Abstract
Irinotecan is a key chemotherapeutic drug used to treat many tumors, including cervical and ovarian cancers; however, irinotecan can cause toxicity, particularly in the presence of uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) gene polymorphisms, which are associated with reduced enzyme activity. Here, we investigated the prevalence of three different variants of UGT1A1 (UGT1A1*6, UGT1A1*27 and UGT1A1*28) and their relationships with irinotecan-induced adverse events in patients with gynecologic cancer, who are treated with lower doses of irinotecan than patients with other types of solid tumors. Fifty-three female patients treated with irinotecan and 362 female patients not treated with irinotecan were screened for UGT1A1*6, UGT1A1*27 and UGT1A1*28. Homozygosity for UGT1A1*6 or heterozygosity for UGT1A1*6/*28 was associated with a high risk of severe absolute neutrophil count decrease or diarrhea (odds ratios: 16.03 and 31.33, respectively). In contrast, serum bilirubin levels were not associated with irinotecan toxicity. Homozygosity for UGT1A1*6/*6 and heterozygosity for UGT1A1*6/*28 were associated with an increased risk of absolute neutrophil count and/or diarrhea in Japanese gynecologic cancer patients, despite the lower doses of irinotecan used in these patients. UGT1A1*6 and UGT1A1*28 are potential predictors of severe absolute neutrophil decrease and diarrhea caused by low-dose irinotecan in gynecologic cancer patients.
Similar content being viewed by others
Introduction
Irinotecan is a key drug used to treat cervical and ovarian cancers; however, ∼20–35% of patients treated with irinotecan experience severe diarrhea and neutropenia.1, 2, 3, 4, 5 As a prodrug, irinotecan is activated by hydrolysis to SN-38, a potent topoisomerase I inhibitor, and inactivated through conversion to SN-38 glucuronide (SN-38G) by UDP-glucuronosyltransferase 1A1 (UGT1A1).6 Gene transcription efficiency is inversely correlated with the UGT1A1 gene polymorphism UGT1A1*28.7 Moreover, as UGT1A1 catalyzes bilirubin glucuronidation, homozygosity for the TA7 allele is associated with Gilbert’s syndrome, a common mild hyperbilirubinemia.8, 9 Three variants (UGT1A1*6, UGT1A1*27 and UGT1A1*28) are associated with reduced enzyme activity and increased irinotecan toxicity,10 and the frequencies of these variants differ between Asian and Caucasian populations.10, 11, 12, 13 These polymorphisms directly reduce UGT enzyme activity.14 UGT1A1*6 also can cause a decrease in metabolic activity and is not linked with UGT1A1*28.15, 16, 17
The U.S. Food and Drug Administration recommends that a dose reduction of irinotecan should be considered in patients homozygous for UGT1A1*28. Furthermore, because of reported ethnic differences, homozygous UGT1A1*6/*6 and UGT1A1*28/*28 genotypes and the heterozygous UGT1A1*6/*28 genotype are seen as poor metabolizers (PMs) of irinotecan. Indeed, patients with UGT1A1 deficiencies experience irinotecan-dependent neutropenia and diarrhea in a dose-dependent manner;18 however, contradictory results have been reported for the association between UGT1A1 genotypes and toxicity profiles in patients receiving low-dose irinotecan.19, 20, 21 Moreover, while some studies have suggested its association with severe neutropenia, total bilirubin is yet to be validated as a marker for predicting the risk of severe neutropenia in gynecological cancer patients treated with irinotecan in the absence of UGT1A1 genetic information.22, 23, 24, 25
To date, only a few studies have described individualized chemotherapy treatment based on the assessment of genetic polymorphisms in gynecologic cancer or on the administration of lower doses of irinotecan for the treatment of gynecologic cancer compared with the doses used for other solid tumors.19 Here, we retrospectively investigated the associations of UGT1A1 polymorphisms with serum bilirubin levels and severe adverse effects in Japanese patients who received irinotecan for the treatment of gynecologic cancer.
Patients and methods
Patients
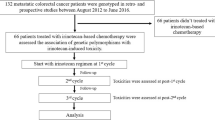
Blood samples were collected from 415 Japanese patients who visited the menopausal clinic or cancer follow-up clinic of the Department of Obstetrics and Gynecology, Keio University Hospital (Tokyo, Japan). Fifty-three patients who had cervical or ovarian cancer and received irinotecan-containing chemotherapy were retrospectively studied. An additional 362 patients who did not receive irinotecan therapy were chosen at random. Patients with pathological hyperbilirubinemia, including obstructive jaundice, and non-Japanese patients were excluded from the study. Informed consent was obtained from all patients before using their blood. The study was conducted with the approval of the ethics committee of the School of Medicine, Keio University (approval numbers: 20050135, 20060091 and 20070081).
UGT1A1 genotyping and classification
Genomic DNA was extracted by standard procedures. UGT1A1*6 (211G→A), UGT1A1*27 (686C→A) and UGT1A1*28 [(TA)6TAA→(TA)7TAA] polymorphisms were genotyped using an Invader UGT1A1 Molecular Assay kit (Third Wave Technologies, Madison, WI, USA) as previously described.26 UGT1A1 polymorphisms were classified into two groups, as recommended by the Pharmaceuticals and Medical Devices Agency, Japan (PMDA): the PM group and the extensive metabolizer (EM) group. The PM group included homozygous UGT1A1*6/*6 and UGT1A1*28/*28 genotypes and the heterozygous UGT1A1*6/*28 genotype. Patients who were not classified as PMs were assigned to the EM group.
Schedule of irinotecan treatment and evaluation of adverse events
The treatment regimen consisted of either 60 mg m−2 irinotecan on days 1, 8 and 15 and 60 mg m−2 cisplatin on day 1 every 4 weeks or 100 mg m−2 irinotecan alone on days 1, 8 and 15 every 4 weeks. Physical examinations and blood tests were retrospectively reviewed to evaluate toxicity and adverse events in irinotecan-treated patients, and their grades were assessed prospectively according to the common terminology criteria for adverse events, version 3.0.27 The monitoring period for adverse events and the worst grade after irinotecan therapy were evaluated until 6 weeks after last irinotecan administration.
Association of irinotecan toxicity with serum bilirubin and UGT1A1 genotypes
Serum total bilirubin was measured for 392 patients, including 49 patients treated with irinotecan. The highest total bilirubin value was adopted from the patient’s own personal historical data in the hospital. Bilirubin measurement was conducted prior to surgery or any chemotherapy in patients given irinotecan, because the bilirubin level may increase after irinotecan therapy. For patients in whom the total bilirubin levels were 1.4 mg dl−1 or greater, hyperbilirubinemia was diagnosed according to the normal range in the hospital. The relationships between serum bilirubin and UGT1A1 genotypes and between serum bilirubin and irinotecan toxicity were statistically analyzed.
Statistical analyses
Statistical analysis was performed with Exel2011, Microsoft Office: mac2011 (Microsoft Japan Co., Ltd., Tokyo, Japan) with the add-in software Statcel 3 (OMS, Saitama, Japan) and Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA) using the indicated tests. The F-test was used to verify the heterogeneity of variances. Nonparametrically distributed variables were assessed using the Mann–Whitney U-test. The chi-square test or Fisher’s exact test was performed for contingency tables. Results with P-values of less than 0.05 were considered significant.
Results
Patient characteristics
Blood samples from a total of 415 patients, including 11 cervical cancer patients, 107 ovarian cancer patients, 225 endometrial cancer patients, 26 ovarian and endometrial double cancer patients, 8 myoma or endometriotic cyst and 38 menopausal disorder were analyzed for UGT1A1 polymorphisms (Table 1). Among these patients, 53 were treated with irinotecan.
UGT1A1 genotype and allele frequency
Genotype and allele frequencies of UGT1A1*6, UGT1A1*27 and UGT1A1*28 in 415 patients, including 53 patients that received irinotecan and 362 without irinotecan treatment, are summarized in Supplementary Table 1.
Two patients (3.8%) treated with irinotecan were homozygous for UGT1A1*6, and none were homozygous for UGT1A1*28. Fourteen patients (26.4%) were heterozygous for UGT1A1*6, and 9 patients (17.0%) were heterozygous for UGT1A1*28. One patient was simultaneously heterozygous for UGT1A1*6 and UGT1A1*28 (data not shown). No irinotecan-treated patients were heterozygous or homozygous for UGT1A1*27.
None were homozygous for UGT1A1*27, whereas 17 (4.1%) and 7 (1.9%) patients without irinotecan treatment were homozygous for UGT1A1*6 and UGT1A1*28, respectively.
Of all cases, all UGT1A1*27 carriers also harbored UGT1A1*28 alleles (data not shown). Moreover, 14 patients (9.2%) were simultaneously heterozygous for UGT1A1*6 and UGT1A1*28 (data not shown).
UGT1A1*6 and UGT1A1*28 groups did not differ significantly between patients receiving or not receiving irinotecan (P=0.802 and 0.464, respectively).
The PM and EM groups did not differ significantly between the total patient population and irinotecan-treated patients (P=0.605; Supplementary Table 2).
Correlation between the UGT1A1 genotype and adverse effects of irinotecan
Genotypes and adverse event assessments for 53 patients (11 cervical cancer, 40 ovarian cancer and 2 ovarian and endometrial double cancer patients) who received irinotecan are summarized in Table 2.27 Thirty-five patients had grades 0–2 absolute neutrophil count, whereas 18 patients had grades 3–4 absolute neutrophil count (Table 2). In addition, 48 patients had grades 0–2 diarrhea, and 5 patients had grades 3–4 diarrhea (Table 2). The occurrence of grades 3–4 absolute neutrophil count and diarrhea was significantly more frequent in PM-group patients than in EM-group patients (odds ratio: 16.03, P=0.0348 and odds ratio: 31.33, P=0.0209, respectively). However, UGT1A1*6 or UGT1A1*28 alone was not associated with absolute neutrophil count.
Three cases in Table 3 were classified as PMs of irinotecan (the PM group). Two of these cases were homozygous for UGT1A1*6, and one was simultaneously heterozygous for UGT1A1*6 and UGT1A1*28. All three had a grade 3 or 4 absolute neutrophil count, and two had grade 3 diarrhea.
Relationship between serum bilirubin and UGT1A1 genotypes or irinotecan toxicity
Total bilirubin levels were significantly higher in the PM group (n=38) than in the EM group (n=354; P<0.0001; Figure 1). Sixty-nine out of 392 patients had been diagnosed with hyperbilirubinemia (⩾1.4 mg dl−1) more than once in their history (Table 4). The occurrence of hyperbilirubinemia was significantly increased in heterozygous or homozygous UGT1A1*28 cases compared with heterozygous or homozygous UGT1A1*6 cases. Furthermore, the occurrence of hyperbilirubinemia was significantly increased in PM-group cases compared with EM-group cases (odds ratio: 6.08, P<0.0001; Table 4). However, serum bilirubin levels were not associated with irinotecan toxicity-induced grade 3 or 4 absolute neutrophil count or diarrhea in the 49 patients who were treated with irinotecan (P>0.05 for both; Table 5).
Discussion
Previous studies have revealed ethnic differences in UGT1A1 haplotypes among Caucasians, African-Americans and Asians.7, 12, 13, 14 Conversely, UGT1A1*6 and UGT1A1*27 polymorphisms have been identified only in Asians.8, 13 Our results for the allele frequencies of UGT1A1*6, UGT1A1*27 and UGT1A1*28 are similar to those of previous reports.
A prior study demonstrates that the UGT1A1*6 genotype is related to lower SN-38 glucuronidation and a higher frequency of grade 3/4 toxicities in patients receiving irinotecan and cisplatin.28 Moreover, a grade 3/4 absolute neutrophil count is significantly more frequent in patients who have the UGT1A1*6 genotype and are undergoing irinotecan-based chemotherapy, and homozygosity for the UGT1A1*6 allele is associated with altered SN-38 disposition, potentially increasing the risk of severe neutropenia in Asian cancer patients.29 Our data could not support this theory, most likely because we did not have enough UGT1A1*6 and UGT1A1*28 cases in this study.
Since UGT1A1*27 is very rare, its clinical impact has not yet been fully elucidated. The UGT1A1*27 and UGT1A1*28 alleles are linked; therefore, UGT1A1*28 genotyping is thought to cover UGT1A1*27 carriers.30 In our study, all four UGT1A1*27 carriers also harbored UGT1A1*28 alleles. Some studies have yielded contradictory results for the relationship between UGT1A1 genotypes and toxicity profiles in patients receiving low-dose irinotecan.19, 20 For example, the risk of hematologic toxicity is strongly associated with the UGT1A1*28 genotype at higher doses (>150 mg m−2), but not at lower doses (⩽150 mg m−2).20 However, a recent meta-analysis revealed that the UGT1A1*28/*28 genotype was associated with an increased risk of neutropenia at all doses of irinotecan.21
Irinotecan is often administered as combination therapy with cisplatin for gynecologic cancer. In a previous study of 177 Japanese cancer patients treated with irinotecan as a single agent or as combination chemotherapy with cisplatin,31 significant associations between UGT1A1*6 or UGT1A1*28 and neutropenia were observed for patients in both groups. Moreover, significant associations between UGT1A1*6 or UGT1A1*28 and diarrhea were also observed for patients who received irinotecan as a single therapy, but not in patients who received combination therapy with cisplatin.31 Of the three PM patients who received irinotecan in our study, one patient was administered irinotecan as a single agent and two patients were given combination chemotherapy with cisplatin (Table 3). Thus, our results demonstrated that significant associations between UGT1A1*6 or UGT1A1*28 and low absolute neutrophil count or diarrhea occurred in Japanese ovarian cancer patients who received irinotecan as single agent or in combination with cisplatin. These findings are in agreement with those of Takano et al., who first reported that grade 3/4 neutropenia, thrombocytopenia and diarrhea were significantly more frequent in UGT1A1*6 and/or UGT1A1*28 genotypes in Japanese gynecologic cancer patients treated with the irinotecan–cisplatin combination.19 In contrast, our findings contradicted a previous report showing no significant contribution of UGT1A1 genotypes to toxicity in patients treated with low-dose irinotecan monotherapy.20 However, interpatient differences in SN-38G formation, which have been correlated with the occurrence of severe diarrhea, and the lower doses of irinotecan used in the present study may, at least in part, explain these conflicting results.32, 33
Hyperbilirubinemia may be a potential alternative predictive marker for irinotecan toxicity. Indeed, modest elevations in bilirubin (1.0–1.5 mg dl−1) are associated with increased grades 3–4 neutropenia in metastatic colorectal cancer patients treated with weekly irinotecan.22 However, baseline serum bilirubin does not reliably predict overall irinotecan-related toxicity or efficacy in these cases. Interestingly, UGT1A1 polymorphisms are associated with serum bilirubin levels, and UGT1A1*28 has been reported to be associated with Gilbert’s syndrome.8, 9 UGT1A1*6, predominant in east Asia, also leads to lower UGT1A1 expression and hyperbilirubinemia.15, 16, 17 In the current study, hyperbilirubinemia was significantly more frequent in heterozygous or homozygous UGT1A1*28 cases or PM cases (Table 4), but was not associated with irinotecan toxicity in our study (Table 5). Thus, our findings strongly suggested that UGT1A1 genotyping may be a more powerful predictive biomarker than serum bilirubin.
Our study has some limitations. Because of the sampling procedure used, the patients examined here were cancer survivors, and cases of aggressive disease were not included. In addition, UGT1A1 polymorphisms are thought to influence the development of some cancers, including colorectal, breast and ovarian cancers.34 Moreover, an individual’s response to irinotecan is unlikely to be affected by UGT1A1*28 status.35 We also did not distinguish between patients receiving irinotecan+cisplatin versus irinotecan alone; this may have affected the outcome of the study. The range of irinotecan dosages in clinical use is very wide and was determined according to organ-based therapies tested in large-scale clinical studies.21 Moreover, the metabolism of irinotecan to SN-38 and other metabolites varies widely between patients. Therefore, a wide range of doses is required, and dose modifications or variations should be based on genotyping. Further prospective studies on the pharmacokinetics, pharmacodynamics and pharmacogenetics of irinotecan are needed to clarify these findings, especially in patients receiving low-dose irinotecan, in which few clinical trials have been conducted.
In conclusion, homozygosity for UGT1A1*6/*6 and heterozygosity for both UGT1A1*6/*28 were predictive of low absolute neutrophil count and diarrhea induced by irinotecan in Japanese gynecologic cancer patients, whereas serum bilirubin levels were not.
Change history
04 December 2013
This article has been corrected since Advance Online Publication, and an erratum is also printed in this issue.
References
Rothenberg, M. L., Kuhn, J. G., Schaaf, L. J., Rodriguez, G. I., Eckhardt, S. G., Villalona-Calero, M. S. et al. Phase I dose-finding and pharmacokinetic trial of irinotecan (CPT-11) administered every two weeks. Ann. Oncol. 12, 1631–1641 (2001).
Negoro, S., Fukuoka, M., Masuda, N., Takada, M., Kusunoki, Y., Matsui, K. et al. Phase I study of weekly intravenous infusions of CPT-11, a new derivative of camptothecin, in the treatment of advanced non-small-cell lung cancer. J. Natl Cancer Inst 83, 1164–1168 (1991).
Rothenberg, M. L., Kuhn, J. G., Burris, H. A. 3rd, Nelson, J., Eckhardt, J. R., Tristan-Morales, M. et al. Phase I and pharmacokinetic trial of weekly CPT-11. J. Clin. Oncol. 11, 2194–2204 (1993).
Fuchs, C. S., Moore, M. R., Harker, G., Villa, L., Rinaldi, D. & Hecht, J. R. Phase III comparison of two irinotecan dosing regimens in second-line therapy of metastatic colorectal cancer. J. Clin. Oncol. 21, 807–814 (2003).
Vanhoefer, U., Harstrick, A., Achterrath, W., Cao, S., Seeber, S. & Rustum, Y. M. Irinotecan in the treatment of colorectal cancer: clinical overview. J. Clin. Oncol. 19, 1501–1518 (2001).
Kawato, Y., Aonuma, M., Hirota, Y., Kuga, H. & Sato, K. Intracellular roles of SN-38, a metabolite of the camptothecin derivative CPT-11, in the antitumor effect of CPT-11. Cancer Res. 51, 4187–4191 (1991).
Beutler, E., Gelbart, T. & Demina, A. Racial variability in the UDP-glucuronosyltransferase 1 (UGT1A1) promoter: a balanced polymorphism for regulation of bilirubin metabolism? Proc. Natl Acad. Sci. USA 95, 8170–8174 (1998).
Bosma, P. J., Chowdhury, J. R., Bakker, C., Gantla, S., de Boer, A., Oostra, B. A. et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N. Engl. J. Med. 333, 1171–1175 (1995).
Monaghan, G., Ryan, M., Seddon, R., Hume, R. & Burchell, B. Genetic variation in bilirubin UPD-glucuronosyltransferase gene promoter and Gilbert’s syndrome. Lancet 347, 578–581 (1996).
Ando, Y., Saka, H., Ando, M., Sawa, T., Muro, K., Ueoka, H. et al. Polymorphisms of UDP-glucuronosyltransferase gene and irinotecan toxicity: a pharmacogenetic analysis. Cancer Res. 60, 6921–6926 (2000).
Ando, Y., Chida, M., Nakayama, K., Saka, H. & Kamataki, T. The UGT1A1*28 allele is relatively rare in a Japanese population. Pharmacogenetics 8, 357–360 (1998).
Hirasawa, A., Akahane, T., Tanigawara, Y. & Aoki, D. Blood-direct InvaderPlus as a new method for genetic testing. Pers. Med. 9, 657–663 (2012).
Fujiwara, Y. & Minami, H. An overview of the recent progress in irinotecan pharmacogenetics. Pharmacogenomics 11, 391–406 (2010).
Ando, Y., Saka, H., Asai, G., Sugiura, S., Shimokata, K. & Kamataki, T. UGT1A1 genotypes and glucuronidation of SN-38, the active metabolite of irinotecan. Ann. Oncol. 9, 845–847 (1998).
Jinno, H., Tanaka-Kagawa, T., Hanioka, N., Saeki, M., Ishida, S., Nishimura, T. et al. Glucuronidation of 7-ethyl-10-hydroxycamptothecin (SN-38), an active metabolite of irinotecan (CPT-11), by human UGT1A1 variants, G71R, P229Q, and Y486D. Drug Metab. Dispos. 31, 108–113 (2003).
Gagné, J. F., Montminy, V., Belanger, P., Journault, K., Gaucher, G. & Guillemette, C. Common human UGT1A polymorphisms and the altered metabolism of irinotecan active metabolite 7-ethyl-10-hydroxycamptothecin (SN-38). Mol. Pharmacol. 62, 608–617 (2002).
Yamamoto, K., Sato, H., Fujiyama, Y., Doida, Y. & Bamba, T. Contribution of two missense mutations (G71R and Y486D) of the bilirubin UDP glycosyltransferase (UGT1A1) gene to phenotypes of Gilbert's syndrome and Crigler-Najjar syndrome type II. Biochim. Biophys. Acta 1406, 267–273 (1998).
Marsh, S. & Hoskins, J. M. Irinotecan pharmacogenomics. Pharmacogenomics 11, 1003–1010 (2010).
Takano, M., Kato, M., Yoshikawa, T., Sasaki, N., Hirata, J., Furuya, K. et al. Clinical significance of UDP-glucuronosyltransferase 1A1*6 for toxicities of combination chemotherapy with irinotecan and cisplatin in gynecologic cancers: a prospective multi-institutional study. Oncology 76, 315–321 (2009).
Hoskins, J. M., Goldberg, R. M., Qu, P., Ibrahim, J. G. & McLeod, H. L. UGT1A1*28 genotype and irinotecan-induced neutropenia: dose matters. J. Natl Cancer Inst. 99, 1290–1295 (2007).
Hu, Z. Y., Yu, Q., Pei, Q. & Guo, C. Dose-dependent association between UGT1A1*28 genotype and irinotecan-induced neutropenia: low doses also increase risk. Clin. Cancer Res. 16, 3832–3842 (2010).
Meyerhardt, J. A., Kwok, A., Ratain, M. J., McGovren, J. P. & Fuchs, C. S. Relationship of baseline serum bilirubin to efficacy and toxicity of single-agent irinotecan in patients with metastatic colorectal cancer. J. Clin. Oncol. 22, 1439–1446 (2004).
Innocenti, F., Undevia, S. D., Iyer, L., Chen, P. X., Das, S., Kocherginsky, M. et al. Genetic variants in the UDP-glucuronosyltransferase 1A1 gene predict the risk of severe neutropenia of irinotecan. J. Clin. Oncol. 22, 1382–1388 (2004).
Ramchandani, R. P., Wang, Y., Booth, B. P., Ibrahim, A., Johnson, J. R., Rahman, A. et al. The role of SN-38 exposure, UGT1A1*28 polymorphism, and baseline bilirubin level in predicting severe irinotecan toxicity. J. Clin. Pharmacol. 47, 78–86 (2007).
Freyer, G., Rougier, P., Bugat, R., Droz, J. P., Marty, M., Bleiberg, H. et al. Prognostic factors for tumour response, progression-free survival and toxicity in metastatic colorectal cancer patients given irinotecan (CPT-11) as second-line chemotherapy after 5FU failure: CPT-11 F205, F220, F221 and V222 study groups. Br. J. Cancer 83, 431–437 (2000).
Hasegawa, Y., Sarashina, T., Ando, M., Kitagawa, C., Mori, A., Yoneyama, M. et al. Rapid detection of UGT1A1 gene polymorphisms by newly developed Invader assay. Clin. Chem. 50, 1479–1480 (2004).
Common terminology criteria for adverse events, version 3.0, 2006. [Cited 23 June 2013.] Available at: (http://ctep.cancer.gov/reporting/ctc_v30.html).
Han, J. Y., Lim, H. S., Shin, E. S., Yoo, Y. K., Park, Y. H., Lee, J. E. et al. Comprehensive analysis of UGT1A polymorphisms predictive for pharmacokinetics and treatment outcome in patients with non-small-cell lung cancer treated with irinotecan and cisplatin. J. Clin. Oncol. 24, 2237–2244 (2006).
Jada, S. R., Lim, R., Wong, C. I., Shu, X., Lee, S. C., Zhou, Q. et al. Role of UGT1A1*6, UGT1A1*28 and ABCG2 c.421C>A polymorphisms in irinotecan-induced neutropenia in Asian cancer patients. Cancer Sci. 98, 1461–1467 (2007).
Sai, K., Saeki, M., Saito, Y., Ozawa, S., Katori, N., Jinno, H. et al. UGT1A1 haplotypes associated with reduced glucuronidation and increased serum bilirubin in irinotecan-administered Japanese patients with cancer. Clin. Pharmacol. Ther. 75, 501–515 (2004).
Minami, H., Sai, K., Saeki, M., Saito, Y., Ozawa, S., Suzuki, K. et al. Irinotecan pharmacokinetics/pharmacodynamics and UGT1A genetic polymorphisms in Japanese: roles of UGT1A1*6 and *28. Pharmacogenet. Genomics 17, 497–504 (2007).
Gupta, E., Lestingi, T. M., Mick, R., Ramirez, J., Vokes, E. E. & Ratain, M. J. Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res. 54, 3723–3725 (1994).
Gupta, E., Mick, R., Ramirez, J., Wang, X., Lestingi, T. M., Vokes, E. E. et al. Pharmacokinetic and pharmacodynamic evaluation of the topoisomerase inhibitor irinotecan in cancer patients. J. Clin. Oncol. 15, 1502–1510 (1997).
Strassburg, C. P. Pharmacogenetics of Gilbert’s syndrome. Pharmacogenomics 9, 703–715 (2008).
Dias, M. M., McKinnon, R. A. & Sorich, M. J. Impact of the UGT1A1*28 allele on response to irinotecan: a systematic review and meta-analysis. Pharmacogenomics 13, 889–899 (2012).
Acknowledgements
This work was supported in part by the Foundation for the Promotion of Cancer Research in Japan (2009–2011). The authors thank the patients for participating in this study. We also thank the assistant medical staff for their help, Mr Hideki Naganishi for his practical support and Ms Keiko Abe and Ms Tomomi Noda for their administrative assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Hirasawa, A., Zama, T., Akahane, T. et al. Polymorphisms in the UGT1A1 gene predict adverse effects of irinotecan in the treatment of gynecologic cancer in Japanese patients. J Hum Genet 58, 794–798 (2013). https://doi.org/10.1038/jhg.2013.105
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2013.105
Keywords
This article is cited by
-
UGT1A1 polymorphism has a prognostic effect in patients with stage IB or II uterine cervical cancer and one or no metastatic pelvic nodes receiving irinotecan chemotherapy: a retrospective study
BMC Cancer (2020)
-
Comparison of effects of UGT1A1*6 and UGT1A1*28 on irinotecan-induced adverse reactions in the Japanese population: analysis of the Biobank Japan Project
Journal of Human Genetics (2019)
-
Combination chemotherapy with irinotecan and gemcitabine for taxane/platinum-resistant/refractory ovarian and primary peritoneal cancer: a multicenter phase I/II trial (GOGO-Ov 6)
Cancer Chemotherapy and Pharmacology (2017)