Abstract
Rare but severe adverse drug reactions (ADRs) are an important issue in drug development and in the proper usage of drugs during the post-approval phase. The ability to predict patient susceptibility to severe ADRs would prevent drug administration to high-risk patients. This would save lives and ensure the quality of life for these patients, but occurrence of idiosyncratic severe ADRs had been very difficult to predict for a long time. However, in this decade, genetic markers have been found for several ADRs, especially for severe cutaneous adverse reactions (SCARs) and drug-induced liver injury (DILI). In this review, we summarize recent progress in identifying genetic markers for SCARS and DILI, and discuss issues that remain unresolved. As for SCARs, associations of HLA-B*15:02 or HLA-A*31:01 and HLA-B*58:01 have been revealed for carbamazepine- and allopurinol-related Stevens–Johnson syndrome and toxic epidermal neclolysis, respectively. HLA-B*57:01 is strongly associated with abacavir-induced hypersensitivity syndrome. Several HLA alleles also demonstrate drug-specific associations with DILI, such as HLA-A*33:03 for ticlopidine, HLA-B*57:01 for flucloxacillin and HLA-DQA1*02:01 for lapatinib. Efforts should be continued to find other genetic markers to achieve high predictability for ADRs, with the goal being development of genetic tests for use in clinical settings.
Similar content being viewed by others
INTRODUCTION
Adverse drug reactions (ADRs) are known to occur with large interindividual variation, and may lead to life threatening or fatal in some patients. In the United States, the overall incidence of serious ADRs was 6.7% from 1966 to 1996, with fatal ADRs reaching 0.32% of hospitalized patients.1 A recent study in Japan found 1010 ADRs in 3459 adult patients in 2004, and of these, 1.6%, 4.9% and 33% were fatal, life threatening and serious, respectively.2 These interindividual differences could be attributable, at least in part, to environmental factors such as coadministered drugs (causing drug–drug interactions), foods, smoking and drinking habits, and underlying disease. In addition, genetic factors could be very important determinants of susceptibility to ADRs. Many genetic polymorphisms affecting protein expression levels and/or functions have been reported as contributing to ADR. These genetic polymorphisms include substitutions, insertions or deletions of nucleotides, variations in copy number and duplications or deletions of entire genes. The functional polymorphisms, particularly in drug-metabolizing enzymes, transporters and other drug response-related genes, are occasionally associated with altered pharmacokinetics and efficacy of drugs, as well as induction of adverse reactions.
ADRs can be divided into two basic types.3 Type A is related to the pharmacological actions of the drug and is therefore predictable. Type A-ADRs are usually dose-dependent, and are in some instances amenable to dose reduction. In contrast, type B-ADRs are thought to be unrelated to the known pharmacological actions of a drug, and thus are unpredictable. They are often referred to as ‘idiosyncratic’ adverse reactions, lacking a simple dose–response relationship to explain their occurrence. In general, type B reactions are severe and occasionally life threatening, and often lead to cessation of a drug in the market.
In this review, we summarize recent pharmacogenomic progress related to two type of B-ADRs: severe cutaneous adverse reactions (SCARs) and drug-induced liver injuries (DILIs). We will review genetic associations and predictors for the occurrence of SCARs and DILI, and the application of this information towards the prevention of these severe reactions.
SEVERE CUTANEOUS ADVERSE REACTIONS (SCARs)
Skin rash is a frequently occuring ADR. However, Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) and drug-induced hypersensitivity syndrome (DIHS) are life-threatening SCARs accompanied by fever and systemic complications. SJS and TEN with characteristic mucosal and cutaneous disorders are considered to represent different severities of the same disease. The most widely accepted classification is based on the degree of skin detachment expressed in terms of the % body surface area affected. SJS is defined as an area of skin detachment involving <10% of the body surface. SJS–TEN overlap is defined as an area of skin detachment affecting from 10 to 30% of the body surface. TEN is defined as a level of skin detachment not >30%.4 In Japan, TEN is defined as a severity of skin detachment involving >10% of the body surface.5 DIHS has also been referred to as drug reaction with eosinophilia and systemic symptoms or hypersensitivity syndrome (HSS). DIHS is a severe adverse reaction leading to multi-organ failure and hypothesized to be associated with reactivation of herpes virus-6. The incidence of these SCARs is estimated to be 2–3 cases per million per year, but this estimate may vary depending on the ethnic group. As for causative agents, DIHS is caused by a limited number of drugs, including carbamazepine, salazosulfapyridine, allopurinol and mexiletine hydrochloride,6 whereas SJS/TEN is known to be caused by more than 100 kinds of drugs. In Japan, although carbamazepine and allopurinol had been leading causative drugs until 2010, the number of SJS/TEN cases induced by lamotrigine has increased since the approval of lamotrigine in 2008.7 In 2011, lamotrigine was the leading cause of drug-induced SJS/TEN. Other causative drugs include nonsteroidal anti-inflammatory drugs and analgesics such as loxoprofen, celecoxib, acetaminophen and cold remedies. Cephalosporin, synthetic antibacteria agents and aromatic antiepileptic drugs such as zonisamide and phenytoin also often induce SJS/TEN.
SJS/TEN is considered to be delayed-type allergic reaction involving T cells.8 Recent reports have implicated the involvement of some human leukocyte antigen (HLA) class I molecules in the development of specific drug-induced SJS/TEN or SCARs, as discussed below.
SCARs: CARBAMAZEPINE
Associations between carbamazepine-induced SCARs and HLA alleles in various ethnic groups are summarized in Table 1. HLA-B*15:02 was initially reported to have a strong association with carbamazepine-induced SJS/TEN in Han Chinese in Taiwan by Chung et al.9 The carrier frequency of HLA-B*15:02 in their cases (n=44) was 100%, which was significantly higher than that of carbamazepine-tolerant patients (3%, n=101) (P=3.13 × 10−27), and the extremely high odds ratio (OR) 2504 was observed. Using patients originating from Southeastern Asia, numerous studies that have included their continuing follow-up analysis have confirmed this strong association, as shown in Table 1.10, 11, 12, 13, 14, 15 However, no carriers of HLA-B*15:02 have been detected in Caucasians12 with carbamazepine-induced SJS/TEN. Furthermore, none of the patients from Southeastern Asia displaying other phenotypes of cutaneous adverse reactions, including HSS or mild skin rash such as maculopapular erythroderma (MPE), were carriers of HLA-B*15:02, although both HSS and MPE are considered to be T-cell mediated delayed-type allergic reactions.10 The incidence rate of SJS/TEN in some Southeastern Asian countries, including Taiwan, Thailand, Malaysia and the Philippines, is 10-fold higher than the rates observed in Europe, USA or Japan.16 The higher frequencies of the HLA-B*15:02 allele (2–12%) in Southeastern Asian populations compared with the frequencies in Caucasians may explain the higher incidence rates of this adverse reaction and the strong associations. HLA-B*15:02 was also reported to be a biomarker for phenytoin-induced SJS/TEN in Taiwanese.17
Although an association with HLA-B*15:02 has not been established like in Caucasians, significant associations between HLA-B*15:11 and carbamazepine-induced SJS/TEN have been found in Japanese (OR=16.3, P=0.0004) and Korean patients (OR=18.0, P=0.002).18, 19 Interestingly, HLA-B*15:11 and HLA-B*15:02 belong to the same serotype, HLA-B75. Other major family members of the HLA-B75 serotype are HLA-B*15:08 and HLA-B*15:21. Although a statistical analysis has not been conducted, Asian patients with carbamzepine-induced SJS/TEN who carry HLA-B*15:11, HLA-B*15:08 or HLA-B*15:21 have been found.13, 14
Recently, Wei et al.20 estimated the molecular basis of the associations between various subfamilies of HLA-B75 and carbamazepine-induced SJS/TEN. A cell line transfected with HLA-B*15 has shown that all HLA-B75 members, including HLA-B*15:02 and HLA-B*15:11 proteins, promote cell lysis by cytotoxic T cells that have been activated by carbamazepine. In contrast, members of other serotypes of HLA-B*15 such as HLA-B62 and HLA-B72 cannot promote the cell lysis.20
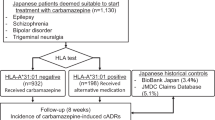
In addition to the HLA-B75 members, an association between carbamazepine-induced SCARs and HLA-A*31:01 was detected for the first time in Japanese patients by Kashiwagi et al.21 (OR=4.33, P=0.0004) and confirmed by Ozeki et al.22 (OR=33.9, P=2.35 × 10−4 for SJS/TEN) and Niihara et al.23 (OR=11.2, P=0.001 for HLA-A31). These studies showed that expression of HLA-A*31:01 correlates with the occurrence of various types of SCARs, such as SJS/TEN, DIHS (HSS), MPE and erythema exsudativum multiforma in Japanese patients. HLA-A*31:01 was also reported to be a biomarker for various carbamazepine-induced cutaneous adverse reactions in Europeans, ranging from mild skin rash, such as MPE, to SCARs, including SJS/TEN (OR=25.93, P=8.0 × 10−5).24 HLA-A*31:01 had been considered a biomarker for carbamaepine-induced MPE and HSS, but not for SJS/TEN in Han Chinese in Taiwan.10 Overall, in Japan and Korea, the occurrence of carbamazepine-induced SJS/TEN correlated significantly with both HLA-A*31:01 and HLA-B*15:11.18, 19, 21, 22, 23
Thus, it can be said that HLA-B75 is a risk factor for carbamazepine-induced SJS/TEN in Southeastern countries, that both HLA-A*31:01 and HLA-B*15:11 are the risk factors for carbamazepine-induced SJS/TEN for Japanese and Korean populations, and that HLA-A*31:01 is a risk factor for various types of SCARs in European populations.
SCARs: ALLOPURINOL
Associations between other drug-induced SCARs and HLA alleles are summarized in Table 2. Allopurinol is used as a urate-lowering drug and frequently causes SCARs, including SJS/TEN. Hung et al.25 published the first report of a strong association between allopurinol-induced SCARs and HLA-B*58:01 in Han Chinese patients living in Taiwan (OR=580.3, P=4.7 × 10−24). In contrast to the case of the biomarker HLA-B*15:02, which is specific to Southeastern Asian patients with carbamazepine-induced SJS/TEN, this association has been confirmed in studies of other Asian26, 27, 28, 29, 30 and European patients.12 Indeed, HLA-B*58:01 is involved in the development of various types of SCARs both in Japanese (OR=62.8, P=5.39 × 10−12 for SJS/TEN)27, 28, 29 and Korean (OR=97.8, P=2.45 × 10−11 for SJS/TEN/HSS)30 patients. A genome-wide association study (GWAS) with Japanese patients detected single-nucleotide polymorphisms (SNPs) on chromosome 6 that absolutely linked with HLA-B*58:01,29 and an inexpensive and simple screening test for HLA-B*58:01 using one of the SNPs (rs9263726) has been developed.31 Unfortunately, no other significantly associated SNPs in other area/chromosomes were found in this GWAS. It is also notable that HLA-B*58:01 is not only a risk factor for severe cutaneous reactions, such as SJS/TEN and DIHS, but also a risk factor for mild cutaneous adverse reactions, such as MPE, in the Han Chinese population.32
SCARs: ABACAVIR
Abacavir is a commonly used nucleotide analog with antiviral activity against HIV-1. Approximately 5–9% of Caucasian patients develop HSS within 6 weeks after the initial exposure to abacavir.33 Martin et al.34 reported the association between abacavir-induced HSS and HLA-B*57:01 in Western Australian HIV patients. Initially, this association was ambiguous in African patients.35, 36 However, as shown in Table 2, for patients immunologically confirmed by skin patch test using abacavir solutions, the carrier frequencies of HLA-B*57:01 were 100% both in Caucasian (42/42) and African patients (5/5).37 Thus, HLA-B*57:01 is now regarded as a common risk factor for abacavir-induced HSS, both for Caucasians and Africans. While HLA-B*57:01 is a common allele in Caucasians, this allele is rare in Asians.38 To date, few patients with abacavir-induced HSS who carry HLA-B*57:01 have been detected in Asia.39, 40
SCARs: NEVIRAPINE
Nevirapine is a potent non-nucleoside reverse transcriptase inhibitor used for the treatment of HIV-1 infection, but it frequently causes various types of skin rashes. The HLA-B*35:05 allele was observed in 17.5% of Thai patients with nevirapine-induced skin rash, compared with only 1.1% of nevirapine-tolerant Thai patients (OR=18.96, P corrected for multiple comparison, Pc=4.6 × 10−6) and 0.7% of the general Thai population (OR=29.87, Pc=2.6 × 10−5).41 Thus, the HLA-B*35:05 allele is a strong predictor for nevirapine-induced adverse skin reactions in HIV-infected Thai patients.
SCARs: METHAZOLAMIDE AND ACETAZOLAMIDE
Methazolamide and acetazolamide are sulfonamide derivatives used as carbonic anhydrase inhibitors to lower intraocular pressure associated with glaucoma. Case reports on SJS/TEN induced by methazolamide or acetazolamide have been primarily limited to Korean and Japanese patients.41, 42, 43, 44, 45, 46 The HLA-B59 serotype/HLA-B*59:01 has been reported to have associations with methazolamide- or acetazolamide-induced SJS/TEN (Table 2).42, 44, 45, 46, 47, 48 The allelic frequency of HLA-B*59:01 is 1–2% in the Japanese and Korean populations, but is very rare in Caucasians and Africans.38
SCARs: TRICHLOROETHYLENE
Trichloroethylene is not a drug, but an organic solvent that is often used in industries. It has caused SCARs in industry workers and local habitants in close proximity to the industries where this substance is used. The association between trichloroethylene-induced hypersensitivity and HLA-B*13:01 in Chinese has been reported.49
SJS/TEN WITH OCULAR COMPLICATIONS
PRESCREENING GENETIC BIOMARKERS TO PREVENT SCARs
A prospective, multicenter, double-blind study called PREDICT-I was conducted to evaluate screening for HLA-B*57:01 to prevent HSS caused by abacavir.52 In this study, nearly 2000 abacavir-naive, HIV-infected patients in Europe and Australia were randomly divided into two groups. In the first group, prospective screening for HLA*57:01 was applied to exclude HLA-B*57:01-positive patients from abacavir treatment. In the second group (control group), abacavir was given to all patients. Six weeks after initiating abacavir treatment, the incidence rate of HSS in both groups was compared. The rate of HSS occurrence in the group receiving prospective screening was significantly lower (3.4%) than the rate of HSS in the control group (7.8%). No patients were positive to abacavir patch test in the first group, whereas about one-third of the HSS patients in the second group (2.7%) were positive. Therefore, in the group receiving prescreening, no immunologically confirmed abacavir-induced HSS occurred. Thus, screening for HLA-B*57:01 before initiation of treatment is useful for reducing the risk of hypersensitive reactions to abacavir. In this condition, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 100%, 96.9%, 47.9% and 100%, respectively. Currently, prescreening for HLA-B*57:01, before initiation of abacavir treatment, is recommended in the United States and mandatory in the European Union.
In December 2007, Taiwan was the first country to include a warning in the package inserts of carbamazepine products that HLA-B*15:02 is a risk factor for carbamazepine-induced SJS/TEN. Carbamazepine had been newly prescribed to around 50 000 patients each year in that country, and the average incidence rate of carbamazepine-induced SJS/TEN between 2002 and 2004 was estimated to be 0.22% (approximately 115 patients a year).53 In a prospective study performed in Taiwan using 4877 carbamazepine-naive patients from 23 hospitals, carbamazepine was administered to only HLA-B*15:02-negative patients. Within 2 months, none of the 4120 patients who took carbamazepine developed SJS/TEN. Therefore, prescreening for HLA-B*15:02 could prevent about 10 patients (4877 × 0.0022) from SJS/TEN. Currently, screening HLA-B*15:02 or HLA-B*58:01 before initiation of treatment with carbamazepine or allopurinol is mandatory. Based on the results obtained in the prospective study mentioned above, the HLA-B*15:02 test is now covered by the National Health Insurance in Taiwan.
PATHOGENESIS OF DELAYED DRUG-HYPERSENSITIVITY REACTIONS
As described so far, various genetic biomarkers for SCARs have been reported. These markers may be specific to individual causative drugs or chemicals, or may be prevalent in certain ethnic groups or phenotypes of cutaneous adverse reactions. However, the majority of patients who possess a genetic risk factor for SCARs have been tolerant to the corresponding causative drug, and thus their pathogenesis should be studied intensively.
In addition to carbamazepine binding to HLA-B75 molecules and triggering activation of T cells for targeted lysis as described earlier,20 Ko et al.54 examined T-cell receptor (TCR) repertoire usage in carbamazepine-induced SJS/TEN patients (n=19) and also the tolerant patients (n=17) who carried HLA-B*15:02. A specific type of the third complementarity-determining region of the TCR, VB-11-ISGSY, was used in 84% of carbamazepine-induced SJS/TEN patients, but this was not used in the tolerant patients. This study also suggested that carbamazepine-specific cytotoxicity could be primed in vitro in peripheral blood mononuclear cells obtained from healthy subjects carrying HLA-B*15:02 and VB-11-ISGSY, and that the cytotoxicity was blocked by an anti-VB-11 antibody. Thus, usage of a specific TCR repertoire may be a critical factor for the development of SJS/TEN induced by carbamazepine.
Carbamazepine is considered to bind noncovalently and directly to HLA,20 whereas abacavir hypersensitivity may invoke a hapten/prohapten-related mechanism, including antigen processing.55 Differences in amino-acid sequence were observed between endogenous peptides isolated from the abacavir-treated HLA-B*57:01-positive B cells and the untreated B cells. Novel drug-induced peptides contained predominantly isoleucine or leucine residue in the carboxyl terminal, which presents a distinct characteristic compared with the residues of the usual endogenous HLA-B*57:01 peptides. From these results, Norcross et al.55 concluded that abacavir induced the loading of novel self-peptides into the HLA-B*57:01 molecule, resulting in the presentation of neo-antigenic peptides that drive polyclonal T-cell autoimmune responses and multi-organ systemic toxicity.
DRUG-INDUCED LIVER INJURY (DILI)
DILI is the most frequently reported adverse drug event in Japan, and most common cause of acute liver failure and transplantation in Western countries. The annual incidence of DILI has been estimated to be 5–10 in 100 000 inhabitants in France.56 Several drugs such as troglitazone, trovafloxacin and tolcapone were withdrawn from the market because of onset of DILI, and, similarly to SCARs, many drugs were regarded as causative for DILI. DILI associated with most drugs is considered idiosyncratic, and although its pathogenesis is poorly understood, immune-mediated (known as allergic) and metabolism-mediated mechanisms for this response have been proposed. DILI is diagnosed using several scoring schemes, such as the Roussel Uclaf Causality Assessment Method (also known as the Council for International Organization of Medical Sciences Scale),57 and the Japanese DDW-J 2004,58 and classified as hepatocellular, cholestasis and a mixture of these two types.
Until now, several drug-specific associations with genetic polymorphisms have been reported, particularly with HLA alleles. In Table 3, we have summarized the reported genetic associations with DILI.
DILI: UNSPECIFIED DRUGS
A study from southern Spain was conducted in which HLA-DRB and HLA-DQB genotypes of 140 definitive or probable DILI cases (according to their Roussel Uclaf Causality Assessment Method scores) were compared with those of 635 healthy volunteers. There was no prevalent drug in case patient groups. The researchers found that the frequencies of DRB1*15 (OR=2.31, P=0.002) and DQB1*06 (OR=2.32, P=0.001) were significantly higher in patients with cholestatic/mixed-type DILI, compared with the controls.59 By contrast, the frequencies of DRB1*07 (OR=0.37, P=0.003) and DQB1*02 (OR=0.39, P=0.0003) were significantly lower. Recent results from a large-scale study using subjects of European ancestry (783 cases and 3001 controls) did not reveal any significant genome-wide associations, including genes in the HLA region, after approximately 1 000 000 SNPs were searched and DILI samples due to flucloxacillin and amoxicillin/clavulanate were removed because of their high incidence rates. However, rs7574865, located in the vicinity of the STAT4 gene, yielded weak associations with hepatocellular type of DILI (P=4.5 × 10−4 in an exploratory study with 256 cases and P=0.011 in a validation study involving 168 cases).60
DILI: TROGLITAZONE
This innovative thiazolizinedione drug used to treat type II diabetes mellitus was introduced into the Japanese and US markets in 1997, but was voluntarily withdrawn from the market in 2000 because of idiosyncratic DILI that resulted in four documented deaths.61 Watanabe et al.62 analyzed 110 Japanese patients who were administered troglitazone, where 25 were DILI cases with at least a 9- or 5-fold increase in alanine aminotransferase or aspartate aminotransferase from the upper limit of normal values, respectively. For the rest of the patients, 85 tolerant controls, there were no remarkable increases in alanine aminotransferase or aspartate aminotransferase noted up to 6 months after troglitazone treatment. Genetic analysis was performed on 68 polymorphic sites of 51 candidate genes involved in drug metabolism, apoptosis, oxidative stress or the signaling pathways of the target proteins peroxisome proliferator-activated receptor gamma 2 and insulin. As a result, a strong association was observed in the combined null genotypes of the glutathione S-transferases (GSTs) GSTM1 and GSTT1, with an OR of 3.692 (P=0.008). The genotype frequencies of the GSTM1-GSTT1 double null were calculated as 0.248 in Japanese, 0.104 in Caucasians and 0.061 in African populations.63 It is noteworthy that other factors would be involved in the troglitazone-induced DILI, because this genotype in the Japanese population is rather common compared with the DILI incidence rate, and the OR is relatively small. GSTs are the family of detoxifying enzymes that mediate conjugation of reduced glutathione with a variety of electrophilic compounds, including reactive metabolites generated from therapeutic drugs.64 Several studies demonstrated that the chemically reactive metabolites derived from troglitazone are produced in the liver, besides the stable major metabolites.61
In addition to troglitazone, associations with the GSTM1-GSTT1 double null genotype were reported in 154 Caucasian patients having other drug-related DILIs, compared with 250 sex- and age-matched healthy controls.65 The ORs for DILI patients receiving anti-infectives (n=49), antibacterials (n=44) and nonsteroidal anti-inflammatory drugs (n=19) were 3.12 (P=0.006), 3.52 (P=0.002) and 5.61 (P=0.001), respectively. In Japanese epileptic patients administering carbamazepine, alanine aminotransferase and aspartate aminotransferase were higher in patients with a double null genotype (n=41) compared with GSTM1-GSTT1 double positive patients (n=50, P=0.01 and 0.02, respectively).66 A meta-analysis showed a significant association of the GSTM1 null genotype (but not the GSTT1 null genotype) with anti-tuberculosis DILI in East Asians, with an OR of 1.55 (P=0.024).67
DILI: TICLOPIDINE
Ticlopidine is an anti-platelet drug that is used in the treatment of atherothrombosis. Severe DILI, primarily the cholestatic type, rarely occurs with ticlopidine, but is relatively more frequent in Japanese than in Caucasians.68 Genetic risk factors for ticlopidine-related DILI were investigated in 22 cases (including 14 of the cholestasis type) and 85 tolerant controls, all of them Japanese patients.69 The target genes included seven cytochrome P450s, five oxidative stress-related genes and six HLAs (HLA-A, -B, -C, -DRB1, -DQB1 and -DPB1). HLA-A*33:03 was significantly associated with ticlopidine-induced DILI, with an OR of 13.0 (Pc=1.24 × 10−5) for all cases, and an OR of 36.5 (Pc=7.32 × 10−7) for the cholestatic cases. The frequency of the HLA-A*33:03 genotype in the Japanese population (0.067) is known to be higher than in Caucasians (0.0065).38 No significant association was observed for any of the other genotypes (P<0.01) on cytochrome P450s and oxidative stress-related genes.
The association with HLA was further enhanced by haplotypes of CYP2B6, which is involved in formation of the S-oxide active metabolite, of ticlopidine. CYP2B6*1H or CYP2B6*1J were both associated with an increase in its transcriptional activity, and the patients with both CYP2B6*1H or CYP2B6*1J and HLA-A*33:03 had a higher OR (38.82) than the patients possessing only HLA-A*33:03 (OR=15.48) when compared with double negative patients.70 CYP2B6 is hypothesized to have a role in the production of a ticlopidine-protein adduct. This could potentially lead to degradation of the adducted proteins into the drug-conjugated peptide, and its binding to HLA-A*33:03 proteins for activation of T cells.
DILI: AMOXICILLIN-CLAVULANATE
Amoxicillin-clavulanate (AC) is one of the most commonly prescribed antibacterials worldwide. Clavulanate is a potent β-lactamase inhibitor that prevents degradation of amoxicillin. Associations of AC-related DILI with HLA alleles have been reported in several studies. The first study, conducted in Belgium, analyzed 35 case patients and 60 healthy volunteers and found that the HLA-DRB1*15:01-DRB5*01:01-DQB1*06:02 haplotype was more prevalent in DILI cases than in controls (Pc<0.0002).71 Another small-scale study in Scotland confirmed this association: the HLA-DRB1*15:01 frequency was significantly higher in 20 AC-related jaundice patients compared with 134 volunteers (OR=9.25, P<2.5 × 10−6), and all patients with HLA-DRB1*15:01 had the DRB1*15:01-DRB5*01:01-DQB1*06:02 haplotype.72 Results from a third study derived from a UK-wide DILIGEN consisting of 61 cases and 191 population controls supported the association of HLA-DRB1*15:01 (OR=2.59, P=0.002).73 The last study first employed the GWAS technique, analyzing 822 927 SNPs for 201 White AC-related DILI cases and 532 population controls from Europe and USA.74 A single sharp peak was found at chromosome 6 in a Manhattan plot for −log10 P-values on the y-axis, in which the associated SNPs were linked with HLA-DQB1*06:02 (OR=3.3, P=1.4 × 10−6) and HLA-DRB1*15:01, and independently with HLA-A*02:01 (OR=2.2, P=2 × 10−6). Assuming that the prevalence of AC-DILI is 0.014%, the best PPV and NPV by the two HLA alleles in Northwestern Europeans were estimated to be 0.1% and 99.9%, respectively.
DILI: FLUCLOXACILLIN
This semi-synthetic penicillin is widely used in European countries and Australia for the treatment of staphylococcal infection. Its usage has been known to be associated with cholestatic hepatitis with a prevalence of 10.3 in every 100 000 new users in the United Kingdom.75 A GWAS study for 866 399 SNPs, using 51 flucloxacillin-related DILI cases and 282 sex- and age-matched controls, revealed many associated SNPs at the short arm of chromosome 6.76 The strongest association was with rs2395029 (OR=45, P=8.7 × 10−33), which was known to be in complete linkage disequilibrium with HLA-B*57:01. The ORs using 64 flucloxacillin-tolerant controls were 80.6 (P=8.97 × 10−19) compared with the exploration cases (n=51), and 100 (P=6.62 × 10−13) compared with the replication cases (n=23). Other SNPs in the HLA region, such as TNF rs361525, also showed a significant association, but none of the SNPs were significant after conditioning with HLA-B*57:01. The HLA-B*57:01 frequency is 0.01–0.03 in Northern Europeans, but is <0.001 in Japanese.38 Flucloxacillin has not been approved for clinical use in Japan. It is interesting to know the molecular pathogenic basis in the future because HLA-B*57:01 is also associated with abacavir-induced HSS.
DILI: LAPATINIB
Lapatinib is a tyrosine kinase inhibitor targeting human epidermal growth factor receptor 2 and epidermal growth factor receptor, and is used in patients with advanced or metastatic breast cancer. In a study seeking to identify genomic markers for sensitive patients to DILI, a significant association of HLA-DQA1*02:01 with lapatinib-related DILI was found in both exploratory (35 cases and 283 controls, OR=2.6, P=0.03) and validation (24 cases and 155 controls, OR=9.0, P=0.00008) studies.77 Its PPV and NPV with regard to HLA-DQA1*02:01 were 0.17 and 0.97, respectively. HLA-DQA1*02:01 frequencies are relatively prevalent, estimated to be 0.13 in Whites, 0.10 in Chinese and 0.09 in African-Americans, but as low as 0.008 in Japanese.38, 77 The ethnic differences in DILI frequencies by lapatinib should be analyzed between Japanese and other populations in the future.
DILI: LUMIRACOXIB
Lumiracoxib is a selective cyclooxigenase-2 inhibitor developed for the treatment of osteoarthritis and acute pain. However, concerns about hepatotoxicity led to withdrawal from the market and development worldwide. GWAS analysis was conducted primarily on lumiracoxib-treated White patients with or without DILI following lumiracoxib treatment.78 The SNP rs9270986 in the HLA region was significantly associated with the onset of DILI in exploration (41 cases and 176 tolerant controls, OR 5.3, P=2.8 × 10−10) and replication (98 cases and 405 tolerant controls, OR 3.0, P=1.0 × 10−9) studies. In addition, a fine mapping study involving 137 cases and 577 controls revealed that the haplotype HLA-DRB1*15:01-DQB1*06:02-DRB5*01:01-DQA1*01:02 showed a strong association with DILI, with HLA-DRB1*15:01 being the most significant allele (OR=7.5, P=6.8 × 10−25). The sensitivity, specificity, PPV and NPV of HLA-DQA1*0102 were 0.736, 0.692, 0.058 and 0.99, respectively. Molecular pathogesis should be investigated in the future because the same haplotype is also associated with AC-induced DILI.
DILI: XIMELAGATRAN
Ximelagatran was developed for the prevention and treatment of thromboembolism, but was withdrawn from clinical development by DILI, where alanine aminotransferase elevation (>3 times the upper limit of normal) was observed in approximately 8% of patients who were administered the drug, with a higher incidence in Northern Europe compared with Asia.79 The risk HLA allele HLA-DRB1*07 was found in an exploration study (74 cases and tolerant 130 controls, P=9.1 × 10−6) and small-scale replication study (10 cases and tolerant 16 controls, P=6 × 10−3).80 The frequencies of HLA-DRB1*07:01 are higher in Whites (0.126) than in Japanese (0.002),38 and thus this ethnic difference might contribute to the above DILI frequencies. An in vitro peptide competition assay suggested an interaction of ximelagatran and its metabolite ethyl melagatran with HLA-DRB*07:01 proteins when present at high concentrations.
DILI: OTHER DRUGS
For anti-tuberculosis-related DILI, a significant association with HLA-DQB1*02:01 was reported in North Indian patients with tuberculosis (OR=1.9).81 HLA-DRB1*01:01 showed a tendency for association with a nevirapine-related hepatic/systemic adverse reactions in Western Australia (OR=4.8, Pc=0.14).82 This result was later confirmed in White patients (OR=3.02, Pc=0.0074).83 Valproate hepatotoxicity was significantly associated with combined SNPs (p.Q1236H and p.E1143G) of the mitochondrial DNA polymerase γ, POLG (OR=23.6, P=5.1 × 10−7).84
PATHOGENESIS OF DILI
Flucloxacillin is known to covalently bind to a lysine residue on albumin in a time-dependent manner, and the level of binding correlated directly with the stimulation of T-cell clones from flucloxacillin-related DILI patients.85, 86 Activation of CD8+ clones with flucloxacillin was process-dependent in the antigen-presenting cells, because glutaraldehyde fixation (which inhibits formation of antigenic peptides) suppressed proliferation, and was restricted by HLA-B*57:01.86 Although an associated HLA allele has not been identified, another β-lactam piperacillin-modifed albumin on a lysine residue was also shown to be processed in the antigen-presenting cells, and activated T-cell clones from piperacillin-hypersensitive patients in a HLA protein-dependent manner.87 These mechanisms for T-cell activation are different from the carbamazepine cases for SJS/TEN in that the drugs bind noncovalently to the HLA. β-lactams (flucloxacillin and piperacillin) can bind spontaneously to proteins such as albumin, and therefore numerous drug–protein conjugates may form, resulting in the processing of these modified proteins and formation of drug–peptide complexes to activate T cells via HLA proteins.
CONCLUDING REMARKS
This review summarized the current status of pharmacogenomic research on two severe ADRs, SCARs and DILI. Advances in this area have been accelerating in the last decade, but two major issues remained to be addressed. First, several HLA markers are reported to be associated with the onset of these ADRs, with relatively high sensitivity, specificity and NPV, but low PPV, suggesting that these markers are necessary but not sufficient for ADR onset, and that other genetic and/or environmental factors should exist. However, an exploratory GWAS on allopurinol for SJS/TEN, and flucloxacillin or lumiracoxib for DILI, did not reveal any genetic markers other than those in the HLA region (chromosome 6). Genome-wide sequencing could reveal rare but highly penetrant variations for the ADRs. As shown before, usage of a specific TCR repertoire may be a critical factor for development of SJS/TEN induced by carbamazepine. Other approaches such as transcriptomics, proteomics or metabolomics might contribute to the detection of relevant factors, including environmental ones. Second, the HLA alleles mainly found to be associated with ADRs are dependent on each drug, and therefore researchers should collect enough case and control samples to ensure statistical power for the detection of genetic biomarkers, both in exploratory and validation studies. However, this would be very difficult because the frequency of severe ADRs is very low, particularly for drugs with a low incidence of ADR. Intra- and international collaborations with similar ethnic populations are essential for resolving this issue. Indeed, collaborations between European and American scientists led to success in finding flucloxacillin-related HLA markers for DILI in White patients. There is no doubt that establishing an Asian or African collaborative network is needed in the very near future to achieve similar goals. Finally, in vitro mechanistic approach or even in silico approach88 would be valuable for predicting interactions between drugs and proteins and its functional consequence, and these results may lead to the generation of a short list of candidate genes.
References
Lazarou, J., Pomeranz, B. H. & Corey, P. N. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279, 1200–1205 (1998).
Morimoto, T., Sakuma, M., Matsui, K., Kuramoto, N., Toshiro, J., Murakami, J. et al. Incidence of adverse drug events and medication errors in Japan: the JADE study. J. Gen. Intern. Med. 26, 148–153 (2011).
Pirmohamed, M., Breckenridge, A. M., Kitteringham, N. R. & Park, B. K. Adverse drug reactions. BMJ 316, 1295–1298 (1998).
Bastuji-Garin, S., Rzany, B., Stern., R. S., Shear, N. H., Naldi, L. & Roujeau, J. C. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch. Dermatol. 129, 92–96 (1993).
Hashimoto, K., Iijima, M., Shiohara., T., Asahina, A., Ikezawa, Z., Nankou, H. et al. Toxic Epidermal Necrolysis - Handling Manual for Individual Severe Adverse Reactions Vol. 1 (Japan Pharmaceutical Information Center, Tokyo, 2007).
Hashimoto, K. Drug Induced Hypersensitivity Syndrome—Dermatology Practice 19, Insight into Skin Rash (Bunkoudou, Tokyo, 2006).
Saito, Y. & Sudo, C. Occurrence and causative drugs of SJS/TEN. Jpn Med. J. 4613, 60–61 (2012).
Torres, M. J., Mayorga, C. & Blanca, M. Nonimmediate allergic reactions induced by drugs: pathogenesis and diagnostic tests. J. Investig. Allergol. Clin. Immunol. 19, 80–90 (2009).
Chung, W. H., Hung, S. I., Hong, H. S., Hsih, M. S., Yang, L. C., Ho, H. C. et al. A marker for Stevens-Johnson syndrome. Nature 428, 486 (2004).
Hung, S. I., Chung, W. H., Jee, S. H., Chen, W. C., Chang, Y. T., Lee, W. R. et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet. Genomics 16, 297–306 (2006).
Man, C. B., Kwan, P., Baum, L., Yu, E., Lau, K. M., Cheng, A. S. et al. Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese. Epilepsia 48, 1015–1018 (2007).
Lonjou, C., Thomas, L., Borot, N., Ledger, N., de Toma, C., LeLouet, H. et al. A marker for Stevens-Johnson syndrome: ethnicity matters. Pharmacogenom. J. 6, 265–268 (2006).
Mehta, T. Y., Prajapati, L. M., Mittal, B., Joshi, C. G., Sheth, J. J., Patel, D. B. et al. Association of HLA-B*1502 allele and carbamazepine-induced Stevens-Johnson syndrome among Indians. Indian J. Dermatol. Venereol. Leprol. 75, 579–582 (2009).
Tassaneeyakul, W., Tiamkao, S., Jantararoungtong, T., Chen, P., Lin, S. Y., Chen, W. H. et al. Association between HLA-B*1502 and carbamazepine-induced severe cutaneous adverse drug reactions in a Thai population. Epilepsia 51, 926–930 (2010).
Wang, Q., Zhou, J. Q., Zhou, L. M., Chen, Z. Y., Fang, Z. Y., Chen, S. D. et al. Association between HLA-B*1502 allele and carbamazepine-induced severe cutaneous adverse reactions in Han people of southern China mainland. Seizure 20, 446–448 (2011).
Lim, K. S., Kwan, P. & Tan, C. T. Association of HLA-B*1502 allele and carbamazepine-induced severe adverse cutaneous drug reaction among Asians, a review. Neurol. Asia 13, 15–21 (2008).
Hung, S. I., Chung, W. H., Liu, Z. S., Chen, C. H., Hsih, M. S., Hui, R. C. et al. Common risk allele in aromatic antiepileptic-drug induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Han Chinese. Pharmacogenomics 11, 349–356 (2010).
Kaniwa, N., Sait, O. Y., Aihara, M., Matsunaga, K., Tohkin, M., Kurose, K. et al. HLA-B*1511 is a risk factor for carbamazepine-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Japanese patients. Epilepsia 51, 2461–2465 (2010).
Kim, S. H., Lee, K. W., Song, W. J., Kim, S. H., Jee, Y. K., Lee, S. M. et al. Carbamazepine-induced severe cutaneous adverse reactions and HLA genotypes in Koreans. Epilepsy Res. 97, 190–197 (2011).
Wei, C. Y., Chung, W. H., Huang, H. W., Chen, Y. T. & Hung, S. I. Direct interaction between HLA-B and carbamazepine activates T cells in patients with Stevens-Johnson syndrome. J. Allergy Clin. Immunol. 129, 1562–1569 (2012).
Kashiwagi, M., Aihara, M., Takahashi, Y., Yamazaki, E., Yamane, Y., Song, Y. et al. Human leukocyte antigen genotypes in carbamazepine-induced severe cutaneous adverse drug response in Japanese patients. J. Dermatol. 35, 683–685 (2008).
Ozeki, T., Mushiroda, T., Yowang, A., Takahashi, A., Kubo, M., Shirakara, Y. et al. Genome-wide association study identifies HLA-A*3101 allele as a genetic risk factor for carbamazepine-induced cutaneous adverse drug reactions in Japanese population. Hum. Mol. Genet. 20, 1034–1041 (2011).
Niihara, H., Kakamu, T., Fujita, Y., Kaneko, S. & Morita, E. HLA-A31 strongly associates with carbamazepine-induced adverse drug reactions but not with carbamazepine-induced lymphocyte proliferation in a Japanese population. J. Dermatol. 39, 594–601 (2012).
McCormack, M., Alfirevic, A., Bourgeois, S., Farrell, J. J., Kasperavičiūtė, D., Carrington, M. et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N. Eng. J. Med. 364, 1134–1143 (2011).
Hung, S. I., Chung, W. H., Liou, L. B., Chu, C. C., Lin, M., Huang, H. P. et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc. Natl Acad. Sci. USA 102, 4134–4139 (2005).
Tassaneeyakul, W., Jantararoungtong, T., Chen, P., Lin, P. Y., Tiamkao, S., Khunarkornsiri, U. et al. Strong association between HLA-B*5801 and allopurinol-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in a Thai population. Pharmacogenet. Genomics 19, 704–709 (2009).
Dainichi, T., Uchi, H., Moroi, Y. & Furue, M. Stevens-Johnson syndrome, drug-induced hypersensitivity syndrome and toxic epidermal necrolysis caused by allopurinol in patients with a common HLA allele: what causes the diversity? Dermatology 215, 86–88 (2007).
Kaniwa, N., Saito, Y., Aihara, M., Matsunaga, K., Tohkin, M., Kurose, K. et al. HLA-B locus in Japanese patients with anti-epileptics and allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis. Pharmacogenomics 9, 1617–1622 (2008).
Tohkin, M., Kaniwa, N., Saito, Y., Sugiyama, E., Kurose, K., Nishikawa, J. et al. A whole-genome association study of major determinants for allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis in Japanese patients. Pharmacogenomics J. 13, 60–69 (2013).
Kang, H. R., Jee, Y. K., Kim, Y. S., Lee, C. H., Jung, J. W., Kim, S. H. et al. Positive and negative associations of HLA class I alleles with allopurinol-induced SCARs in Koreans. Pharmacogenet. Genomics 21, 303–307 (2011).
Maekawa, K., Nishikawa, J., Kaniwa, N., Sugiyama, E., Koizumi, T., Kurose, K. et al. Development of a rapid and inexpensive assay for detecting a surrogate genetic polymorphism of HLA-B*58:01: a partially predictive but useful biomarker for allopurinol-related Stevens-Johnson syndrome/toxic epidermal necrolysis in Japanese. Drug Metab. Pharmacokinet 27, 447–450 (2012).
Cao, Z. H., Wei, Z. Y., Zhu, Q. Y., Zhang, J. Y., Yang, L., Qin, S. Y. et al. HLA-B*58:01 allele is associated with augmented risk for both mild and severe cutaneous adverse reactions induced by allopurinol in Han Chinese. Pharmacogenomics 13, 1193–1201 (2012).
Mallal, S., Nolan, D., Witt, C., Masel, G., Martin, A. M., Moore, C. et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet 359, 727–732 (2002).
Martin, A. M., Nolan, D., Gaudieri, S., Almeida, C. A., Nolan, R., James, I. et al. Predisposition to abacavir hypersensitivity conferred by HLA-B*5701 and a haplotypic Hsp70-Hom variant. Proc. Natl Acad. Sci. USA 101, 4180–4185 (2004).
Sadiq, S. T. & Pakianathan, M. Uncertainties of routine HLA B*5701 testing in black African HIV cohorts in the UK. Sex. Transm. Infect. 83, 181–182 (2007).
Hughes, A. R., Mosteller, M., Bansal, A. T., Davies, K., Haneline, S. A., Lai, E. H. et al. Association of genetic variations in HLA-B region with hypersensitivity to abacavir in some, but not all, populations. Pharmacogenomics 5, 203–211 (2004).
Saag, M., Balu, R., Phillips, E., Brachman, P., Martorell, C., Burman, W. et al. Study of hypersensitivity to abacavir and pharmacogenetic evaluation study team. High sensitivity of human leukocyte antigen-b*5701 as a marker for immunologically confirmed abacavir hypersensitivity in White and Black patients. Clin. Infect. Dis. 46, 1111–1118 (2008).
Gonzalez-Galarza, F. F., Christmas, S., Middleton, D. & Jones, A. R. Allele frequency net: a database and online repository for immune gene frequencies in worldwide populations. Nucleic Acid Res. 39, D913–D919 (2011).
Sun, H. Y., Hung, C. C., Lin, P. H., Chang, S. F., Yang, C. Y., Chang, S. Y. et al. Incidence of abacavir hypersensitivity and its relationship with HLA-B*5701 in HIV-infected patients in Taiwan. J. Antimicrob. Chemother. 60, 599–604 (2007).
Park, W. B., Choe, P. G., Song, K. H., Lee, S., Jang, H. C., Jeon, J. H. et al. Should HLA-B*5701 screening be performed in every ethnic group before starting abacavir? Clin. Infect. Dis. 48, 365–367 (2009).
Chantarangsu, S., Mushiroda, T., Mahasirimongkol, S., Kiertiburanakul, S., Sungkanuparph, S., Manosuthi, W. et al. HLA-B*3505 allele is a strong predictor for nevirapine-induced skin adverse drug reactions in HIV-infected Thai patients. Pharmacogenet. Genomics 19, 139–146 (2009).
Shirato, S., Kagaya, F., Suzuki, Y. & Joukou, S. Stevens-Johnson syndrome induced by methazolamide treatment. Arch. Ophthalmol. 115, 550–553 (1997).
Park, Y. J., Moon, J. I. & Park, C. K. Three cases of Stevens-Johnson syndrome associated with methazolamide treatment. J. Korean. Ophthalmol. Soc. 40, 613–618 (1999).
Sung, K. H., Jwong, Y., Choi, H. U. & Lee, S. K. Two cases of HLA-B59(+) Stevens-Johnson syndrome (SJS)-toxic epideremal necroylsis (TEN) associated with methazolamide treatment. Korean Dermatol. 43, 561–563 (2005).
Ha, J. H., Song, J. Y., Kim, H. O., Kim, C. W. & Kim, S. S. A case of Stevens-Johnson syndrome caused by acetazolamide. Korean J. Deramtol. 41, 248–250 (2003).
Her, Y., Kil, M. S., Park, J. H., Kim, C. W. & Kim, S. S. Stevens-Johnson syndrome induced by acetazolamide. J. Dermatol. 38, 272–275 (2011).
Moon, J. I., Seo, J. H. & Park, C. K. Association of HLA type with Stevens-Johnson syndrome induced by methazolamide treatment. J. Korean Ophthalmol. Soc. 41, 2241–2246 (2000).
Kim, S. H., Kim, M., Lee, K. W., Kim, S. H., Kang, H. R., Park, H. W. et al. HLA-B*5901 is strongly associated with methazolamide-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Pharmacogenomics 11, 879–884 (2011).
Li, H., Dai, Y., Huang, H., Li, L., Leng, S., Cheng, J. et al. HLA-B*1301 as a biomarker for genetic susceptibility to hypersensitivity dermatitis induced by trichloroethylene among workers in China. Environ. Health Perspect. 115, 1553–1556 (2007).
Ueta, M., Sotozono, C., Tokunaga, K., Yabe, T. & Kinoshita, S. Strong association between HLA-A*0206 and Stevens-Johnson syndrome in the Japanese. Am. J. Ophthalmol. 143, 367–368 (2007).
Ueta, M., Tokunaga, K., Sotozono, C., Inatomi, T., Yabe, T., Matsushita, M. et al. HLA class I and II gene polymorphisms in Stevens-Johnson syndrome with ocular complications in Japanese. Mol. Vis. 14, 550–555 (2008).
Mallal, S., Phillips, E., Carosi, G., Molina, J. M., Workman, C., Tomazic, J. et al. HLA-B*5701 screening for hypersensitivity to abacavir. N. Engl. J. Med. 358, 568–579 (2008).
Chen, P., Lin, J. J., Lu, C. S., Ong, C. T., Hsieh, P. F., Yang, C. C. et al. Taiwan SJS Consortium. Carbamazepine-induced toxic effects and HLA-B*1502 screening in Taiwan. N. Engl. J. Med. 364, 1126–1133 (2011).
Ko, T. M., Chung, W. H., Wei, C. Y., Shih, H. Y., Chen, J. K., Lin, C. H. et al. Shared and restricted T-cell receptor use is crucial for carbamazepine-induced Stevens-Johnson syndrome. J. Allergy Clin. Immunol. 128, 1266–1276 (2011).
Norcross, M. A., Luo, S., Lu, L., Boyne, M. T., Gomarteli, M., Rennels, A. D. et al. Abacavir induces loading of novel self-peptides into HLA-B*57: 01: an autoimmune model for HLA-associated drug hypersensitivity. AIDS 26, F21–F29 (2012).
Sgro, C., Clinard, F., Ouazir, K., Chanay, H., Allard, C., Guilleminet, C. et al. Incidence of drug-induced hepatic injuries: a French population-based study. Hepatology 36, 451–455 (2002).
Danan, G. & Benichou, C. Causality assessment of adverse reactions to drugs--I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J. Clin. Epidemiol. 46, 1323–1330 (1993).
Takikawa, H. & Onji, M. A proposal of the diagnostic scale of drug-induced liver injury. Hepatol. Res. 32, 250–251 (2005).
Andrade, R. J., Lucena, M. I., Alonso, A., García-Cortes, M., García-Ruiz, E., Benitez, R. et al. HLA class II genotype influences the type of liver injury in drug-induced idiosyncratic liver disease. Hepatology 39, 1603–1612 (2004).
Urban, T. J., Shen, Y., Stolz, A., Chalasani, N., Fontana, R. J., Rochon, J. et al. Limited contribution of common genetic variants to risk for liver injury due to a variety of drugs. Pharmacogenet. Genomics 22, 784–795 (2012).
Ikeda, T. Drug-induced idiosyncratic hepatotoxicity: prevention strategy developed after the troglitazone case. Drug Metab. Pharmacokinet. 26, 60–70 (2011).
Watanabe, I., Tomita, A., Shimizu, M., Sugawara, M., Yasumo, H., Koishi, R. et al. A study to survey susceptible genetic factors responsible for troglitazone-associated hepatotoxicity in Japanese patients with type 2 diabetes mellitus. Clin. Pharmacol. Ther. 73, 435–455 (2003).
Kurose, K., Sugiyama, E. & Saito, Y. Population differences in major functional polymorphisms of pharmacokinetics/pharmacodynamics-related genes in Eastern Asians and Europeans: implications in the clinical trials for novel drug development. Drug Metab. Pharmacokinet. 27, 9–54 (2012).
Whalen, R. & Boyer, T. D. Human glutathione S-transferases. Semin. Liver Dis. 18, 345–358 (1998).
Lucena, M. I., Andrade, R. J., Martínez, C., Ulzurrun, E., García-Martín, E., Borraz, Y. et al. Glutathione S-transferase m1 and t1 null genotypes increase susceptibility to idiosyncratic drug-induced liver injury. Hepatology 48, 588–596 (2008).
Ueda, K., Ishitsu, T., Seo, T., Ueda, N., Murata, T., Hori, M. et al. Glutathione S-transferase M1 null genotype as a risk factor for carbamazepine-induced mild hepatotoxicity. Pharmacogenomics 8, 435–442 (2007).
Cai, Y., Yi, J., Zhou, C. & Shen, X. Pharmacogenetic study of drug-metabolising enzyme polymorphisms on the risk of anti-tuberculosis drug-induced liver injury: a meta-analysis. PLoS One 7, e47769 (2012).
Mizushima, M., Iwata, N., Fujimoto, T. T., Ishikawa, K. & Fujimura, K. Patient characteristics in ticlopidine hydrochloride-induced liver injury: Case-control study. Hepatol. Res. 33, 234–240 (2005).
Hirata, K., Takagi, H., Yamamoto, M., Matsumoto, T., Nishiya, T., Mori, K. et al. Ticlopidine-induced hepatotoxicity is associated with specific human leukocyte antigen genomic subtypes in Japanese patients: a preliminary case-control study. Pharmacogenomics J. 8, 29–33 (2008).
Ariyoshi, N., Iga, Y., Hirata, K., Sato, Y., Miura, G., Ishii, I. et al. Enhanced susceptibility of HLA-mediated ticlopidine-induced idiosyncratic hepatotoxicity by CYP2B6 polymorphism in Japanese. Drug Metab. Pharmacokinet. 25, 298–306 (2010).
Hautekeete, M. L., Horsmans, Y., Van Waeyenberge, C., Demanet, C., Henrion, J., Verbist, L. et al. HLA association of amoxicillin-clavulanate--induced hepatitis. Gastroenterology 117, 1181–1186 (1999).
O'Donohue, J., Oien, K. A., Donaldson, P., Underhill, J., Clare, M., MacSween, R. N. et al. Co-amoxiclav jaundice: clinical and histological features and HLA class II association. Gut 47, 717–720 (2000).
Donaldson, P. T., Daly, A. K., Henderson, J., Graham, J., Pirmohamed, M., Bernal, W. et al. Human leukocyte antigen class II genotype in susceptibility and resistance to co-amoxiclav-induced liver injury. J. Hepatol. 53, 1049–1053 (2010).
Lucena, M. I., Molokhia, M., Shen, Y., Urban, T. J., Aithal, G. P., Andrade, R. J. et al. Susceptibility to amoxicillin-clavulanate-induced liver injury is influenced by multiple HLA class I and II alleles. Gastroenterology 141, 338–347 (2011).
Russmann, S., Kaye, J. A., Jick, S. S. & Jick, H. Risk of cholestatic liver disease associated with flucloxacillin and flucloxacillin prescribing habits in the UK: cohort study using data from the UK General Practice Research Database. Br. J. Clin. Pharmacol. 60, 76–82 (2005).
Daly, A. K., Donaldson, P. T., Bhatnagar, P., Shen, Y., Pe'er, I., Floratos, A. et al. HLA-B*5701 genotype is a major determinant of drug-induced liver injury due to flucloxacillin. Nat. Genet. 41, 816–819 (2009).
Spraggs, C. F., Budde, L. R., Briley, L. P., Bing, N., Cox, C. J., King, K. S. et al. HLA-DQA1*02:01 is a major risk factor for lapatinib-induced hepatotoxicity in women with advanced breast cancer. J. Clin. Oncol. 29, 667–673 (2011).
Singer, J. B., Lewitzky, S., Leroy, E., Yang, F., Zhao, X., Klickstein, L. et al. A genome-wide study identifies HLA alleles associated with lumiracoxib-related liver injury. Nat. Genet. 42, 711–714 (2010).
Harenberg, J., Jörg, I. & Weiss, C. Observations of alanine aminotransferase and aspartate aminotransferase in THRIVE studies treated orally with ximelagatran. Int. J. Toxicol. 25, 165–169 (2006).
Kindmark, A., Jawaid, A., Harbron, C. G., Barratt, B. J., Bengtsson, O. F., Andersson, T. B. et al. Genome-wide pharmacogenetic investigation of a hepatic adverse event without clinical signs of immunopathology suggests an underlying immune pathogenesis. Pharmacogenomics J. 8, 186–195 (2008).
Sharma, S. K., Balamurugan, A., Saha, P. K., Pandey, R. M. & Mehra, N. K. Evaluation of clinical and immunogenetic risk factors for the development of hepatotoxicity during antituberculosis treatment. Am. J. Respir. Crit. Care Med. 166, 916–919 (2002).
Martin, A. M., Nolan, D., James, I., Cameron, P., Keller, J., Moore, C. et al. Predisposition to nevirapine hypersensitivity associated with HLA-DRB1*0101 and abrogated by low CD4 T-cell counts. AIDS 19, 97–99 (2005).
Yuan, J., Guo, S., Hall, D., Cammett, A. M., Jayadev, S., Distel, M. et al. Toxicogenomics of nevirapine-associated cutaneous and hepatic adverse events among populations of African, Asian, and European descent. AIDS 25, 1271–1280 (2011).
Stewart, J. D., Horvath, R., Baruffini, E., Ferrero, I., Bulst, S., Watkins, P. B. et al. Polymerase γ gene POLG determines the risk of sodium valproate-induced liver toxicity. Hepatology 52, 1791–1796 (2010).
Jenkins, R. E., Meng, X., Elliott, V. L., Kitteringham, N. R., Pirmohamed, M. & Park, B. K. Characterisation of flucloxacillin and 5-hydroxymethyl flucloxacillin haptenated HSA in vitro and in vivo. Proteomics Clin. Appl. 3, 720–729 (2009).
Monshi, M. M., Faulkner, L., Gibson, A., Jenkins, R. E., Farrell, J., Earnshaw, C. J. et al. Human leukocyte antigen (HLA)-B*57:01-restricted activation of drug-specific T cells provides the immunological basis for flucloxacillin-induced liver injury. Hepatology 57, 727–739 (2013).
El-Ghaiesh, S., Monshi, M. M., Whitaker, P., Jenkins, R., Meng, X., Farrell, J. et al. Characterization of the antigen specificity of T-cell clones from piperacillin-hypersensitive patients with cystic fibrosis. J. Pharmacol. Exp. Ther. 341, 597–610 (2012).
Bhattacharya, S., Shoda, L. K., Zhang, Q., Woods, C. G., Howell, B. A., Siler, S. Q. et al. Modeling drug- and chemical-induced hepatotoxicity with systems biology approaches. Front. Physiol. 3, 462 (2012).
Acknowledgements
This study was supported in part by Health Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare of Japan. We thank all of the doctors and patients for their cooperation during this research study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kaniwa, N., Saito, Y. Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury. J Hum Genet 58, 317–326 (2013). https://doi.org/10.1038/jhg.2013.37
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2013.37
Keywords
This article is cited by
-
Association of HLA-DRB1*04:05 allele with drug-induced interstitial lung disease in Japanese population
The Pharmacogenomics Journal (2020)
-
Managing the challenge of drug-induced liver injury: a roadmap for the development and deployment of preclinical predictive models
Nature Reviews Drug Discovery (2020)
-
SNP-based HLA allele tagging, imputation and association with antiepileptic drug-induced cutaneous reactions in Hong Kong Han Chinese
The Pharmacogenomics Journal (2018)
-
Comparison of exome-based HLA class I genotyping tools: identification of platform-specific genotyping errors
Journal of Human Genetics (2017)
-
Association between infection and severe drug adverse reactions: an analysis using data from the Japanese Adverse Drug Event Report database
European Journal of Clinical Pharmacology (2017)