Abstract
There is strong evidence for a negative association between schizophrenia and rheumatoid arthritis (RA). However, the mechanism for this association is unknown. We hypothesize that these two diseases share susceptibility genes. Recently, extensive studies have identified some RA susceptibility genes, including NFKBIL1, SLC22A4, RUNX1, FCRL3 and PADI4, in the Japanese population. To assess whether polymorphisms in these RA susceptibility genes are implicated in vulnerability to schizophrenia, we conducted a two-stage case–control association study in Japanese subjects. In a screening population of 534 patients and 559 control subjects, we examined eight polymorphisms in RA susceptibility genes and found a potential association of padi4_94 in PADI4 with schizophrenia. However, we could not replicate this association in a confirmatory population of 2126 patients and 2228 control subjects. The results of this study suggest that these polymorphisms in RA susceptibility genes do not contribute to genetic susceptibility to schizophrenia.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic mental disorder and rheumatoid arthritis (RA) is a chronic inflammatory disease. Both diseases affect approximately 1% of the world population. There is strong evidence for a negative association between schizophrenia and RA, implying low comorbidity of these disorders.1, 2, 3 However, the mechanism for this association is unknown. Genetic epidemiological studies including family, twin and adoption studies have shown that genetic factors play important roles in the pathogeneses of these two diseases.4 Interestingly, major histocompatibility complex (MHC), class II, DR β 1 (HLA-DRB1) is associated with both schizophrenia5, 6, 7 and RA.8, 9 These findings led us to hypothesize that these two diseases share susceptibility genes.
Recently, extensive studies have identified some RA susceptibility genes in the Japanese population. The study by Okamoto et al.10 identified a second RA susceptibility locus within the MHC region of the short arm of chromosome 6 as the T allele at position −61 in the promoter region of nuclear factor of κ light polypeptide gene enhancer in B-cells inhibitor-like 1 (NFKBIL1). The study by Tokuhiro et al.11 reported an association between slc2F2, an intronic single-nucleotide polymorphism (SNP) in a Runt-related transcription factor 1 (RUNX1) binding site of solute carrier family 22, member 4 (SLC22A4) on the 5q31 cytokine cluster region and RA. In that study, an SNP (runx1) of RUNX1 on 21q22.3 was also associated with RA. Kochi et al.12 showed an association of a functional SNP at position −169 (fcrh3_3) in the promoter region of Fc receptor-like 3 (FCRL3) on 1q21–23 with RA. This SNP altered the binding affinity for nuclear factor-κB and regulated the expression of FCRL3 mRNA. The study by Suzuki et al.13 found that the haplotype of peptidylarginine deiminase type IV (PADI4) on 1p36, which affects the stability of transcripts, was associated with RA. A recent meta-analysis revealed associations of PADI4, FCRL3 and SLC22A4 with RA in East Asian populations.14 To assess whether these polymorphisms of RA susceptibility genes are implicated in vulnerability to schizophrenia, we performed a two-stage case–control association study in Japanese subjects.
Materials and methods
Subjects
This study was approved by the Ethics Committee of each participating institute, and written informed consent was obtained from each participant. All the participants were unrelated Japanese subjects. The screening population consisted of 534 patients with schizophrenia (281 men and 253 women; mean age, 40.1 (s.d. 14.2) years) and 559 control subjects (297 men and 262 women; mean age, 37.3 (s.d. 10.1) years). The confirmatory population consisted of 2126 patients with schizophrenia (1137 men and 989 women; mean age, 47.3 (s.d. 14.3) years) and 2228 control subjects (1189 women and 1039 men; mean age, 46.6 (s.d. 13.9) years). The patients were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) criteria consensus of at least two experienced psychiatrists on the basis of all available sources of information, including unstructured interviews, clinical observations and medical records. The control subjects were mentally healthy subjects with no self-reported history of psychiatric disorders who showed good social and occupational skills, although they were not assessed by a structured psychiatric interview.
Genotyping
Genomic DNA was extracted from peripheral blood using a standard phenol/chloroform method. We examined eight polymorphisms in five RA susceptibility genes. We included the SNPs that showed the strongest associations in the original studies, namely T-62A (rs2071592) in NFKBIL1,10 slc2F1 (rs2073838) in SLC22A4,11 runx1 (rs2268277) in RUNX1,11 fcrh3_3 (rs7528684) in FCRL312 and padi4_94 (rs2240340) in PADI4.13 We also examined slc2F2 (rs3792876), which was found to affect the transcriptional efficiency of SLC22A4.11 For PADI4, we genotyped two additional SNPs (padi4_104 (rs1748033) and padi4_102 (rs2240337)) because Ikari et al.15 indicated that padi4_94, padi4_104 and padi4_102 allowed them to describe the four haplotypes detected in the original study.
All the SNPs were genotyped using a TaqMan 5′-exonuclease assay as described earlier.16
Statistical analysis
Deviation from the Hardy–Weinberg equilibrium (HWE) was tested using the χ2 test. Pair-wise linkage disequilibrium (LD) indices (D′ and r2) and haplotype frequencies were determined using Haploview v4.0.17 Genotypic associations were examined using the χ2 test or Fisher’s exact test. The allele and haplotype frequencies of the patients and control subjects were compared using the χ2 test. A probability level of P<0.05 was considered to indicate statistical significance.
A power calculation was performed using Genetic Power Calculator.18 The power was estimated with an α of 0.05, assuming that the disease prevalence was 0.01 and the risk allele frequencies were the values observed in control samples.
Results
We genotyped eight SNPs in RA susceptibility genes in a screening population (Table 1). The genotype distributions of these SNPs did not deviate significantly from the HWE in both groups. We found a potential association between padi4_94 and schizophrenia (allelic uncorrected P=0.047).
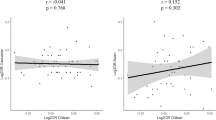
Two SNPs (slc2F2 and slc2F1) in SLC22A4 were in strong LD (D′=0.99; r2=0.97) and three SNPs (padi4_94, padi4_104 and padi4_102) in PADI4 were in LD (D′=0.80–1; r2=0.09–0.82). The degree of LD between the two SNPs in SLC22A4 was very similar to that of the HapMap data (D′=1; r2=1). The degree of LD between the three SNPs in PADI4 was higher than that of the HapMap data (D′=0.37–1; r2=0.01–0.96), but very similar to that found in a previous study (D′=0.76–1).15 Next, we performed haplotype analyses of SLC22A4 and PADI4 in the screening population (Table 2). There were no significant differences in the haplotype frequencies of SLC22A4 and PADI4 between the two groups.
To confirm the potential association between padi4_94 and schizophrenia, we examined this SNP in a confirmatory population (Table 3). However, we were unable to replicate this association. We were also unable to find this association in a combined population comprising the screening and confirmatory populations.
Discussion
In our two-stage case–control study, we found no associations of eight polymorphisms in RA susceptibility genes with schizophrenia in the Japanese population. Although there was a marginally significant association between padi4_94 and schizophrenia in the screening population, this association could not be replicated in the confirmatory population. The positive association observed in the screening population was probably because of a type I error. It is unlikely that the negative results in the confirmatory and combined populations were due to type II errors because the power calculation showed that, when the genotypic relative risk was set at 1.3 for homozygous risk allele carriers under the multiplicative model of inheritance, the power was more than 0.80 in the confirmatory population.
To the best of our knowledge, the RA susceptibility genes examined in this study have not been tested for their associations with schizophrenia, with the exception of NFKBIL1. NFKBIL1 is located on 6p21.3 where a genome scan meta-analysis has suggested a locus of susceptibility to schizophrenia.19 The study by Shirt et al.20 investigated 26 SNPs covering a 100-kb region centered on D6S2672, including two SNPs in NFKBIL1. These two SNPs in NFKBIL1 were not associated with schizophrenia in their Caucasian samples of 236 patients and 240 control subjects. The study by Morar et al.21 analyzed 36 SNPs in a 165-kb region around tumor necrosis factor, including five SNPs in NFKBIL1. There were no significant associations of these five SNPs in NFKBIL1 with schizophrenia in their sample of 204 families (79 sib-pairs and 125 trios). In this study, we did not find an association between T-62A in NFKBIL1 and schizophrenia in our Japanese samples of 534 patients and 559 control subjects. Our results are in line with the negative findings reported in the previous studies.20, 21 To draw a definitive conclusion that NFKBIL1 does not contribute to genetic susceptibility to schizophrenia, however, further studies using larger sample sizes and sufficient markers are required in different ethnic populations.
We recognize several limitations of this study. First, we investigated only eight SNPs in five RA susceptibility genes. Overall, 10, 4, 15, 7 and 14 tagging SNPs for NFKBIL1, SLC22A4, RUNX1, FCRL3 and PADI4, respectively, covering these RA susceptibility gene regions and the 5′ and 3′ flanking regions were selected from the HapMap database (release #23a; population: Japanese in Tokyo; minor allele frequency: more than 0.05). We applied the criterion of an r2 threshold greater than 0.8 in the ‘aggressive tagging: use 2- and 3-marker haplotype’ mode using the ‘Tagger’ program22 as implemented in Haploview v4.0,17 and all polymorphisms examined, with the exception of runx 1, were forced to be selected as tagging SNPs. Therefore, our results cannot exclude the possible contributions of other polymorphisms in these RA susceptibility genes to the pathogenesis of schizophrenia. Second, the sample size of the screening population was moderate. The power calculation showed that when the genotypic relative risk was set at 1.69 for homozygous risk allele carriers under the multiplicative model of inheritance, the power was more than 0.80 for seven of the examined SNPs, but only 0.43 for padi4_102. Therefore, we could not exclude the possibility that our negative results in the screening population, especially for padi4_102, were because of type II errors. Third, no standardized structured interview was applied to verify the clinical diagnoses of the enrolled patients, but the diagnosis of schizophrenia was assigned on the basis of all available sources of information. The control samples were not well characterized. We cannot exclude the possibility that our control samples may have contained some younger individuals who will suffer from schizophrenia later in life. To the best of our knowledge, however, there were no control subjects who were likely to develop schizophrenia at their present stage of life. Thus it is unlikely that our failure to find a significant association is attributable to misdiagnosis. Fourth, substantial differences in the susceptibility genes to RA exist between Caucasian and Japanese populations. A missense SNP (R620W) in protein tyrosine phosphatase non-receptor type 22 (PTPN22) was associated with RA in a Caucasian population,23 whereas R620W was not polymorphic in a Japanese population.24 If R620W in PTPN22 explains the negative association between schizophrenia and RA, an association of R620W with schizophrenia should only be observed in Caucasian populations, although such association studies have not been conducted. In this study, therefore, we evaluated polymorphisms in RA susceptibility genes identified in the Japanese population. However, there are no solid epidemiological data to support a negative association between schizophrenia and RA in the Japanese population. Thus our strategy based on this negative association may not be effective.
In conclusion, this study suggests that the eight polymorphisms in RA susceptibility genes examined do not contribute to genetic susceptibility to schizophrenia in the Japanese population.
References
Mors, O., Mortensen, P. B. & Ewald, H. A population-based register study of the association between schizophrenia and rheumatoid arthritis. Schizophr. Res. 40, 67–74 (1999).
Oken, R. J. & Schulzer, M. At issue: schizophrenia and rheumatoid arthritis: the negative association revisited. Schizophr. Bull 25, 625–638 (1999).
Leucht, S., Burkard, T., Henderson, J., Maj, M. & Sartorius, N. Physical illness and schizophrenia: a review of the literature. Acta. Psychiatr. Scand. 116, 317–333 (2007).
Torrey, E. F. & Yolken, R. H. The schizophrenia-rheumatoid arthritis connection: infectious, immune, or both? Brain Behav. Immun. 15, 401–410 (2001).
Arinami, T., Otsuka, Y., Hamaguchi, H., Itokawa, M., Aoki, J., Shibuya, H. et al. Evidence supporting an association between the DRB1 gene and schizophrenia in Japanese. Schizophr. Res. 32, 81–86 (1998).
Sasaki, T., Matsushita, M., Nanko, S., Fukuda, R., Kennedy, J. L. & Tokunaga, K. Schizophrenia and the HLA-DRB1 gene in the Japanese population. Am. J. Psychiatry 156, 771–773 (1999).
Akaho, R., Matsushita, I., Narita, K., Okazaki, Y., Okabe, Y., Matsushita, M. et al. Support for an association between HLA-DR1 and schizophrenia in the Japanese population. Am. J. Med. Genet. (Neuropsychiatr. Genet.) 96, 725–727 (2000).
Wakitani, S., Murata, N., Toda, Y., Ogawa, R., Kaneshige, T., Nishimura, Y. et al. The relationship between HLA-DRB1 alleles and disease subsets of rheumatoid arthritis in Japanese. Br. J. Rheumatol. 36, 630–636 (1997).
Kochi, Y., Yamada, R., Kobayashi, K., Takahashi, A., Suzuki, A., Sekine, A. et al. Analysis of single-nucleotide polymorphisms in Japanese rheumatoid arthritis patients shows additional susceptibility markers besides the classic shared epitope susceptibility sequences. Arthritis. Rheum. 50, 63–71 (2004).
Okamoto, K., Makino, S., Yoshikawa, Y., Takaki, A., Nagatsuka, Y., Ota, M. et al. Identification of IkBL as the second major histocompatibility complex-linked susceptibility locus for rheumatoid arthritis. Am. J. Hum. Genet. 72, 303–312 (2003).
Tokuhiro, S., Yamada, R., Chang, X., Suzuki, A., Kochi, Y., Sawada, T. et al. An intronic SNP in a RUNX1 binding site of SLC22A4, encoding an organic cation transporter, is associated with rheumatoid arthritis. Nat. Genet. 35, 341–348 (2003).
Kochi, Y., Yamada, R., Suzuki, A., Harley, J. B., Shirasawa, S., Sawada, T. et al. A functional variant in FcRH3, encoding Fc receptor homolog 3, is associated with rheumatoid arthritis and several autoimmunities. Nat. Genet. 37, 478–485 (2005).
Suzuki, A., Yamada, R., Chang, X., Tokuhiro, S., Sawada, T., Suzuki, M. et al. Functional haplotypes of PADI4, encoding citrullinating enzyme peptidylarginine deiminase 4, are associated with rheumatoid arthritis. Nat. Genet. 34, 395–402 (2003).
Takata, Y., Inoue, H., Sato, A., Tsugawa, K., Miyatake, K., Hamada, D. et al. Replication of reported genetic associations of PADI4, FCRL3, SLC22A4 and RUNX1 genes with rheumatoid arthritis: results of an independent Japanese population and evidence from meta-analysis of East Asian studies. J. Hum. Genet. 53, 163–173 (2008).
Ikari, K., Kuwahara, M., Nakamura, T., Momohara, S., Hara, M., Yamada, H. et al. Association between PADI4 and rheumatoid arthritis: a replication study. Arthritis. Rheum. 52, 3054–3057 (2005).
Watanabe, Y., Muratake, T., Kaneko, N., Nunokawa, A. & Someya, T. No association between the brain-derived neurotrophic factor gene and schizophrenia in a Japanese population. Schizophr. Res. 84, 29–35 (2006).
Barrett, J. C., Fry, B., Maller, J. & Daly, M. J. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21, 263–265 (2005).
Purcell, S., Cherny, S. S. & Sham, P. C. Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 19, 149–150 (2003).
Lewis, C. M., Levinson, D. F., Wise, L. H., DeLisi, L. E., Straub, R. E., Hovatta, I. et al. Genome scan meta-analysis of schizophrenia and bipolar disorder, part II: schizophrenia. Am. J. Hum. Genet. 73, 34–48 (2003).
Shirts, B. H., Kim, J. J., Reich, S., Dickerson, F. B., Yolken, R. H., Devlin, B. et al. Polymorphisms in MICB are associated with human herpes virus seropositivity and schizophrenia risk. Schizophr. Res. 94, 342–353 (2007).
Morar, B., Schwab, S. G., Albus, M., Maier, W., Lerer, B. & Wildenauer, D. B. Evaluation of association of SNPs in the TNF alpha gene region with schizophrenia. Am. J. Med. Genet. B Neuropsychiatr. Genet. 144B, 318–324 (2007).
de Bakker, P. I., Yelensky, R., Pe’er, I., Gabriel, S. B., Daly, M. J. & Altshuler, D. Efficiency and power in genetic association studies. Nat. Genet. 37, 1217–1223 (2005).
Begovich, A. B., Carlton, V. E., Honigberg, L. A., Schrodi, S. J., Chokkalingam, A. P., Alexander, H. C. et al. A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am. J. Hum. Genet. 75, 330–337 (2004).
Mori, M., Yamada, R., Kobayashi, K., Kawaida, R. & Yamamoto, K. Ethnic differences in allele frequency of autoimmune-disease-associated SNPs. J. Hum. Genet. 50, 264–266 (2005).
Acknowledgements
We thank the patients, their families and the healthy volunteers for their participation. This work was supported by a grant for the Promotion of Niigata University Research Projects (to YW).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watanabe, Y., Nunokawa, A., Kaneko, N. et al. Two-stage case–control association study of polymorphisms in rheumatoid arthritis susceptibility genes with schizophrenia. J Hum Genet 54, 62–65 (2009). https://doi.org/10.1038/jhg.2008.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2008.4
Keywords
This article is cited by
-
Meta-analysis of SLC22A4 and RUNX1 polymorphisms
Zeitschrift für Rheumatologie (2015)
-
An epidemiologic and clinical overview of medical and psychopathological comorbidities in major psychoses
European Archives of Psychiatry and Clinical Neuroscience (2011)
-
A two-stage case–control association study of PADI2 with schizophrenia
Journal of Human Genetics (2009)