing of the amplified region of cDNA revealed splicing inaccuracy or inefficiency that leads to insertion of ATAA on RNA level. (d) Sanger sequencing result on cDNA confirmed cosegregation of the splicing variant in the family. A full color version of this figure is available at Journal of Human Genetics online.
Deletion of exons 3 and 4 (c.77_220del144) of BBS4 gene in one family was confirmed by RT–PCR. This known deletion was previously observed in another Iranian patient (unpublished data), suggesting that it is a recurrent BBS4 mutation in Iranian BBS patients.33
It is noteworthy to mention another mutation: c.1156–1157 CG>TA (p.Arg386*) in BBS12 gene that is identified in two out of three BBS12 disease-associated patients of this study, which is a small-scale evidence for its predominance in BBS12-related Iranian patients.
Discussion
This study was performed to characterize responsible genes and mutation spectrum in a cohort of 14 Iranian families with BBS. In total, nine BBS genes (BBS1, BBS2, BBS3, BBS4, BB6, BBS7, BBS9, BBS10 and BBS12) were completely screened in these patients and the causal mutations in 12 of them were identified in five BBS genes.
Generally, the highest proportion of contributing genes in BBS belongs to BBS1 and BBS10, accounting for 23% and 20% of the cases, respectively. It should be noted that these contributions varies in different populations as the proportion of BBS1 and BBS10 extends to 40–50% in Northern European patients. In addition, the most common reported mutations are M390R in BBS1 and C91fs*95 in BBS10.2, 14 Screening the three most prevalent genes: BBS1, BBS2 and BBS10 in this study showed no mutation in BBS1 and BBS10, which is quite different from other populations, whereas 28.6% of patients of this study carried BBS2 mutations compared with the reported average contribution of 8–12% for BBS2 in most populations.34 It is noteworthy to mention that mutation hotspots are not common among BBS genes, except M390R in BBS1 and also C91fs*95 mutations, which are commonly (48%) found in patients with BBS10 disease-associated alleles in many populations such as European, as well as Middle Eastern and Arab populations.2, 35 The absence of BBS1 and BBS10 disease-associated mutations and also higher frequency of BBS2 mutations in a cohort of BBS patients with Iranian origin is completely different from Caucasian populations.
Although recognizable genotype–phenotype correlation is absent in BBS, there are some reports of milder phenotypes in BBS1- and BBS12-related disease compared with BBS10.34 Hjortshøj et al.36 observed that milder phenotype was mostly observed in patients who carried recurrent p.M390R mutation in the BBS1 gene. They concluded that the observed milder phenotype in BBS1 disease-associated patients could be explained by the type of mutation (missense in BBS1) compared with mostly truncating mutations in BBS10. The majority of our patients carry truncating mutations in BBS genes. This is consistence with the observation of mostly severe symptoms in our patients.
The only missense variant in this study was c.829G>A (p.Gly277Arg) identified by whole exome sequencing in the BBS4 gene. Bioinformatic predictions and multiple sequence alignment revealed high conservation for the Gly277, with deleterious effects on the protein level if this substitution happens (Figure 3). BBS4 is one of the conserved BBS proteins constituting BBSome, a protein complex with a role in biogenesis of primary cilium.37 It is proposed that centriolar satellites transport BBSome to the basal body of the cilium and the PCM1 helps the aggregation of BBSome by chaperonic functions. There are published data on interactions between BBS4-PCM1 and BBS8-PCM1, which indicates association of BBSome via these two proteins.36 The Gly277 in BBS4 is located in the region necessary for interaction with PCM1 protein. In the other word, this missense variant seems to disrupt the association between BBSome and PCM1 that may lead to its incorrect or disrupted transport. All these data together suggest the pathogenicity of c.829G>A (p.Gly277Arg) in this patient (Figure 3).
(a) Bioinformatic predictions and multiple sequence alignment (obtained from PolyPhen2 software) revealed high conservation for the Gly277 with destructive effects on the protein level if c.829G>A happens in BBS4. (b) Cosegregation of c.829G>A in family members is shown. A full color version of this figure is available at Journal of Human Genetics online.
Four out of 12 variants identified in this study were splicing variants. This was not beyond our expectation, as almost 10% of all the mutations reported in diseases can be caused by variants located in splice site sequences.38 This percentage could be extended to even 50% of disease-causing variants in genes with large number of exons.39 As it has been proposed such mutations could display different effects on pre-mRNA splicing process, such as, exon skipping, intron retention, introducing novel splice sites within exonic or intronic regions or activating cryptic splice sites located in the vicinity.40 These splicing effects are explained by the examples identified in the present work.
Regarding the RT–PCR results of c.1910+1 G>T in the BBS2 gene, the reason may lie in the essence of splicing reactions. In this case, there might be a cryptic splice site, which is activated under the impact of this substitution leading to deletion of both exons in the mature product. However, this activation seems to be not fully penetrant owing to the presence of PCR product including deletion of only one exon. Overall, regardless of whether one or two exons are deleted in the mature mRNA, this splice site variant removes at least a chain of 37 amino acids that might disrupt BBS2 protein interaction mostly with BBS7 and BBS9 proteins in BBSome complex.37 As stated, impairment of pre-mRNA splicing could be due to mutations in every sequence of the gene, but mostly located in highly conserved 5′ and 3′ locations. It is clear that there are other nucleotides in the vicinity that are highly conserved and their alterations might affect the normal pre-mRNA splicing reactions such as c.471G>C (IVS3 ds G-C −1/p.T157T) in BBS2 in the present work.39 It is noteworthy to mention that c.471G>T (p.T157T) has been reported in two patients originating from Lebanon. Although the nucleotide change on genomic level is different (G>T in the study by Deveault et al.34 and G>C in our study), the repeated report of c.471G substitution in BBS patients, who interestingly all come from Middle East, make another strong reason for involvement of this variant in the disease.34
In addition, based on the RT–PCR analysis, the impact of c.263+1G>A in BBS9 leads to creation of premature stop codon (PTC). This result could be explained by the fact that such errors in splicing regions could cause inefficient or inaccurate splicing reactions leading to the generation of PTC and inducing probable downstream reactions of nonsense-mediated decay followed by mRNA degradation, which is in fact the surveillance mechanism for the cell.41, 42, 43, 44 Regarding the location of PTC, which confines upstream of the 3′-most exon–exon junction with more than 50–55 nucleotides, nonsense-mediated decay might be activated to destroy the mature mRNA yielding no protein product.45 However, the presence of the specific mRNA in our study could be explained by the fact that translation is considered as the prerequisite of nonsense-mediated decay, meaning that mature mRNA will not be degraded unless the translation begins in the cytoplasm.44
According to the results achieved by this study, no mutation was identified in the following genes: BBS1, BBS3, BBS6 and BBS10.
BBS3 (ARL6) is one of the GTP-binding proteins with essential role in proper localization of BBSome.19 Regarding its unusual predominance in Saudi patients with BBS compared to the rare frequency of 0.4% in Caucasian populations plus an additional previous report of BBS3 in an Iranian family, a decision was made to screen the gene in the cohort of this study.46, 47 However, no mutation was identified in our cohort that reaffirms the BBS3 low frequency same as the Caucasian population.
Overall, nine BBS genes (BBS1, BBS2, BBS3, BBS4, BBS6, BBS7, BBS9, BBS10 and BBS12) each that accounted for >5% of BBS patients in previous reports were completely screened. However, the mutation frequency for BBS4 and BBS7 was just 2%. These two genes were selected based on the published higher frequency for BBS4 in Middle Eastern populations and previous observation of BBS7 in a cohort of 136 Iranian families with intellectual disability.48
This study represents the distribution of causal mutations among Iranian BBS patients, which is significantly different from the other reports, especially from Caucasian populations. The commonly mutated BBS1 and BBS10 genes were not mutated in our patients and may not have an important role in Iranian patients while other genes such as BBS2 (28.6% in this study), BBS4 (∼14% of this study), BBS12 (21.4% in this study) and BBS9 (∼14% of this study) seem to have a greater role in Iranian patients with BBS compared with other populations.
Although a small sample size is presented in this study, the obtained results indicated high and nearly the same prevalence for both BBS2 and BBS12 in our cohort of Iranian patients. There is not a common statement about the choice of BBS2 as the third most mutated gene. As proposed by Muller et al.,49 regarding the small coding region of BBS12, this gene could be considered in diagnostic approaches before BBS2, for efficient and rapid genotyping. However, this should not cause the underestimation about the large proportion of BBS2 among the patients in diagnostic approaches.49 These results suggest a different strategy in molecular genetics diagnostic approaches for BBS in Iran and possibly other Middle Eastern countries. However, the advent of high-throughput sequencing in recent years has changed the molecular diagnostic protocols for such disorders with clinical and genetic heterogeneity.50 The importance of studies such as the present one is represented by identifying the most common causes of this disorder in each population, which could elucidate an algorithm for clinical genetic practice that would clarify the screening protocols before applying more advance technologies such as next-generation sequencing.51 In conclusion, this study represents another strong indication for heterogeneity of the disorder and extends the mutational spectrum of the known BBS genes by introducing nine novel mutations in five BBS genes.
References
Tobin, J. L. & Beales, P. L. Bardet–Biedl syndrome: beyond the cilium. Pediatr. Nephrol. 22, 926–936 (2007).
Zaghloul, N. A. & Katsanis, N. Mechanistic insights into Bardet–Biedl syndrome, a model ciliopathy. J. Clin. Invest. 119, 428–437 (2009).
Green, J. S., Parfrey, P. S., Harnett, J. D., Farid, N. R., Cramer, B. C., Johnson, G. et al. The cardinal manifestations of Bardet–Biedl syndrome, a form of Laurence–Moon–Biedl syndrome. New Engl. J. Med. 321, 1002–1009 (1989).
Katsanis, N., Lupski, J. R. & Beales, P. L. Exploring the molecular basis of Bardet–Biedl syndrome. Hum. Mol. Genet. 10, 2293–2299 (2001).
Beales, P. L., Elcioglu, N., Woolf, A. S., Parker, D. & Flinter, F. A. New criteria for improved diagnosis of Bardet–Biedl syndrome: results of a population survey. J. Med. Genet. 36, 437–446 (1999).
Blacque, O. E. & Leroux, M. R. Bardet–Biedl syndrome: an emerging pathomechanism of intracellular transport. Cell. Mol. Life Sci. 63, 2145–2161 (2006).
Ajmal, M., Khan, M. I., Neveling, K., Tayyab, A., Jaffar, S., Sadeque, A. et al. Exome sequencing identifies a novel and a recurrent BBS1 mutation in Pakistani families with Bardet–Biedl syndrome. Mol. Vis. 19, 644–653 (2013).
Croft, J. B., Morrell, D., Chase, C. L. & Swift, M. Obesity in heterozygous carriers of the gene for the Bardet–Biedl syndrome. Am. J. Med. Genet. 55, 12–15 (1995).
Klein, D. & Ammann, F. The syndrome of Laurence–Moon–Bardet–Biedl and allied diseases in Switzerland. Clinical, genetic and epidemiological studies. J. Neurol. Sci. 9, 479–513 (1969).
M’hamdi, O., Ouertani, I., Maazoul, F. & Chaabouni-Bouhamed, H. Prevalence of Bardet–Biedl syndrome in Tunisia. J. Community Genet. 2, 97–99 (2011).
Farag, T. I. & Teebi, A. S. High incidence of Bardet–Biedl syndrome among the Bedouin. Clin. Genet. 36, 463–464 (1989).
Moore, S. J., Green, J. S., Fan, Y., Bhogal, A. K., Dicks, E., Fernandez, B. A. et al. Clinical and genetic epidemiology of Bardet–Biedl syndrome in Newfoundland: a 22-year prospective, population-based, cohort study. Am. J. Med. Genet. A 132, 352–360 (2005).
Hjortshoj, T. D., Gronskov, K., Brondum-Nielsen, K. & Rosenberg, T. A novel founder BBS1 mutation explains a unique high prevalence of Bardet–Biedl syndrome in the Faroe Islands. Br. J. Ophthalmol. 93, 409–413 (2009).
Forsythe, E. & Beales, P. L. Bardet–Biedl syndrome. Eur. J. Hum. Genet. 21, 8–13 (2013).
Katsanis, N. The oligogenic properties of Bardet–Biedl syndrome. Hum. Mol. Genet. 13, 65–71 (2004).
Marion, V., Stutzmann, F., Gerard, M., De Melo, C., Schaefer, E., Claussmann, A. et al. Exome sequencing identifies mutations in LZTFL1, a BBSome and smoothened trafficking regulator, in a family with Bardet–Biedl syndrome with situs inversus and insertional polydactyly. J. Med. Genet. 49, 317–321 (2012).
Scheidecker, S., Etard, C., Pierce, N. W., Geoffroy, V., Schaefer, E., Muller, J. et al. Exome sequencing of Bardet–Biedl syndrome patient identifies a null mutation in the BBSome subunit BBIP1 (BBS18). J. Med. Genet. 51, 132–136 (2014).
Wiens, C. J., Tong, Y., Esmail, M. A., Oh, E., Gerdes, J. M., Wang, J. et al. Bardet–Biedl syndrome-associated small GTPase ARL6 (BBS3) functions at or near the ciliary gate and modulates Wnt signaling. J. Biol. Chem. 285, 16218–16230 (2010).
Zhang, Q., Yu, D., Seo, S., Stone, E. M. & Sheffield, V. C. Intrinsic protein-protein interaction-mediated and chaperonin-assisted sequential assembly of stable Bardet–Biedl syndrome protein complex, the BBSome. J. Biol. Chem. 287, 20625–20635 (2012).
Khan, S., Ullah, I., Irfanullah, Touseef, M., Basit, S., Khan, M. N. et al. Novel homozygous mutations in the genes ARL6 and BBS10 underlying Bardet–Biedl syndrome. Gene 515, 84–88 (2013).
Beales, P. L., Katsanis, N., Lewis, R. A., Ansley, S. J., Elcioglu, N., Raza, J. et al. Genetic and mutational analyses of a large multiethnic Bardet–Biedl cohort reveal a minor involvement of BBS6 and delineate the critical intervals of other loci. Am. J. Hum. Genet. 68, 606–616 (2001).
Pawlik, B., Mir, A., Iqbal, H., Li, Y., Nurnberg, G., Becker, C. et al. A novel familial BBS12 mutation associated with a mild phenotype: implications for clinical and molecular diagnostic strategies. Mol. Syndromol. 1, 27–34 (2010).
Miller, S. A., Dykes, D. D. & Polesky, H. F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 16, 1215 (1988).
Neitzel, H. A routine method for the establishment of permanent growing lymphoblastoid cell lines. Hum. Genet. 73, 320–326 (1986).
Rozen, S. & Skaletsky, H. Primer3 on the WWW for general users and for biologist programmers. Methods Mol. Biol. 132, 365–386 (2000).
Adzhubei, I. A., Schmidt, S., Peshkin, L., Ramensky, V. E., Gerasimova, A., Bork, P. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Kumar, P., Henikoff, S. & Ng, P. C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat. Protoc. 4, 1073–1081 (2009).
Berezin, C., Glaser, F., Rosenberg, J., Paz, I., Pupko, T., Fariselli, P. et al. ConSeq: the identification of functionally and structurally important residues in protein sequences. Bioinformatics 20, 1322–1324 (2004).
McKenna, A., Hanna, M., Banks, E., Sivachenko, A., Cibulskis, K., Kernytsky, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Liu, X., Jian, X. & Boerwinkle, E. dbNSFP: a lightweight database of human nonsynonymous SNPs and their functional predictions. Hum. Mutat. 32, 894–899 (2011).
Keren, H., Lev-Maor, G. & Ast, G. Alternative splicing and evolution: diversification, exon definition and function. Nat. Rev. Genet. 11, 345–355 (2010).
Stenson, P. D., Mort, M., Ball, E. V., Howells, K., Phillips, A. D., Thomas, N. S. et al. The Human Gene Mutation Database: 2008 update. Genome Med. 1, 13 (2009).
Mykytyn, K., Braun, T., Carmi, R., Haider, N. B., Searby, C. C., Shastri, M. et al. Identification of the gene that, when mutated, causes the human obesity syndrome BBS4. Nat. Genet. 28, 188–191 (2001).
Deveault, C., Billingsley, G., Duncan, J. L., Bin, J., Theal, R., Vincent, A. et al. BBS genotype–phenotype assessment of a multiethnic patient cohort calls for a revision of the disease definition. Hum. Mutat. 32, 610–619 (2011).
Slavotinek, A. & Beales, P. Clinical utility gene card for: Bardet–Biedl syndrome. Eur. J. Hum. Genet. (e-pub ahead of print 8 December 2010; doi:10.1038/ejhg.2010.199).
Hjortshøj, T. D., Gronskov, K., Philp, A. R., Nishimura, D. Y., Riise, R., Sheffield, V. C. et al. Bardet–Biedl syndrome in Denmark—report of 13 novel sequence variations in six genes. Hum. Mutat. 31, 429–436 (2010).
Jin, H., White, S. R., Shida, T., Schulz, S., Aguiar, M., Gygi, S. P. et al. The conserved Bardet–Biedl syndrome proteins assemble a coat that traffics membrane proteins to cilia. Cell 141, 1208–1219 (2010).
Mykytyn, K., Nishimura, D. Y., Searby, C. C., Beck, G., Bugge, K., Haines, H. L. et al. Evaluation of complex inheritance involving the most common Bardet–Biedl syndrome locus (BBS1). Am. J. Hum. Genet. 72, 429–437 (2003).
Krawczak, M., Thomas, N. S., Hundrieser, B., Mort, M., Wittig, M., Hampe, J. et al. Single base-pair substitutions in exon–intron junctions of human genes: nature, distribution, and consequences for mRNA splicing. Hum. Mutat. 28, 150–158 (2007).
Baralle, D. & Baralle, M. Splicing in action: assessing disease causing sequence changes. J. Med. Genet. 42, 737–748 (2005).
Chanfreau, G. F. A dual role for RNA splicing signals. EMBO Rep. 11, 720–721 (2010).
Nagy, E. & Maquat, L. E. A rule for termination-codon position within intron-containing genes: when nonsense affects RNA abundance. Trends Biochem. Sci. 23, 198–199 (1998).
Maquat, L. E. Nonsense-mediated mRNA decay. Curr. Biol. 12, 196–197 (2002).
Stamm, S., Ben-Ari, S., Rafalska, I., Tang, Y., Zhang, Z., Toiber, D. et al. Function of alternative splicing. Gene 344, 1–20 (2005).
Maquat, L. E. Nonsense-mediated mRNA decay in mammals. J. Cell. Sci. 118, 1773–1776 (2005).
Ghadami, M., Tomita, H. A., Najafi, M. T., Damavandi, E., Farahvash, M. S., Yamada, K. et al. Bardet–Biedl syndrome type 3 in an Iranian family: clinical study and confirmation of disease localization. Am. J. Med. Genet. 94, 433–437 (2000).
Abu Safieh, L., Aldahmesh, M. A., Shamseldin, H., Hashem, M., Shaheen, R., Alkuraya, H. et al. Clinical and molecular characterisation of Bardet–Biedl syndrome in consanguineous populations: the power of homozygosity mapping. J. Med. Genet. 47, 236–241 (2010).
Najmabadi, H., Hu, H., Garshasbi, M., Zemojtel, T., Abedini, S. S., Chen, W. et al. Deep sequencing reveals 50 novel genes for recessive cognitive disorders. Nature 478, 57–63 (2011).
Muller, J., Stoetzel, C., Vincent, M. C., Leitch, C. C., Laurier, V., Danse, J. M. et al. Identification of 28 novel mutations in the Bardet–Biedl syndrome genes: the burden of private mutations in an extensively heterogeneous disease. Hum. Genet. 127, 583–593 (2010).
Redin, C., Le Gras, S., M'hamdi, O., Geoffroy, V., Stoetzel, C., Vincent, M. C. et al. Targeted high-throughput sequencing for diagnosis of genetically heterogeneous diseases: efficient mutation detection in Bardet–Biedl and Alstrom syndromes. J. Med. Genet. 49, 502–512 (2012).
M'hamdi, O., Ouertani, I. & Chaabouni-Bouhamed, H. Update on the genetics of Bardet–Biedl syndrome. Mol. Syndromol. 5, 52–57 (2013).
Nishimura, D. Y., Swiderski, R. E., Searby, C. C., Berg, E. M., Ferguson, A. L., Hennekam, R. et al. Comparative genomics and gene expression analysis identifies BBS9, a new Bardet-Biedl syndrome gene. Am. J. Hum. Genet. 77, 1021–1033 (2005).
Acknowledgements
We would like to thank our patients and their families for the collaboration in this research. This study could not be completed without the assistance of Dr Sharifian, Dr Riazi, Dr Bozorgmehr, Dr Jamali, Dr Shafaghati and Dr Davarnia, who referred the patients to our Center. This research project has been funded by Kariminejad–Najmabadi Pathology and Genetics Center, Tehran, Iran.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Fattahi, Z., Rostami, P., Najmabadi, A. et al. Mutation profile of BBS genes in Iranian patients with Bardet–Biedl syndrome: genetic characterization and report of nine novel mutations in five BBS genes. J Hum Genet 59, 368–375 (2014). https://doi.org/10.1038/jhg.2014.28
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.28
This article is cited by
-
BBS4 Is Essential for Nuclear Transport of Transcription Factors Mediating Neuronal ER Stress Response
Molecular Neurobiology (2021)