Abstract
NAD(P)H oxidase is one of the most important sources of reactive oxygen species and has been demonstrated to be upregulated by angiotensin II in the kidney. Given the effect of angiotensin-converting enzyme inhibitors on the progression of both diabetic and non-diabetic renal disease, we hypothesized that the polymorphisms of NAD(P)H oxidase are associated with development of end-stage renal disease (ESRD). We examined five polymorphisms in the CYBA gene encoding the p22 phox component of NAD(P)H oxidase, including 242C/T and 640A/G polymorphisms in 467 ESRD patients and 490 healthy individuals. The T allele of the 242C/T polymorphism showed a protective effect against ESRD only in the nondiabetic (non-DM) group (P=0.0095), and haplotype estimation revealed that the frequency of 242C–640A was higher in the non-DM group (46.7%) than in the control group (39.7%). The CC–AA genotype was still significantly associated with ESRD without diabetes after adjusting for confounding factors (P=0.035). In contrast, there was no difference between the DM group and the control group. In conclusion, we identified a risk haplotype for nondiabetic ESRD in the CYBA gene using haplotype analysis. Haplotype analysis proved useful for elucidating the genetic contribution of NAD(P)H oxidase p22 phox to ESRD.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is classifiable as a multifactorial disease because the accumulation and combination of genetic factors and environmental factors influence the onset and development to end-stage renal disease (ESRD) of CKD. Although CKD results from various pathogeneses including glomerulonephritis, diabetes, lupus nephritis, interstitial nephritis, and hypertensive renal damage, the most predictive factor for progression to ESRD is not the etiology of glomerular injury, but the degree of proteinuria and the tubulointerstitial damage (Remuzzi and Bertani 1998). Therefore, there are presumably certain common pathways to ESRD regardless of their pathogenesis, such as the direct damage by massive urinary proteins and chronic ischemia resulting from fibrosis in the tubulointerstitium, and both genetic and environmental factors appear to be responsible for these common pathways. Oxidative stress is one of the major features of ESRD because a high concentration of lipid peroxidation products and advanced glycated end-products are found in ESRD patients (Miyata et al 2000; Papanastasiou et al 1994). However, it has not been clearly shown whether oxidative stress exacerbates renal damage in patients with chronic renal failure.
The NAD(P)H oxidase is a multicomponent complex that catalyzes the production of superoxide anion (O −2 ). It has a heterodimer membrane component that consists of a large glycoprotein gp91 phox, a small protein p22 phox and the cytosolic components p47 phox, p67 phox, p40 phox, and Rac. The p22 phox subunit serves as a docking site for the cytosolic phox proteins. NAD(P)H oxidase has been found not only in phagocytic cells, but also in nonphagocytic cells such as vascular smooth muscle cells (Ushio-Fukai et al 1996), renal mesangial cells (Jones et al 1995), and renal tubular cells (Hannken et al 1998). The upregulation of NAD(P)H oxidase has been demonstrated in a chronic renal failure model (Vaziri et al 2003). NAD(P)H oxidase is also upregulated by angiotensin II in afferent arterioles of glomerulus (Wang et al 2003) and renal proximal tubular cells (Hannken et al 1998). The effects of angiotensin-converting enzyme (ACE) inhibitors have been demonstrated in both diabetic and nondiabetic renal diseases by large-scale clinical trials (Jafar et al 2001; Lewis et al 1993; Ruggenenti et al 1999) and ACE inhibitors are thought to have a renoprotective effect by ameliorating intraglomerular hypertension and reducing the degree of proteinuria as well as blood pressure. However, the precise physiological mechanisms have not been revealed yet. Given the regulation of NAD(P)H oxidase by angiotensin II, we hypothesized that NAD(P)H oxidase activity is associated with development to ESRD.
There are two important polymorphisms in the CYBA gene encoding the p22 phox which have been reported to show associations with coronary artery disease (CAD) (Gardemann et al 1999; Inoue et al 1998) and carotid atherosclerosis (Hayaishi-Okano et al 2003); namely 242C/T and 640A/G polymorphisms. The 242C/T polymorphism substitutes histidine-72 with tyrosine and is thought to be essential to superoxide production (Guzik et al 2000), whereas the 640A/G polymorphism is located in the 3′ untranslated region (3′ UTR). However, significant associations have been observed in a limited number of case–control studies (Gardemann et al 1999; Hayaishi-Okano et al 2003; Inoue et al 1998).
In the present study, we performed a case–control association study for not only these two polymorphisms, 242C/T and 640A/G, but for three other polymorphisms, two of which are located in the promotor region (−930A/G and −852C/G) and one of which is in the splice site of intron 3 (IVS3+8T/C). The −930A/G polymorphism was reported to be associated with higher promotor activity (Moreno et al 2003). In addition to our analysis of the link between disease and the polymorphisms, we performed haplotype estimation and examined possible interactions among the polymorphisms.
Materials and methods
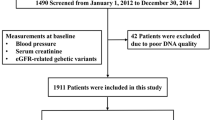
Study population
Four hundred sixty-seven patients with ESRD who were treated with hemodialysis at five dialysis centers in Tokyo area were enrolled in this study. The causes of ESRD were chronic glomerulonephritis (n=221), diabetic nephropathy (n=130), nephrosclerosis (n=64), and miscellaneous other conditions such as lupus nephritis and interstitial nephritis (n=52). Patients of ESRD caused by polycystic kidney disease and other congenital disorders were excluded. The ESRD patients were divided into two subgroups: those derived from diabetic nephropathy (DM group) and without it (non-DM group). The control group consisted of 490 unrelated healthy individuals who had medical check-ups at a health center in Tokyo area. All of the individuals in the control group were healthy, and did not show urinary abnormality, renal dysfunction, hyperglycemia, nor take any medication. There were statistical differences between the ESRD group and the control group with respect to age (63.2±12.8 [mean ± SD] years in the ESRD group versus 33.1±4.6 years in the control group) and gender (male-to-female ratio, 2.01:1 in the ESRD group vs 4.00:1 in the control group). This study was approved by the Ethics Committee for Human Genome Study in the University of Tokyo, and informed consent was obtained from each individual at the time of recruitment.
Genotyping of polymorphisms
Genomic DNAs were extracted from peripheral blood leukocytes by FlexiGene (Qiagen, Hilden, Germany) following the manufacturer’s protocol. We have established a high-throughput and accurate single nucleotide polymorphism (SNP) typing system by fluorescent capillary electrophoresis single-strand conformation polymorphism (CE-SSCP) analysis (Doi et al 2004). A system composed of a multicapillary DNA analyzer (ABI PRISM 3100; Applied Biosystems, Foster City, CA, USA), a newly developed sieving matrix (Conformation Analysis Polymer; Applied Biosystems), and four different colors of fluorescent labels (6-FAM, VIC, NED, and PET) enabled rapid and highly reliable SNP typing.
Briefly, four polymerase chain reaction (PCR) amplifications with fluorescent labeled primers were performed, and each PCR fragment was denatured to single-strand DNA in formamide before electrophoresis. Capillary electrophoretic runs with a multicapillary DNA analyzer (ABI PRISM 3100; Applied Biosystems) show a distinct peak for each allele because SNPs cause conformational changes in single-strand DNA molecules resulting in detectable mobility differences. The primers, the annealing temperatures, and fluorescent labels are listed in Table 1. Optimal temperatures for the electrophoresis were determined by preliminary runs using DNA samples from 16 unrelated individuals, which had previously been typed for all of the SNPs by direct sequencing. The results were analyzed using DNA analysis software (GeneScan and Genotyper, Applied Biosytems).
Using CE-SSCP analysis, we found a novel −852C/G polymorphism in the p22 phox promoter in addition to the −930A/G polymorphism described by Moreno et al (2003). The PCR fragments which contained both −852C/G and −930A/G polymorphisms showed specific peak location patterns according to the combination of each haplotype in capillary electrophoresis (data not shown). Therefore, CE-SSCP analysis could distinguish −852 and −930 haplotypes simultaneously.
Statistical analyses
The chi-square (χ2) test was used to compare the frequencies of the polymorphisms between the study groups. Conformity of the genotype proportion to the Hardy–Weinberg equilibrium was examined in the patient group and the control group. Linkage disequilibrium between polymorphisms was examined by calculating Lewontin’s D′ (Lewontin 1964), and the frequencies of haplotypes were estimated on the basis of a maximum-likelihood method with an expectation-maximization algorithm (Excoffier and Slatkin 1995). Permutation-based hypothesis testing (permutation test) procedures were performed to examine associations of estimated haplotype frequencies with ESRD (Fallin et al 2001). The χ2 statistics were derived from a series of simple m×n tables based on the frequency of each estimated haplotype. The null distribution of χ2 test statistics was then approximated via a randomization test in which case–control status indicators were randomly permuted among the individuals in the sample and the χ2 statistics recomputed. The P value of the permutation test was empirically determined by the ratio of the data sets above the null χ2 statistics for 10,000 permutations. These calculations were performed using a commercial program (SNPAlyze Ver3.2 Pro; Dynacom, Chiba, Japan). Logistic regression analysis and Mann–Whitney U-test were performed using StatView-J5.0 (Abacus Concepts, Berkeley, CA, USA) to adjust for confounding factors and compare durations of dialysis treatment respectively. A P value of <0.05 was considered significant.
Results
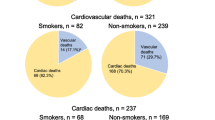
The frequencies of genotypes in the patient group and the healthy controls did not differ significantly from those expected under Hardy–Weinberg equilibrium. Table 2 shows the distribution of genotypes for the five polymorphisms in p22 phox. The T allele carrier of the 242C/T polymorphism was significantly decreased in ESRD patients compared with the healthy controls (15.8 vs 21.0%, P=0.039; odds ratio (OR), 1.41; 95% confidence interval (CI), 1.02–1.97). Subgroup analysis revealed that an association of the 242C/T polymorphism with ESRD due to diabetic nephropathy (DM group) was not found. On the other hand, a more significant association was found in patients without diabetic nephropathy (non-DM group) compared with the healthy controls (13.9 vs 21.0%, P=0.0095; OR, 1.64; 95% CI, 1.13–2.39). There was no significant association for the other polymorphisms.
Haplotype analysis revealed that the frequencies of the haplotypes estimated for all five polymorphisms in the groups were close to each other and did not show any significant difference by permutation test (Table 3). Considering that the 242C/T polymorphism showed a significant association, we performed haplotype analysis on the 242C/T and neighboring polymorphisms. As shown in Table 4, three common haplotypes were presumed for the 242C/T and 640A/G polymorphisms. The C allele of the 242C/T polymorphism was preferably found with the G allele of the 640A/G polymorphism, whereas the 242T allele was found with the 640A allele. The 242C–640G haplotype was most frequent in the control group and the DM group. In contrast, the 242C–640A haplotype was more frequent than the 242C–640G haplotype in the non-DM group. That was consistent with the finding that the index of linkage disequilibrium (Lewontin’s D′) between 242C/T and 640A/G in the non-DM group was smaller than those in the control and the DM groups. The permutation test showed a significant association of the overall haplotype frequency profiles with ESRD in the non-DM group (P=0.010 based on 10,000 permutations). At the same time, haplotype analysis on the 242C/T and the IVS3+8T/C did not show any significant difference (data not shown). These results indicate that the primary susceptibility factors for ESRD might be localized around the 242C/T polymorphism in exon 4 and the 640A/G polymorphism in exon 6.
The distribution of the 242CC–640AA genotype was significantly more frequent in the non-DM group than in the control group, and showed a strong association (P=0.0022; OR, 1.68; 95% CI, 1.20–2.35). On the other hand, the 242TT–640GG genotype did not show any significant difference between the non-DM group and the control group. These observations indicated that the 242C–640A haplotype might be a recessive risk haplotype for ESRD. A logistic regression analysis incorporating the 242CC–640AA genotype, age and gender was performed because there were differences between the patients and healthy controls with respect to age and gender. Even after adjusting for confounding factors, a significant association of 242CC–640AA genotype with ESRD without diabetes was still demonstrated (Table 5; P=0.035; OR, 2.43; 95% CI, 1.07–5.55).
Finally, we examined the relationship between the 242CC–640AA genotype and duration of dialysis treatment because this risk genotype might be responsible for CAD, which is often a complication with ESRD patients and can contribute to their deaths. There was no difference in duration of dialysis treatment between the 242CC–640AA genotype carriers and the others (242CC–640AA: 105.2±80.1 months vs the others: 94.5±73.7 months, P=0.26) and no tendency for a decrease in the frequency of the 242CC–640AA genotype according to the duration of dialysis treatment (Table 6).
Discussion
We performed a large-scale case-control association study consisting of a total of 957 cases and control samples to elucidate the polymorphisms in the CYBA gene encoding NAD(P)H p22 phox and their possible role as predisposing factors for progression of ESRD. Although only one polymorphism (242C/T) showed a significant association with the non-DM group, haplotype estimation and linkage disequilibrium analysis enabled us to find different distributions of the haplotypes with 242C/T and 640A/G polymorphisms among the study groups and identify a strong association of the 242CC–640AA genotype with the non-DM group even after adjusting for confounding factors.
Recently certain common pathways have been proposed to exist for the progression of CKD to ESRD regardless of the pathogenesis of CKD. In spite of the diversity of pathogenesis, proteinuria and interstitial fibrosis are common features of renal injury and the only predisposing factors for development of ESRD (Remuzzi and Bertani 1998). Considering the confirmed data that ACE inhibitors have protective effects against the progression of CKD which includes heterogeneous pathogenesis, and that NAD(P)H oxidase is upregulated by angiotensin II in the kidney, our data possibly indicate that genetic polymorphisms of NAD(P)H oxidase contribute to the progression of CKD to ESRD rather than the onset of CKD. Further studies such as a prospective cohort study are required to confirm the association of NAD(P)H oxidase genetic polymorphisms with the progression of CKD to ESRD.
We could not detect any significant association in the DM group, although NAD(P)H oxidase is thought to play an important role in diabetic nephropathy (Li and Shah 2003). Diabetes is thought to be polygenetic and many different genetic factors contribute to the pathophysiology of diabetes (Turner et al 1995). A typical example is the recent report from Matsunaga-Irie et al (2004). They found a significant association with diabetic nephropathy in type 2 diabetes when they examined the 242C/T polymorphism accompanied with the receptor for advanced glycation end products (RAGE) gene 1704G/T polymorphism. It is likely that other genetic factors in addition to RAGE polymorphisms, such as nitric oxide synthetase, methylenetetrahydrofolate reductase, peroxisome proliferator-activated receptor γ−2, and aldose reductase gene polymorphisms may also contribute predisposing factors to diabetic nephropathy (Caramori et al 2003; Noiri et al 2000, 2002; Zhao et al 2004b). Hodgkinson et al 2003) showed an association of the 242C/T polymorphism with diabetic nephropathy in type 1 diabetes. However, the allele frequencies in their control samples were very different from those in previous reports, and the genotype frequencies significantly deviated from the Hardy–Weinberg equilibrium, suggesting nonrandom sampling or some other technical error (Doi et al 2004). On the other hand, the non-DM group in this study, consisting of not only chronic glomerulonephritis but nephrosclerosis, lupus nephritis, interstitial nephritis, and unknown etiology, showed a significant association with ESRD. In clinical trials demonstrating the effect of ACE inhibitors on nondiabetic renal disease, such as a REIN study, the patients also exhibited glomerular disease, interstitial disease, and unknown etiology (Ruggenenti et al 1999). Therefore, our data indicated that diabetic nephropathy is genetically distinct from nondiabetic renal diseases.
In the literature to date, there is only one case-control association study of NAD(P)H p22 phox polymorphisms with kidney that is categorized as non-DM. Wolf et al (2002) could not demonstrate any significant association of the 242C/T polymorphism with IgA nephropathy and lupus nephritis. The conflict between their results and ours seems to be due to the fact that their samples included not only patients with ESRD but those with preterminal renal failure, as well as the fact that their number of samples was relatively small. Moreover, they did not examine 640A/G and other polymorphisms at all. At the same time, previous case-control association studies with CAD have produced conflicting results (Whitehead and FitzGerald 2001). Only three studies in the literature have examined both 242C/T and the 640A/G polymorphisms (Gardemann et al 1999; Inoue et al 1998; Zafari et al 2002). Gardemann et al (1999) reported a protective effect of the G allele upon analyzing the samples of 2,205 CAD patients whose coronary artery lesions were defined by angiography. However, Inoue et al (1998) found a significant association not with 640A/G but with 242C/T polymorphism, and Zafari et al (2002) did not find any association with either of these polymorphisms. It is worth noting that haplotype analyses were not performed in these three studies.
In the present study, we performed haplotype estimation and linkage disequilibrium analysis—for the first time, to our knowledge—and found different distributions of the haplotypes with 242C/T and 640A/G polymorphisms among the study groups. The 242C–640A haplotype was revealed to be more frequent in the non-DM group than in the control group. Previous reports of case-control studies and in vivo functional analyses have also indicated the protective effects of the 242T allele and 640G allele for CAD (Gardemann et al 1999; Inoue et al 1998), carotid atherosclerosis (Hayaishi-Okano et al 2003), reactive oxygen species production (Guzik et al 2000; Wyche et al 2004). The 242C/T polymorphism is assumed to play an important role in NAD(P)H oxidase activity because this polymorphism results in the substitution of histidine-72 with tyrosine. Guzik et al (2000) elucidated the effect of the 242T (72 tyrosine) allele for reduction of superoxide generation by NAD(P)H oxidase, using saphenous vein and internal mammary artery from patients undergoing coronary artery bypass surgery. Wyche et al (2004) demonstrated that the 242C/T polymorphism was associated with superoxide production from neutrophils isolated from healthy individuals using a specific method of electron spin resonance spectroscopy (ESR). Although there has not been any functional analysis of the 640A/G polymorphism, the 3′ UTR is generally known to contain important sequences that contribute directly and significantly to the longevity of mRNA transcripts (Ross 1995) and it is possible that unknown regulatory proteins responsible for mRNA stability bind to this polymorphic site. These observations suggest that the homozygote of the haplotype 242C–640A, 242CC–640AA genotype, which does not possess any protective allele, might be associated with higher reactive oxygen species production and subsequent renal damage in accordance with our data. Considering the effect of ACE inhibitors on NAD(P)H oxidase suppression, patients with this risk genotype of 242CC–640AA should be treated with early and intensive ACE inhibition therapy to prevent progression to ESRD.
In this study, there was a significant difference in terms of age and gender between our ESRD samples and the control samples. A significant association of the 242CC–640AA genotype with nondiabetic ESRD was still found even after adjusting for these confounding factors. Moreover, the ESRD patients in this study represent advanced phenotypes of CKD. Iseki et al (2003) reported that only 0.2% of 86,253 Japanese individuals who participated in healthy check-ups and showed no proteinuria developed ESRD during 17 years of follow-up. Consequently, the estimated probability of false-positive association is minimal in this particular disease group even if some individuals in the control group become ESRD patients in the future.
In conclusion, we identified a risk haplotype for ESRD in NAD(P)H oxidase p22 phox polymorphisms. Haplotype estimation in these polymorphisms, moreover, proved useful when locating the primary susceptibility gene for progression to ESRD. On the other hand, this risk haplotype only showed a significant association with nondiabetic ESRD, indicating that the progression of diabetic nephropathy was genetically distinct from nondiabetic renal disease due to its genetic complexity.
References
Caramori ML, Canani LH, Costa LA, Gross JL (2003) The human peroxisome proliferator-activated receptor gamma2 (PPARgamma2) Pro12Ala polymorphism is associated with decreased risk of diabetic nephropathy in patients with type 2 diabetes. Diabetes 52:3010–3013
Doi K, Doi H, Noiri E, Nakao A, Fujita T, Tokunaga K (2004a) High-throughput single nucleotide polymorphism typing by fluorescent single-strand conformation polymorphism analysis with capillary electrophoresis. Electrophoresis 25:833–838
Doi K, Noiri E, Tokunaga K (2004b) The association of NAD(P)H oxidase p22phox with diabetic nephropathy is still uncertain: response to Hodgkinson, Millward, and Demaine. Diabetes Care 27:1518–1519 (author reply 1519)
Excoffier L, Slatkin M (1995) Maximum-likelihood estimation of molecular haplotype frequencies in a diploid population. Mol Biol Evol 12:921–927
Fallin D, Cohen A, Essioux L, Chumakov I, Blumenfeld M, Cohen D, Schork NJ (2001) Genetic analysis of case/control data using estimated haplotype frequencies: application to APOE locus variation and Alzheimer’s disease. Genome Res 11:143–151
Gardemann A, Mages P, Katz N, Tillmanns H, Haberbosch W (1999) The p22 phox A640G gene polymorphism but not the C242T gene variation is associated with coronary heart disease in younger individuals. Atherosclerosis 145:315–323
Guzik TJ, West NE, Black E, McDonald D, Ratnatunga C, Pillai R, Channon KM (2000) Functional effect of the C242T polymorphism in the NAD(P)H oxidase p22phox gene on vascular superoxide production in atherosclerosis. Circulation 102:1744–1747
Hannken T, Schroeder R, Stahl RA, Wolf G (1998) Angiotensin II-mediated expression of p27Kip1 and induction of cellular hypertrophy in renal tubular cells depend on the generation of oxygen radicals. Kidney Int 54:1923–1933
Hayaishi-Okano R, Yamasaki Y, Kajimoto Y, Sakamoto K, Ohtoshi K, Katakami N, Kawamori D, Miyatsuka T, Hatazaki M, Hazama Y, Hori M (2003) Association of NAD(P)H oxidase p22 phox gene variation with advanced carotid atherosclerosis in Japanese type 2 diabetes. Diabetes Care 26:458–463
Hodgkinson AD, Millward BA, Demaine AG (2003) Association of the p22phox component of NAD(P)H oxidase with susceptibility to diabetic nephropathy in patients with type 1 diabetes. Diabetes Care 26:3111–3115
Inoue N, Kawashima S, Kanazawa K, Yamada S, Akita H, Yokoyama M (1998) Polymorphism of the NADH/NADPH oxidase p22 phox gene in patients with coronary artery disease. Circulation 97:135–137
Iseki K, Ikemiya Y, Iseki C, Takishita S (2003) Proteinuria and the risk of developing end-stage renal disease. Kidney Int 63:1468–1474
Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, Maschio G, Brenner BM, Kamper A, Zucchelli P, Becker G, Himmelmann A, Bannister K, Landais P, Shahinfar S, de Jong PE, de Zeeuw D, Lau J, Levey AS (2001) Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 135:73–87
Jones SA, Hancock JT, Jones OT, Neubauer A, Topley N (1995) The expression of NADPH oxidase components in human glomerular mesangial cells: detection of protein and mRNA for p47phox, p67phox, and p22phox. J Am Soc Nephrol 5:1483–1491
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD (1993) The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The collaborative study group. N Engl J Med 329:1456–1462
Lewontin RC (1964) The interaction of selection and linkage. I. General considerations; heterotic models. Genetics 120:849–852
Li JM, Shah AM (2003) ROS generation by nonphagocytic NADPH oxidase: potential relevance in diabetic nephropathy. J Am Soc Nephrol 14:S221–S226
Matsunaga-Irie S, Maruyama T, Yamamoto Y, Motohashi Y, Hirose H, Shimada A, Murata M, Saruta T (2004) Relation between development of nephropathy and the p22phox C242T and receptor for advanced glycation end product G1704T gene polymorphisms in type 2 diabetic patients. Diabetes Care 27:303–307
Miyata T, Kurokawa K, Van Ypersele De Strihou C (2000) Advanced glycation and lipoxidation end products: role of reactive carbonyl compounds generated during carbohydrate and lipid metabolism. J Am Soc Nephrol 11:1744–1752
Moreno MU, San Jose G, Orbe J, Paramo JA, Beloqui O, Diez J, Zalba G (2003) Preliminary characterisation of the promoter of the human p22(phox) gene: identification of a new polymorphism associated with hypertension. FEBS Lett 542:27–31
Noiri E, Taguchi J, Nakao A, Fujita T (2000) MTHFR gene polymorphism as an exacerbation factor of diabetic nephropathy in type 2 diabetes. Analysis in Japanese male hemodialysis patients. Diabetes Care 23:260
Noiri E, Satoh H, Taguchi J, Brodsky SV, Nakao A, Ogawa Y, Nishijima S, Yokomizo T, Tokunaga K, Fujita T (2002) Association of eNOS Glu298Asp polymorphism with end-stage renal disease. Hypertension 40:535–540
Papanastasiou P, Grass L, Rodela H, Patrikarea A, Oreopoulos D, Diamandis EP (1994) Immunological quantification of advanced glycosylation end-products in the serum of patients on hemodialysis or CAPD. Kidney Int 46:216–222
Remuzzi G, Bertani T (1998) Pathophysiology of progressive nephropathies. N Engl J Med 339:1448–1456
Ross J (1995) mRNA stability in mammalian cells. Microbiol Rev 59:423–450
Ruggenenti P, Perna A, Gherardi G, Garini G, Zoccali C, Salvadori M, Scolari F, Schena FP, Remuzzi G (1999) Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet 354:359–364
Turner RC, Hattersley AT, Shaw JT, Levy JC (1995) Type II diabetes: clinical aspects of molecular biological studies. Diabetes 44:1–10
Ushio-Fukai M, Zafari AM, Fukui T, Ishizaka N, Griendling KK (1996) p22phox is a critical component of the superoxide-generating NADH/NADPH oxidase system and regulates angiotensin II-induced hypertrophy in vascular smooth muscle cells. J Biol Chem 271:23317–23321
Vaziri ND, Dicus M, Ho ND, Boroujerdi-Rad L, Sindhu RK (2003) Oxidative stress and dysregulation of superoxide dismutase and NADPH oxidase in renal insufficiency. Kidney Int 63:179–185
Wang D, Chen Y, Chabrashvili T, Aslam S, Borrego Conde LJ, Umans JG, Wilcox CS (2003) Role of oxidative stress in endothelial dysfunction and enhanced responses to angiotensin II of afferent arterioles from rabbits infused with angiotensin II. J Am Soc Nephrol 14:2783–2789
Whitehead AS, FitzGerald GA (2001) Twenty-first century phox: not yet ready for widespread screening. Circulation 103:7–9
Wolf G, Panzer U, Harendza S, Wenzel U, Stahl RA (2002) No association between a genetic variant of the p22(phox) component of NAD(P)H oxidase and the incidence and progression of IgA nephropathy. Nephrol Dial Transplant 17:1509–1512
Wyche KE, Wang SS, Griendling KK, Dikalov SI, Austin H, Rao S, Fink B, Harrison DG, Zafari AM (2004) C242T CYBA polymorphism of the NADPH oxidase is associated with reduced respiratory burst in human neutrophils. Hypertension 43:1246–1251
Zafari AM, Davidoff MN, Austin H, Valppu L, Cotsonis G, Lassegue B, Griendling KK (2002) The A640G and C242T p22(phox) polymorphisms in patients with coronary artery disease. Antioxid Redox Signal 4:675–680
Zhao HL, Tong PC, Lai FM, Tomlinson B, Chan JC (2004) Association of glomerulopathy with the 5′-end polymorphism of the aldose reductase gene and renal insufficiency in type 2 diabetic patients. Diabetes 53:2984–2991
Acknowledgements
The authors are grateful to Dr. Jun Ohashi (University of Tokyo) for suggestions about statistical analysis, and to Drs. Yasushi Yukiyama, Hitoshi Miyake (Fujitsu Kawasaki Hospital), Tadahiro Nishi (Nishi Clinic), Takashi Ozawa (Kodaira Kitaguchi Clinic), Hisakazu Degawa (Sinkoiwa Clinic Funabori), and Hiroshi Nonaka (Nonaka Clinic) for providing samples. This study was supported by a Grant-in-Aid for Scientific Research on Priority Areas (C) “Medical Genome Science” (K.T.), Grant #14370315 from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (E.N.), and a grant from the Cell Science Research Foundation (E.N.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doi, K., Noiri, E., Nakao, A. et al. Haplotype analysis of NAD(P)H oxidase p22 phox polymorphisms in end-stage renal disease. J Hum Genet 50, 641–647 (2005). https://doi.org/10.1007/s10038-005-0310-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-005-0310-4
Keywords
This article is cited by
-
Association of NADPH oxidase p22phox gene C242T, A640G and −930A/G polymorphisms with primary knee osteoarthritis in the Greek population
Molecular Biology Reports (2013)
-
Genetic polymorphisms of NAD(P)H oxidase: variation in subunit expression and enzyme activity
The Pharmacogenomics Journal (2008)