Abstract
The purpose of this study is to comprehensively evaluate potential functional polymorphisms in the P21 gene in relation to the risk of lung cancer. We first determined the frequencies of P21 polymorphisms in 27 healthy Koreans, and then examined three polymorphisms (−2266G > A, S31R, and IVS2 + 16G > C), based on their frequencies and haplotype-tagging status, in a case–control study. Individuals with at least one −2266A allele were at a significantly decreased risk of lung cancer compared with those harboring the −2266 GG genotype [adjusted odds ratio (OR) = 0.71, 95% confidence interval (CI) = 0.53–0.95, P = 0.02). The haplotypes (ht2–4) carrying 31R or IVS2 + 16C alleles were associated with a significantly decreased risk of lung cancer compared with the haplotype 31S/IVS2 + 16G, which carried wild-type alleles at both loci (adjusted OR = 0.65, 95% CI = 0.50–0.83, P = 0.007)]. When the −2266A allele and ht2–4 were considered to be protective alleles, the risk of lung cancer decreased in a dose-dependent manner as the number of protective alleles increased (P = 0.0002). These results suggest that a combined analysis of these three P21 polymorphisms might better predict the risk of lung cancer than the analysis of a single polymorphism.
Similar content being viewed by others
Introduction
Regulation of the cell cycle is critical for normal growth and differentiation, and its disruption can lead to tumor growth and progression (Hartwell and Kastan 1994). Cyclin-dependent kinases (CDKs) form complexes with cyclins and control the progression of the cell cycle, whereas cyclin-dependent kinase inhibitors (CKIs) inhibit the kinase activities of the complexes and block cell cycle transition (Graña and Reddy 1995; Sherr and Roberts 1999). Thus far, two groups of CKIs have been identified. The CIP/KIP family of CKIs, including the p21WAF1/CIP1, p27KIP1, and p57KIP2, inhibits a variety of CDKs, such as cyclin D-, E-, and A-dependent kinases. The other group of CKIs (named inhibitors of CDK4, INK4), including p16INK4a, p15INK4b, p18INK4c, and p19INK4d, specifically inhibit cyclin D-dependent kinases CDK4 and CDK6 (el-Deiry et al. 1993; Xiong et al. 1993; Graña and Reddy 1995; Sherr and Roberts 1999).
P21 is induced by wild-type p53 protein in response to DNA damage, leading to either cell cycle arrest in the G1 checkpoint or apoptosis (el-Deiry et al. 1993, 1994; Xiong et al. 1993; Polyak et al. 1996). The p21 protein can suppress tumor growth by inhibiting nuclear antigen-dependent DNA replication in proliferating cells (Li et al. 1994; Waga et al. 1994). In addition, several studies have observed that the p21 protein was down-regulated in various human cancers, including lung cancer, and its expression level in cancers was associated with prognosis (Caputi et al. 1998; Pruneri et al. 1999; Shoji et al. 2002; Na et al. 2007). Thus, polymorphisms in the P21 gene may result in the alteration of p21 expression and/or activity, thereby, modulating susceptibility to cancer.
Several studies have examined the effects of P21 polymorphisms on the risk of lung cancer, but the results have been inconsistent (Sjalander et al. 1996; Shih et al. 2000; Su et al. 2003; Popanda et al. 2007). In addition, most studies have focused on the S31R (C98A in exon 2, rs1801270) polymorphism. Recently, it has been demonstrated that −2266G > A (rs4135234), at 5 bp upstream from the p53 binding site, and −1022G > A (rs762623), in the putative binding site of the E2F transcription factor, both increase p21 expression (Kong et al. 2007). Therefore, a case–control study in a Korean population was performed to further verify the role of P21 polymorphisms on the risk of lung cancer. Among the P21 polymorphisms deposited in the public database (http://www.ncbi.nlm.nih.gov/SNP) were captured six polymorphisms [−2266G < A, −2101C > A (at 160 bp upstream for the p53 binding site, rs3829963), −1022G > A, S31R, IVS2 + 16G > C (rs3176352), and *20C > T (the nucleotide 3′ of the translation termination codon was denoted by *1 (den Dunnen and Antonarakis 2001), rs1059234); Fig. 1a] with > 10% frequencies that were located in the promoter, exons (leading to an amino acid change), intron–exon junctions, or the 3′UTR. The frequencies and linkage disequilibrium (LD) status of the six single nucleotide polymorphisms (SNPs) were then examined in 27 healthy Koreans. Finally, three SNPs (−2266G > A, S31R, and IVS2 + 16G > C) were selected for a case–control study based on their frequency and LD status.
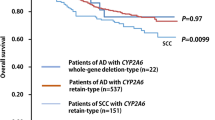
Gene map, polymorphisms, and linkage disequilibrium (LD) coefficients. A Gene map and polymorphisms in the P21 gene on chromosome 6p21.2. Coding exons are marked by black blocks and 5′- and 3′-UTRs by white blocks. The first base of transcription start site is denoted as +1 (reference genomic sequence NT_007592). B LD blocks between P21 polymorphisms in 27 healthy Koreans (a) and the subjects (n = 1,082) of a case–control study (b). The LD blocks were generated by the Haploview program using the method proposed by Gabriel et al. (2002). The black boxes indicate complete LD (|D′| = 1.0 and r 2 = 1.0). The dark gray boxes indicate strong evidence of LD [confidence interval (CI) minima for strong LD: upper 0.98, low 0.7; fraction of strong LD in informative comparisons must be at least 0.95]. The white boxes indicate strong recombination (upper CI ≤ 0.9) and the gray boxes indicate uninformative findings. The triangles indicate haplotype blocks. The numbers in the squares are |D′| (×100) values
Materials and methods
Study population
This case–control study included 549 lung cancer patients and 533 healthy controls. The method used for subject enrollment was the same as previously described (Park et al. 2006a, 2006b). In brief, eligible cases included all patients who were newly diagnosed with primary lung cancer between January 2001 and May 2002 at Kyungpook National University Hospital, Daegu, Korea. There were no age, gender, histological, or stage restrictions, but patients with a prior history of cancer were excluded from this study. The cases included 256 (46.6%) squamous cell carcinomas, 191 (34.8%) adenocarcinomas, 93 (16.9%) small cell carcinomas, and 9 (1.6%) large cell carcinomas. The control subjects were randomly selected from a pool of healthy volunteers who visited the general health check-up center at Kyungpook National University Hospital during the same period. The control subjects were matched (1:1) to the cancer cases based on gender and age (±5 years). All of the cases and controls were ethnic Koreans who resided in Daegu City or the surrounding regions. This study was approved by the institutional review board of the Kyungpook National University Hospital, and written informed consent was obtained from each participant.
Genotyping
We first determined the frequencies of P21 polymorphisms in 27 healthy Koreans by direct sequencing. The primer sets used for sequencing were designed based on the GenBank reference sequence (accession no. NT_007592). Table 1 shows the primer sequences and annealing temperature for the polymerase chain reaction (PCR) analysis. Sequence variations were confirmed by two authors independently. Among six SNPs, three SNPs (−2266G > A, S31R, and IVS2 + 16G > C) were selected for large-scale genotyping based on their frequencies and LD status.
The genotypes of the three P21 polymorphisms were determined by PCR and melting-curve analysis using fluorescence-labeled hybridization probes (LightCycler 480®, Roche Diagnostic, Mannheim, Germany). Table 2 shows the primer sequences and hybridization probes. A genotype success rate of more than 98% was achieved using the LightCycler. Samples that could not be scored using the LightCycler were re-genotyped by direct sequencing using an ABI PRISM 3700 genetic analyzer (Applied Biosystems). Genotyping analyses were performed “blind” with respect to the case/control status to ensure quality control. Approximately 10% of the samples were randomly selected to be genotyped again by a different investigator, and the results were 100% concordant. Information regarding all SNPs, SNP IDs, and allele frequencies was obtained from the NCBI homepage. In the reference sequence, the transcription start site was counted as +1.
Statistical analysis
The cases and controls were compared using Student’s t-test for continuous variables and a χ2 test for categorical variables. The Hardy–Weinberg equilibrium was tested using a goodness-of-fit χ2 test with one degree of freedom, as implemented through SAS Genetics. The LD between pairs of polymorphisms was measured as D′ and γ2 by HaploView (http://broad.mit.edu/mpg/haploview). LD blocks were inferred from the definition proposed by Gabriel et al. (2002). Haplotypes and their frequencies were estimated based on a Bayesian algorithm using the Phase program (Stephen et al. 2001). Unconditional logistic regression analysis was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs), with adjustment for possible confounders (age and pack-years of smoking as continuous variables). In addition to the overall association analysis, we performed a stratified analysis by age (median age), gender, and tumor histology to further explore the association between P21 genotypes/haplotypes and the risk of lung cancer in each stratum. The interaction between genotype and smoking was tested with both a logistic regression model that included the interaction term between genotype and smoking (smoking status, pack-years of smoking, or smoking exposure level), and by stratification analysis. For these analyses, smokers in the case and control groups were categorized into two subgroups according to the median pack-year value: lighter smokers (≤39 pack-years) and heavier smokers (>39 pack-years). The homogeneity test was performed to compare the difference between the genotype-related ORs of different groups. All of the analyses were performed using Statistical Analysis Software for Windows, version 8.12 (SAS Institute, Gary, NC, USA).
Results
The variant allele frequencies of the P21 −2266G < A, −2101C > A, −1022G > A, S31R, IVS2 + 16G > C, and *20C > T polymorphisms in 27 healthy Koreans were 0.130, 0.519, 0.130, 0.519, 0.370, and 0.519, respectively. The −2266G > A and −1022G > A, as well as the −2101C > A, S31R, and *20C > T, polymorphisms were in complete LD, respectively (Fig. 1b). Thus, the −2266G > A, S31R, and IVS2 + 16G > C polymorphisms were chosen for the association study.
Table 3 shows the demographics of the cases and controls enrolled in the study. There were no significant differences in the mean age or gender distribution between cases and controls. However, there were more current smokers among the cases than the controls (P < 0.001), and the number of pack-years in smokers was significantly higher in the cases than in the controls (40.0±17.5 vs. 34.0±17.8 pack-years; P < 0.001). These differences were controlled in the later multivariate analyses.
The genotype and polymorphic allele frequencies of the P21 −2266G > A, S31R, and IVS2 + 16G > C polymorphisms in the cases and controls are shown in Table 4. The genotype distributions of the four polymorphisms among the controls were in Hardy–Weinberg equilibrium. The frequency of the variant A allele at −2266G > A was significantly lower in the cases than in the controls (0.107 vs. 0.142, P = 0.01). Individuals with at least one −2266A allele were at a significantly decreased risk of lung cancer compared with those harboring the −2266 GG genotype (adjusted OR = 0.71, 95% CI = 0.53–0.95, P = 0.02). The risk of lung cancer decreased in a dose-dependent manner as the number of −2266A alleles increased (P Trend = 0.01). For the P21 S31R and IVS2 + 16G > C polymorphisms, individuals with at least one 31R and IVS2 + 16C allele had a borderline significantly decreased risk of lung cancer compared to carriers with the homozygous wild-type allele (adjusted OR = 0.77, 95% CI = 0.59–1.01, P = 0.06; and adjusted OR = 0.79, 95% CI = 0.61–1.01, P = 0.06, respectively).
Among the three P21 polymorphisms, the S31R and IVS2 + 16G > C were in strong LD (Fig. 1b). Thus, we examined the association between the haplotypes of the S31R and IVS2 + 16G > C polymorphisms and the risk of lung cancer. The distribution of the inferred haplotypes among the cases was significantly different from the controls (P = 0.03, Table 4). Consistent with the results of the genotyping analyses, haplotype 2 (ht2, 31S/IVS2 + 16C) and ht3 (31R/IVS2 + 16G), carrying one variant allele at the S31R or IVS2 + 16G > C, were associated with a significantly decreased risk of lung cancer compared with ht1 (31S/IVS2 + 16G) carrying wild-type alleles at both loci (adjusted OR = 0.64, 95% CI = 0.49–0.84, P = 0.001; and adjusted OR = 0.65, 95% CI = 0.50–0.85, P = 0.002, respectively). In addition, the risk of lung cancer decreased in a dose-dependent manner as the number of variant alleles increased (P Trend = 0.009). When ht2, ht3, and ht4, carrying one or two variant alleles at the two loci, were combined as one group (ht2–4) and compared with ht1, the combined ht2–4 was associated with a significantly decreased risk of lung cancer (adjusted OR = 0.65, 95% CI = 0.50–0.83, P = 0.007).
We next examined the combined effects of the three P21 polymorphisms on the risk of lung cancer. Because the −2266A allele and ht2–4 were protective against lung cancer, we considered the −2266A and ht2–4 as protective alleles, and then evaluated their combined effects by grouping the subjects based on the number of protective alleles that each subject possessed. The number of subjects with zero or four protective alleles was small (the number of subjects with zero alleles: 16 in the cases and 7 in the controls; and the number of subjects with four alleles: 9 in the cases and 15 in the controls), the subjects were grouped into three groups; subjects with 0–1 (group 1), 2 (group 2), or 3–4 (group 3) protective alleles. The frequency distribution of the combined genotypes in the cases significantly differed from that in the controls (P = 0.002, Table 5). Compared with group 1, the risk of lung cancer decreased in a dose-dependent manner as the number of protective alleles increased (adjusted OR = 0.60, 95% CI = 0.44–0.82, P = 0.001 for group 2; and adjusted OR = 0.48, 95% CI = 0.33–0.71, P = 0.0002 for group 3; P Trend = 0.0002).
It is possible that P21 polymorphisms may have different effects on the lung cancer risk according to the histological type because the different histological types of lung cancer are distinct diseases with different etiologies and carcinogenesis pathways. Therefore, stratification analysis was performed to determine if P21 polymorphisms may have differential effects on the risk of lung cancer according to the tumor histology. The protective effect of the −2266A allele and ht2–4 on the risk of lung cancer was observed for the three major histological types of lung cancer (Table 5).
We assessed the potential interaction between the P21 polymorphisms and smoking by both the logistic regression model, including the interaction term between genotype/combined genotype and smoking, and by stratification analysis. The interaction term between genotype/combined genotype and smoking was not statistically significant. There was no clear evidence that smoking modified the effect of genotype on lung cancer risk in the stratified analysis (data not shown).
Discussion
Although several studies have evaluated the association between P21 polymorphisms and the risk of lung cancer, most studies have focused on the S31R polymorphism, and the results are inconsistent. To comprehensively study potentially functional variants in the P21 gene, we first determined the frequencies and haplotype-tagging status of six P21 polymorphisms in 27 healthy Koreans, and then examined three polymorphisms (−2266G > A, S31R, and IVS2 + 16G > C) in a case–control study. We found the first evidence that the P21 −2266G > A polymorphism significantly contributes to the risk of lung cancer. In addition, we found that, when the P21 −2266G > A polymorphism was combined with the P21 S31R and IVS2 + 16G > C polymorphisms, the statistical power for the prediction of lung cancer risk increased.
A novel finding of the present study was that individuals with the P21 −2266 GA or AA genotype were at a significantly decreased risk of lung cancer compared to carriers of the −2266 GG genotype. The mechanism underlying the association between the −2266G > A polymorphism and lung cancer risk remains to be elucidated. However, because the −2266G > A polymorphism is located in the vicinity of the p53 binding site, the −2266 G-to-A change might increase the binding affinity of p53, and, thus, enhance P21 expression. This explanation is in agreement with the previous report (Kong et al. 2007), in which individuals carrying the −2266 GA or AA genotype had higher p21 mRNA expression than carriers with the −2266 GG genotype. Another possible explanation is that the observed effect of the −2266G > A polymorphism on the risk of lung cancer may be secondary to LD with other functional P21 variants. In the present study, the −2266G > A polymorphism was completely linked with the −1022G > A polymorphism. Because the −1022G > A polymorphism is located in a putative E2F binding site, which is a strong transcription factor of P21 (Hiyama et al. 1998), this polymorphism may influence the binding affinity of E2F and modify P21 expression levels.
The P21 S31R polymorphism may alter the function of p21 protein because it is located in the DNA-binding zinc finger motif of the gene, and the *20C > T polymorphism in the 3′UTR can alter mRNA stability, thereby, affecting p21 protein expression level. Based on the potential functional significance of the S31R and *20C > T polymorphisms, these two polymorphisms, alone or in combination, have been studied in many cancer types, including lung cancer, but the results are inconsistent (Sjalander et al. 1996; Shih et al. 2000; Roh et al. 2001, 2004; Su et al. 2003; Wu et al. 2003; Popanda et al. 2007). Some studies have noted that the 31R allele was associated with a significantly decreased risk of cervical, esophageal, endometrial, and lung cancers (Roh et al. 2001, 2004; Wu et al. 2003; Popanda et al. 2007). In contrast, however, Kibel et al. (2003) and Huang et al. (2004) found that the 31R allele was associated with a significantly increased risk of prostate cancer. Li et al. (2005) also reported that the 31R and *20T alleles additively increase the risk of squamous cell carcinoma of the head and neck. Moreover, several studies found no significant association of the P21 S31R polymorphism with the risk of several types of cancers (Shih et al. 2000; Su et al. 2003; Lai et al. 2005). There are several possible explanations for these differences. First, different ethnicities were examined in the studies. The variant allele frequency of the P21 S31R polymorphism is significantly different between Asian (0.408–0.571, Roh et al. 2001; Wu et al. 2003; Huang et al. 2004; Lai et al. 2005) and Caucasian (0.063–0.074, Li et al. 2005; Popanda et al. 2007) populations. Therefore, the genetic effect of the P21 S31R polymorphism on the susceptibility to human cancer may be different in different ethnic populations. Second, different molecular mechanisms may underlie different cancers. In addition, inadequate study design, such as nonrandom sampling, limited sample size, and the pitfalls arising from unknown confounders, should also be considered.
In this study, the −2266A allele was associated with a 29% reduced risk of lung cancer compared to the −2266 GG genotype, and ht2–4 was associated with a 35% reduced risk of lung cancer compared to ht1. When the −2266G > A polymorphism and S31R/IVS2 + 16G > C haplotypes were combined, the risk of lung cancer decreased in a dose-dependent manner as the number of protective alleles increased, and the presence of three or four protective alleles was associated with a 52% reduction of lung cancer risk compared to the presence of none or one protective allele. These results indicate that the protective alleles, −2266A and ht2–4, additively decrease the risk of lung cancer. In addition, this finding indicates that a combination of the −2266G > A polymorphism and the S31R/IVS2 + 16G > C haplotype is superior in predicting the risk of lung cancer compared with an analysis of a single polymorphism.
There were a number of possible limitations of this study. Since this study was a hospital-based case–control study, there might have been some selection bias. Given that most lung cancer patients are treated at a University Hospital in Korea, the demographics and clinical characteristics of the cancer patients in this study were compatible with those of a nationwide lung cancer survey (Lee et al. 2000). Furthermore, because all of the lung cancer patients who were diagnosed at the University Hospital were included in this study, it is reasonable to assume that the case group represents the lung cancer cases in the community. Another selection bias may have been derived from the controls who did not participate in this study. However, self-selection bias is unlikely because the general demographics and smoking exposure information of the non-participating controls were similar to those of the participating controls. By matching the control subjects to the cancer cases according to age and gender, the potential confounding factors might be minimized. An inadequacy in matching on smoking exposure would be controlled in data analysis with an additional adjustment. There might have been some information bias. First, the disease status may have been misclassified, but this is unlikely because all of the cases were pathologically confirmed. Second, genotypes may be misclassified by using the LightCycler. Again, the possibility of genotype misclassification is unlikely because the genotypes were confirmed by direct sequencing analyses. Third, exposure may be misclassified because of recall bias between the cases and controls during the interview. However, the cases and controls were interviewed in the same manner and the questionnaires were rechecked by randomly re-interviewing 10% of the subjects, which generated similar results. Finally, this study was designed to evaluate the effects of P21 polymorphisms on the risk of overall lung cancer. Hence, the stratification analyses according to age, gender, smoking status, and tumor histology might have a type I error (due to multiple comparisons) and/or a type II error (due to the small number of subjects in the subgroups). Therefore, additional studies with larger sample sizes will be needed to confirm our findings.
In conclusion, we found that the P21 −2266G > A polymorphism was associated with the risk of lung cancer. In addition, we demonstrated an additive effect of P21 −2266G > A, S31R, and IVS2 + 16G > C polymorphisms on the risk of lung cancer. However, because this is the first study of the P21 −2266G > A polymorphism in relation to human cancer, additional studies with larger sample sizes are required to confirm our findings. Moreover, because the genetic polymorphisms often vary between different ethnic groups, further studies are needed to clarify the association of the P21 polymorphisms, particularly −2266G > A, with the risk of lung cancer in diverse ethnic populations.
References
Caputi M, Esposito V, Baldi A, De Luca A, Dean C, Signoriello G, Baldi F, Giordano A (1998) P21waf1/cip1mda-6 expression in non-small-cell lung cancer: relationship to survival. Am J Respir Cell Mol Biol 18:213–217
den Dunnen JT, Antonarakis E (2001) Nomenclature for the description of human sequence variations. Hum Genet 109:121–124
el-Deiry WS, Tokino T, Velculescu VE, Levy DB, Parsons R, Trent JM, Lin D, Mercer WE, Kinzler KW, Vogelstein B (1993) WAF1, a potential mediator of p53 tumor suppression. Cell 75:817–825
el-Deiry WS, Harper JW, O’Conner PM, Velculescu VE, Canman CE, Jackman J, Pietenpol JA, Burrell M, Hill DE, Wang Y et al (1994) WAF1/CIP1 is induced in p53-mediated G1 arrest and apoptosis. Cancer Res 54:1169–1174
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D (2002) The structure of haplotype blocks in the human genome. Science 296:2225–2229
Graña X, Reddy EP (1995) Cell cycle control in mammalian cells: role of cyclins, cyclin dependent kinases (CDKs), growth suppressor genes and cyclin-dependent kinase inhibitors (CKIs). Oncogene 11:211–219
Hartwell LH, Kastan MB (1994) Cell cycle control and cancer. Science 266:1821–1828
Hiyama H, Iavarone A, Reeves SA (1998) Regulation of the cdk inhibitor p21 gene during cell cycle progression is under the control of the transcription factor E2F. Oncogene 16:1513–1523
Huang SP, Wu WJ, Chang WS, Wu MT, Chen YY, Chen YJ, Yu CC, Wu TT, Lee YH, Huang JK, Hunag CH (2004) p53 codon 72 and p21 codon 31 polymorphisms in prostate cancer. Cancer Epidemiol Biomarkers Prev 13:2217–2224
Kibel AS, Suarez BK, Belani J, Oh J, Webster R, Brophy-Ebbers M, Guo C, Catalona WJ, Picus J, Goodfellow PJ (2003) CDKN1A and CDKN1B polymorphisms and risk of advanced prostate carcinoma. Cancer Res 63:2033–2036
Kong EK, Chong WP, Wong WHS, Lau CS, Chan TM, Ng PKM, Song YQ, Mak W, Lau YL (2007) p21 gene polymorphisms in systemic lupus erythematosus. Rheumatol 46:220–226
Lai KC, Chen WC, Jeng LB, Li SY, Chou MC, Tsai FJ (2005) Association of genetic polymorphisms of MK, IL-4, p16, p21, p53 genes and human gastric cancer in Taiwan. Eur J Cancer Surg 31:1135–1140
Lee CT, Kang KH, Koh Y, Chang J, Chung HS, Park SK, Yoo KY, Song JS (2000) Characteristics of lung cancer in Korea, 1997. Lung Cancer 30:15–22
Li R, Waga S, Hannon GJ, Beach D, Stillman B (1994) Differential effects by the p21 CDK inhibitor on PCNA-dependent DNA replication and repair. Nature 371:534–537
Li G, Liu Z, Sturgis EM, Shi Q, Chamberlain RM, Spitz MR, Wei Q (2005) Genetic polymorphisms of p21 are associated with risk of squamous cell carcinoma of the head and neck. Carcinogenesis 26:1596–1602
Na II, Rho JK, Choi YJ, Kim CH, Park JH, Koh JS, Ryoo BY, Yang SH, Lee JC (2007) The survival outcomes of patients with resected non-small cell lung cancer differ according to EGFR mutations and the P21 expression. Lung Cancer 57:96–102
Park JY, Park JM, Jang JS, Choi JE, Kim KM, Cha SI, Kim CH, Kang YM, Lee WK, Kam S, Park RW, Kim IS, Lee JT, Jung TH (2006a) Caspase 9 promoter polymorphisms and risk of primary lung cancer. Hum Mol Genet 15:1963–1971
Park SH, Choi JE, Kim EJ, Jang JS, Lee WK, Cha SI, Kim CH, Kam S, Kim DS, Park RW, Kim YC, Han SB, Jung TH, Park JY (2006b) Polymorphisms in the FAS and FASL genes and risk of lung cancer in a Korean population. Lung Cancer 54:303–308
Polyak K, Waldman T, He TC, Kinzler KW, Vogelstein B (1996) Genetic determinants of p53-induced apoptosis and growth arrest. Genes Dev 10:1945–1952
Popanda O, Edler L, Waas P, Schattenberg T, Butkiewicz D, Muley T, Dienemann H, Risch A, Bartsch H, Schmezer P (2007) Elevated risk of squamous-cell carcinoma of the lung in heavy smokers carrying the variant alleles of the TP53 Arg72Pro and p21 Ser31Arg polymorphisms. Lung Cancer 55:25–34
Pruneri G, Pignataro L, Carboni N, Buffa R, Di Finizio D, Cesana BM, Neri A (1999) Clinical relevance of expression of the CIP/KIP cell-cycle inhibitors p21 and p27 in laryngeal cancer. J Clin Oncol 17:3150–3159
Roh JW, Kim MH, Kim JW, Park NH, Song YS, Kang SB, Lee HP (2001) Polymorphisms in codon 31 of p21 and cervical cancer susceptibility in Korean women. Cancer Lett 165:59–62
Roh JW, Kim JW, Park NH, Song YS, Park IA, Park SY, Kang SB, Lee HP (2004) p53 and p21 genetic polymorphisms and susceptibility to endometrial cancer. Gynecol Oncol 93:499–505
Sherr CJ, Roberts JM (1999) CDK inhibitors: positive and negative regulators of G-phase progression. Genes Dev 13:1501–1512
Shih CM, Lin PT, Wang HC, Huang WC, Wang YC (2000) Lack of evidence of association of p21WAF1/CIP1 polymorphism with lung cancer susceptibility and prognosis in Taiwan. Jpn J Cancer Res 91:9–15
Shoji T, Tanaka F, Takata T, Yanagihara K, Otake Y, Hanaoka N, Miyahara R, Nakagawa T, Kawano Y, Ishikawa S, Katakura H, Wada H (2002) Clinical significance of p21 expression in non-small-cell lung cancer. J Clin Oncol 18:3865–3871
Sjalander A, Birgander R, Rannug A, Alexandrie AK, Tornling G, Beckman G (1996) Association between the p21 codon 31 A1 (arg) allele and lung cancer. Hum Hered 46:221–225
Stephens M, Smith NJ, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Su L, Liu G, Zhou W, Xu LL, Miller DP, Park S, Lynch TJ, Wain JC, Christiani DC (2003) No association between the p21 codon 31 serine-arginine polymorphism and lung cancer risk. Cancer Epidemiol Biomarkers Prev 12:174–175
Waga S, Hannon GJ, Beach D, Stillman B (1994) The p21 inhibitor of cyclin-dependent kinases controls DNA replication by interaction with PCNA. Nature 369:574–578
Wu MT, Wu DC, Hsu HK, Kao EL, Yang CH, Lee JM (2003) Association between p21 codon 31 polymorphism and esophageal cancer risk in a Taiwanese population. Cancer Lett 201:175–180
Xiong Y, Hannon GJ, Zhang H, Casso D, Kobayashi R, Beach D (1993) p21 is a universal inhibitor of cyclin kinase. Nature 366:701–704
Acknowledgments
This study is supported in part by a grant from the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (grant no. 0720550-2), and in part by the Brain Korea 21 Project in 2006.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, Y.Y., Kang, HK., Choi, J.E. et al. Comprehensive assessment of P21 polymorphisms and lung cancer risk. J Hum Genet 53, 87–95 (2008). https://doi.org/10.1007/s10038-007-0222-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-007-0222-6
Keywords
This article is cited by
-
Polymorphism at codon 31 of CDKN1A (p21) as a predictive factor for bevacizumab therapy in glioblastoma multiforme
BMC Cancer (2023)
-
Single nucleotide polymorphisms and the risk of developing a second primary cancer among head and neck cancer patients: a systematic literature review and meta-analysis
BMC Cancer (2021)
-
Association between p21 Ser31Arg polymorphism and the development of cervical lesion in women infected with high risk HPV
Tumor Biology (2016)
-
p53 polymorphisms: cancer implications
Nature Reviews Cancer (2009)