Abstract
Histamine plays a major role in allergic disorders, including asthma. A major pathway of histamine biotransformation in the lungs is mediated by histamine N-methyltransferase (HNMT). We investigated the association of a functional SNP C314T; a SNP A929G, a (CA)n repeat in intron 5, and a novel (CA)n repeat (BV677277), 7.5 kb downstream of the HNMT gene with asthma and its associated traits such as total serum IgE levels in a case-control as well as in a family-based study design. In contrast to a previous study, no association was observed for the polymorphisms investigated with asthma (P>0.05). When haplotypes were constructed for these loci and compared, no significant difference was observed in the distribution between cases and controls. In the family-based design, no biased transmission was observed for any of the polymorphisms and haplotypes with asthma using the additive model of inheritance in family-based association test (FBAT). Thus, consistent with the case-control findings, the polymorphisms and haplotypes in the HNMT gene are not associated with asthma in the Indian population.
Similar content being viewed by others
Introduction
Histamine is an important preformed mediator in allergic disorders (Bachert 1998; Miescher and Vogel 2002). It includes one of the most important mediators released from the mast cells and basophils after the cross-linking of surface-bound IgE by allergen and causes bronchoconstriction in the lungs (Horton et al. 2001). In mammals, primarily two enzymes metabolize histamine: histamine N-methyl transferase (HNMT) and diamine oxidase (Yamauchi et al. 1994; Weinshilboum et al. 1999). However, HNMT plays the dominant role in histamine biotransformation in the bronchial epithelium (Okinaga et al. 1995; Deindl et al. 2005).
There are large differences in HNMT activity in various human tissues. Previous biochemical studies have revealed a five-fold variation in HNMT activity in human red blood cell (RBCs), predominantly as a result of common genetic polymorphisms (Scott et al. 1988; Price et al. 1993). A functional single nucleotide polymorphism (SNP), C314T, has been identified in the HNMT gene that results in an amino acid change (Thr105Ile). The 314T (Ile105) allele was associated with decreased levels of HNMT enzymatic activity (Preuss et al. 1998). Therefore, the presence of the 314T allele might result in reduced histamine metabolism and may influence the susceptibility to develop bronchial hyperresponsiveness (BHR), a hallmark of asthma. A previous study carried out in the Caucasian population found a positive association of this SNP with asthma (Yan et al. 2000a). On the other hand, a study carried out in the European population failed to find any association of this polymorphism and another polymorphism in the 3′-UTR (A939G) with food allergy (Petersen et al. 2003). Another study carried out in the Japanese population also failed to replicate any association of the C314T polymorphism with atopic asthma (Sasaki et al. 2000). A recent study carried out in two pediatric cohorts recruited from the German population also failed to replicate the association of the C314T SNP with asthma and BHR (Deindl et al. 2005). In addition to these polymorphisms, a polymorphic (CA)n repeat has also been found in intron 5 of the HNMT gene (Yan et al. 2000b).
We conducted a case-control as well as a family-based study to identify the genetic association of the HNMT gene with asthma in the Indian population. We investigated C314T, (CA)n repeat in intron 5, A939G, and a novel (CA)n repeat polymorphism (BV677277) 7.5 Kb downstream of the gene in the study population and attempted to evaluate the association of these markers individually and at the level of haplotype with asthma and its associated quantitative traits such as total serum IgE levels. Our results show that the HNMT gene is not associated with asthma in the Indian population.
Materials and methods
Subjects
Unrelated atopic asthmatics [n=216, 28.2±14.82 years, gender ratio (M/F)=0.55:0.45] were recruited from various collaborating hospitals of northern India (Table 1). For the family based study, 135 probands were recruited [mean age=14.5±9.7 years, gender ratio (M/F)=0.56:0.44]. These probands had to have at least one biological sibling willing to participate in the study, and all relatives who agreed to participate were also recruited. All individuals gave their informed consent, and the institutional ethics committee approved the study. Patients were selected using a questionnaire for obtaining details of present and past history of physician-diagnosed asthma, history of atopy with allergic symptoms (allergic rhinitis, atopic dermatitis, allergic conjunctivitis, hay fever, food allergy, drug allergy), family history, the geographical region of origin, and migration status (Nagarkatti et al. 2002). Clinical tests performed to validate the asthma phenotype were PFT [FEV1, bronchial reversibility (>15%) test using β2-agonist inhaler (albuterol/salbutamol)], skin-prick test (SPT, wheal reaction >3 mm diameter) to a panel of 15 local environmental allergens, and total serum IgE. Only individuals (probands) with a family history of asthma and/or atopy (i.e., individuals having strong familial tendencies to develop allergic reactions) were included in the study. Healthy volunteers/normal controls (n=263, 26.82±10.42 years) were selected on the basis of the criteria of having no symptoms or history of above-mentioned allergic diseases (Table 1). Individuals who were active smokers in the past 2 years or suffering from parasitic/helminthic infestations (as determined from the clinical histories) were excluded. The genetic homogeneity between patients and controls was confirmed by genotyping loci as yet unlinked to asthma or related atopic disorders (Sharma et al. 2004).
PCR amplification and genotyping
Genomic DNA was isolated using a standardized protocol (Nagarkatti et al. 2002) and genotyped for polymorphisms within and around the HNMT gene. The C314T, A595G, A939G, and A1097T polymorphisms were amplified using primers as detailed in Table 2. These polymorphisms were scored using SNapShot ddNTP primer extension kit (Applied Biosystems, Foster city, CA, USA) as per the manufacturer’s instructions. Putative repetitive sequences in and around the HNMT gene were identified using RepeatMasker software (http://www.repeatmasker.org). A novel (CA)n repeat (BV677277) 7.5 kb downstream of the HNMT gene and a (CA)n repeat in intron 5 of the gene were also genotyped and validated for distribution in our population. The accuracy of the genotyping was confirmed by direct sequencing of DNA samples of homozygous individuals (n=5).
Statistical methods
The differences in allele and genotype frequencies for individual SNPs in patients and controls were analyzed using the χ2 test while the Kolmogorov–Smirnov (KS) test was used to test the association of the (CA)n repeat allele size with asthma (Sharma and Ghosh 2004). Hardy–Weinberg equilibrium (HWE) for patients and controls was calculated using De-finetti program (http://ihg.gsf.de/cgi-bin/hw/hwa1.pl). ANOVA was used to assess the significance of association between polymorphisms of the HNMT gene and quantitative phenotypes such as total serum IgE levels. Haplotypes were generated in patients and unrelated controls using PHASE Version 2.1 (Stephens and Donnelly 2003). The association of haplotypes was tested with asthma status and total serum IgE levels.
For the family-based analysis, family-based association test (FBAT ) was used (http://www.biostat.harvard.edu/~fbat) (Laird et al. 2000; Rabinowitz and Laird 2000). The FBAT software was chosen over the classical transmission disequilibrium test because it allows one to analyze a variety of family structures (e.g., parent–proband trios, families with one or more affected siblings, and sibships with one unaffected subject) under different models of inheritance wherein best results are obtained using the additive model (Laird et al. 2000). This software was particularly suitable for our study, as our samples were heterogeneous with respect to family structures. We also tested for association between haplotypes of the four polymorphisms with asthma using the haplotype FBAT (HBAT) option in the FBAT package.
Power calculations
We used the program PS-power and sample size program (Dupont and Plummer 1998) to test whether our cases and controls were sufficient to detect association to C314T SNP in the HNMT gene. Using the odds ratio reported by Yan et al. 2000a (OR=1.9), and the samples utilized in our study (NP=216×2=432 and NC=263×2=526) and an alpha value of 0.05, the power with the current sample size was 84%.
Results
Total serum IgE levels in patients and healthy volunteers
Total serum IgE levels were found to follow a log normal distribution. When the cases and controls were compared with respect to log total serum IgE levels, a highly significant difference was observed (t ratio=6.13, d.f.=293, P<0.0001) (Table 1). However, there was no difference in the cases and the controls with respect to age and gender (Table 1).
Association analysis with asthma in case-control study
The SNPs C314T and A595G were previously detected by comparing two published human cDNA sequences (Chen et al. 2002). In our initial genotyping, the A595G was found to be nonpolymorphic (N=200). Similarly, this variant was also not detected in the study conducted in the Caucasian population (Preuss et al. 1998). For the C314T SNP, the distribution of the 314A and 314T alleles was found to be similar in cases and controls (LR χ2=0.22, d.f.=1, P=0.64). The distribution of the genotypes CC, CT, and TT was also not significantly different between the two groups (LR χ2=0.61, d.f.=2, P=0.74) (Table 3).
Furthermore, two other SNPs in the 3′UTR, viz., A939G and A1097T, were found to be in complete linkage disequilibrium with each other (D′=1, data not shown), so for all further analyses, A939G was used. No significant difference was observed between the allele and genotype counts for the A939G SNP between the cases and controls (LR χ2=0.1, d.f.=1, P=0.76 at the level of alleles and LR χ2=0.13, d.f.=2, P=0.94 at the genotype level, respectively) (Table 3). The observed genotype counts for none of the markers (C314T and A939G) deviated significantly from those expected according to the HWE (P>0.05). Also, none of the genotypes for these loci were associated with log total serum IgE levels (P>0.05) (Table 3).
When the (CA)n repeat in intron 5 was genotyped and analyzed, a total of 14 alleles were obtained (Table 4). The heterozygosity index for this repeat polymorphism is 0.85. To test for the difference in the distribution of alleles in the patient and control groups, the KS test was carried out. The χ2 value for the largest difference in allele frequency was 1.67 (P=0.43). Thus, the difference in allele counts was not significantly different between patients and controls. One-way ANOVA showed a marginal association between the alleles for this locus and serum IgE levels (F=1.84, d.f.=12, P=0.04) (Table 4). However, on applying the correction for multiple testing, this significance was lost (α=0.05/14=0.0036). Hence, the (CA)n repeat in intron 5 is not associated with serum IgE levels in the Indian population.
We have identified a novel (CA)n repeat (BV677277) 7.5 Kb downstream of the HNMT gene. Genotyping of this repeat in our study population showed a low heterozygosity index of 0.14. A total of four alleles were observed for this locus. The frequency distribution of the alleles is represented in Table 4. Alleles 281 and 283 were the major alleles, present at frequencies above 5%. However, using the KS test, no significant difference was observed for the alleles at this locus between patients and controls (KS χ2=0.19, P=0.91). Also, none of the alleles for this locus were associated with log total serum IgE levels (P>0.05) (Table 4).
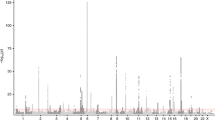
To study the combined effect of these variations, haplotypes were constructed for C314T, intron 5 (CA)n, A939G, and BV677277 (CA)n polymorphisms using PHASE (Stephens and Donnelly 2003). Default parameters were used to generate these haplotypes, and the differences in frequencies were compared in cases and controls. A total of 47 haplotypes were observed; however, the frequency of only eight haplotypes was >5%. These accounted for 77.8% frequency in patients and controls. The relative frequencies of the major haplotypes in patients and controls are shown in Fig. 1. However, there was no statistical difference in the distribution of the haplotypes in the two groups (P>0.05).
Association analysis with asthma in a family-based study
Further, we carried out a family based study to confirm the results obtained from our case-control analysis. A total of 623 individuals from 135 nuclear families were genotyped. There were 135 probands, 173 asthmatic, and 80 relatives with allergic diseases. Apart from these, 230 unaffected (normal) family members were also genotyped. Family structures were varied and included: 43 simple proband–parent trios, 60 nuclear families with a trio and one or more sib pairs, and 32 two-generation families with more than two affected members. Genotype frequencies for the C314T and A939G SNPs did not differ significantly from Hardy–Weinberg expectations in the probands (P>0.05). There was no significant association between asthma and the four polymorphisms investigated using the additive model in FBAT (Table 5).
Haplotype analysis using FBAT revealed no evidence for biased transmission of four marker haplotypes under the additive model of inheritance (Table 5). Similarly, there were no statistically significant results for asthma phenotype when considering two-locus haplotypes for the polymorphisms investigated (P >0.05, data not shown). Thus, consistent with the case-control findings, the haplotypes in the HNMT gene were not associated with asthma.
Discussion
Histamine is produced and stored in airway mast cells and basophils. Upon release from the storage vesicles in response to specific allergens through immunoglobulin E (IgE) receptor triggering, histamine rapidly diffuses into the surrounding tissues where it mediates its vasoconstrictor function (Miescher and Vogel 2002; Beaven 1978). The released histamine is rapidly inactivated and disappears from the site within minutes (Beaven 1978). HNMT plays a dominant role in this process by mediating histamine biotransformation in the bronchial epithelial and endothelial cells of the human airways (Okinaga et al. 1995; Weinshilboum et al. 1999; Horton et al. 2001). In addition, the contractile response of isolated human bronchi to histamine is augmented by the use of an HNMT inhibitor (Yamauchi et al. 1994). Hence, the decreased activity of this major histamine-degrading enzyme in the lungs could result in increased histamine levels and hence increased bronchoconstriction and asthma severity.
Here, we set out to analyze the possible association between polymorphisms in and around the HNMT gene and asthma using family based and case-control studies based on the assumption that histamine metabolism might play a significant role in the pathogenesis of asthma. In addition, we also attempted to look for any possible association of these polymorphisms with another associated trait, serum IgE, as increased serum IgE level is a hallmark feature of atopic asthma. Furthermore, since the HNMT enzyme is involved in histamine metabolism after its release from the mast cells upon cross-linking of IgE-bound receptors by allergens, we wanted to see whether any variant of HNMT was associated with serum IgE levels. Although, C314T, A939G, and BV677277 failed to show any grouping of genotypes and/alleles, the alleles of the (CA)n repeat in intron 5 showed a marginal association with log total serum IgE levels (P=0.04). However, this association was lost on correcting for multiple testing. Thus, the polymorphisms in the HNMT gene were not associated with serum IgE levels in the Indian population.
Additionally, we failed to detect any association between any of these polymorphisms and asthma in both the case-control as well as family-based study design. Furthermore, when we stratified the patient samples into mild, moderate, and severe on the basis of FEV1 values (FEV1 ≥80% predicted classified as mild, 60–80% as moderate, and ≤60% as severe disease), no difference was observed with respect to the distribution of alleles/genotypes in the three groups (data not shown). An earlier study identified the C314T polymorphism as the functional variant within this gene (Preuss et al. 1998). This polymorphism has previously been shown to reduce the enzymatic activity (Preuss et al. 1998) and to represent a risk for asthma in the Caucasian population (Yan et al. 2000a). Yan et al. (2000a) found a significant increase in the frequency of the 314T allele (frequency=0.14) in asthmatic individuals. It is interesting to note that the frequency of the T allele was similar in the controls (frequency=0.08) used by them to the ones used in this study (frequency=0.08); however, the frequency was lesser in the patients used by us (frequency=0.09). This discrepancy in the results obtained in their study and our study could be attributed to the following: (1) variation in ethnicity and environmental exposure; (2) one-third of the patients in their study were nonatopic asthmatics as compared with the atopic asthmatics used in our study, (3) all patients recruited for our study had a positive family history of asthma/atopy, and (4) the gender ratio for the patient population (M/F=0.36:0.64) was different from the one used in our study (0.55:0.45). Thus, it is not very surprising to observe the differences between the results obtained in the two studies. On the other hand, our results are supported by a recent study conducted in two pediatric cohorts from the German population which failed to confirm any effect of this polymorphism on asthma, allergic asthma, FEV1, or BHR (Deindl et al. 2005). Another study carried out with Japanese atopic asthmatics and normal school children also failed to detect any association between the C314T polymorphism and atopic asthma (Sasaki et al. 2000). A study carried out in a European population also failed to detect any association between this polymorphism and A939G polymorphism in the 3′-UTR with food allergy (Petersen et al. 2003). However, it is also possible that studies carried out so far in different populations may not be large enough to detect minor effects of the HNMT polymorphisms on asthma. It is important to point out here that power for our case-control study was >80% for the C314T polymorphism.
To evaluate the combined effect of the polymorphisms on asthma, haplotypes were constructed. This is the first study wherein the association of the HNMT gene was studied using multiple loci (three SNPs and two repeats) individually and at the level of haplotypes, both in the case-control and family-based study design. However, no significant difference was observed in the haplotype frequency in cases and controls in both family-based and case-control studies.
Since asthma is a complex disorder caused by the interaction of many genes, each having only a small effect, we used a case-control study for finding any association with one of the promising loci for asthma (Sharma et al. 2004). However, a case-control study has a higher chance of finding a false positive association than a family-based study. To circumvent this problem, the results from a well-characterized (age- and gender-matched) case-control cohort have been confirmed in a family-based study. We also ensured genetic homogeneity between patients and controls by genotyping markers as yet unlinked to asthma. We found no significant difference in the allele counts in patients and controls used for this study (P>0.05, data not shown). In summary, our findings suggest that the polymorphisms present in and around the HNMT gene are unlikely to be the major risk factors for asthma.
References
Bachert C (1998) Histamine—a major role in allergy? Clin Exp Allergy 28 (Suppl 6):15–19
Beaven MA (1978) Histamine: its role in physiological and pathological processes. Monogr Allergy 13:1–113
Chen GL, Xu ZH, Wang W, Wang GP, Zhou G, Wang D, Zhou HH (2002) Analysis of the C314T and A595G mutations in histamine N-methyltransferase gene in a Chinese population. Clin Chim Acta 326:163–167
Deindl P, Peri-Jerkan S, Deichmann K, Niggemann B, Lau S, Sommerfeld C, Sengler C, Muller S, Wahn U, Nickel R, Heinzmann A, German Multicenter Atopy Study Group (2005) No association of histamine-N-methyltransferase polymorphism with asthma or bronchial hyperresponsiveness in two German pediatric populations. Pediatr Allergy Immunol 16:40–42
Dupont WD, Plummer W (1998) Power and sample size calculations for studies involving linear regression. Control Clin Trials 19:589–601
Horton JR, Sawada K, Nishibori M, Zhang X, Cheng X (2001) Two polymorphic forms of human histamine methyltransferase: structural, thermal, and kinetic comparisons. Structure (Camb) 9:837–849
Laird NM, Horvath S, Xu X (2000) Implementing a unified approach to family-based tests of association. Genet Epidemiol 19 (Suppl 1):S36–S42
Miescher SM, Vogel M (2002) Molecular aspects of allergy. Mol Aspects Med 23:413–462
Nagarkatti R, B Rao C, Rishi JP, Chetiwal R, Shandilya V, Vijayan V, Kumar R, Pemde HK, Sharma SK, Sharma S, Singh AB, Gangal SV, Ghosh B (2002) Association of IFNG gene polymorphism with asthma in the Indian population. J Allergy Clin Immunol 110:410–412
Okinaga S, Ohrui T, Nakazawa H, Yamauchi K, Sakurai E, Watanabe T, Sekizawa K, Sasaki H (1995) The role of HMT (histamine N-methyltransferase) in airways: a review. Methods Find Exp Clin Pharmacol 17 (Suppl C):16–20
Petersen J, Drasche A, Raithel M, Schwelberger HG (2003) Analysis of genetic polymorphisms of enzymes involved in histamine metabolism. Inflamm Res 52(Suppl 1):S69–S70
Preuss CV, Wood TC, Szumlanski CL, Raftogianis RB, Otterness DM, Girard B, Scott MC, Weinshilboum RM (1998) Human histamine N-methyltransferase pharmacogenetics: common genetic polymorphisms that alter activity. Mol Pharmacol 53:708–717
Price RA, Scott MC, Weinshilboum RM (1993) Genetic segregation analysis of red blood cell (RBC) histamine N-methyltransferase (HNMT) activity. Genet Epidemiol 10:123–131
Rabinowitz D, Laird N (2000) A unified approach to adjusting association tests for population admixture with arbitrary pedigree structure and arbitrary missing marker information. Hum Hered 50:211–223
Sasaki Y, Ihara K, Ahmed S, Yamawaki K, Kusuhara K, Nakayama H, Nishima S, Hara T (2000) Lack of association between atopic asthma and polymorphisms of the histamine H1 receptor, histamine H2 receptor, and histamine N-methyltransferase genes. Immunogenetics 51:238–240
Scott MC, Van Loon JA, Weinshilboum RM (1988) Pharmacogenetics of N-methylation: heritability of human erythrocyte histamine N-methyltransferase activity. Clin Pharmacol Ther 43:256–262
Sharma S, Ghosh B (2004) Association of an intragenic microsatellite marker in the CC16 gene with asthma in the Indian population. J Hum Genet 49:677–683
Sharma S, Nagarkatti R, B-Rao C, Niphadkar PV, Vijayan V, Sharma SK, Ghosh B (2004) A_16_C haplotype in the FcepsilonRIbeta gene confers a higher risk for atopic asthma in the Indian population. Clin Genet 66:417–425
Stephens M, Donnelly P (2003) A comparison of bayesian methods for haplotype reconstruction from population genotype data. Am J Hum Genet 73:1162–1169
Weinshilboum RM, Otterness DM, Szumlanski CL (1999) Methylation pharmacogenetics: catechol O-methyltransferase, thiopurine methyltransferase, and histamine N-methyltransferase. Annu Rev Pharmacol Toxicol 39:19–52
Yamauchi K, Sekizawa K, Suzuki H, Nakazawa H, Ohkawara Y, Katayose D, Ohtsu H, Tamura G, Shibahara S, Takemura M, et al (1994) Structure and function of human histamine N-methyltransferase: critical enzyme in histamine metabolism in airway. Am J Physiol 267:L342–L349
Yan L, Galinsky RE, Bernstein JA, Liggett SB, Weinshilboum RM (2000a) Histamine N-methyltransferase pharmacogenetics: association of a common functional polymorphism with asthma. Pharmacogenetics 10:261–266
Yan L, Szumlanski CL, Rice SR, Sobell JL, Lachman HM, Weinshilboum RM (2000b) Histamine N-methyltransferase functional polymorphism: lack of association with schizophrenia. Am J Med Genet 96:404–406
Acknowledgements
We thank our collaborating physicians Drs. S.K. Sharma, N.K. Bhatia, and P.V. Niphadkar for helping us in sample collection. We also thank all patients, their family members, and healthy volunteers for participating in this study. We thank Ms. Abha Soni, Mr. Amrendra Gupta, and Ms. Sanober Nahid for assistance. We acknowledge the Functional Genomics Unit of Institute of Genomics and Integrative Biology (IGIB) and The Center for Genomics Applications (TCGA), Delhi, for helping in sequencing and genotyping. The financial support from the Council of Scientific and Industrial Research (CSIR Task force project No. SMM0006), Government of India, is greatly acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Accession No.: BV677277
Rights and permissions
About this article
Cite this article
Sharma, S., Mann, D., Singh, T.P. et al. Lack of association of histamine-N-methyltransferase (HNMT) polymorphisms with asthma in the Indian population. J Hum Genet 50, 611–617 (2005). https://doi.org/10.1007/s10038-005-0302-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-005-0302-4
Keywords
This article is cited by
-
Histamine: New Thoughts About a Familiar Mediator
Clinical Pharmacology & Therapeutics (2011)
-
Polymorphisms of two histamine-metabolizing enzymes genes and childhood allergic asthma: a case control study
Clinical and Molecular Allergy (2010)