Abstract
DNase II is an important enzyme for DNA fragmentation and degradation during programmed cell death and, consequently, a potential candidate gene for genetic study of systemic lupus erythematosus (SLE). Genetic associations of DNase II with SLE and related phenotypes were examined in Korean patients with SLE. A total of 350 Korean SLE patients and 330 healthy subjects were enrolled. Direct DNA sequencing and TaqMan were employed. Logistic regression analyses were performed to examine the genetic association with SLE and related phenotypes. Through direct sequencing in 24 Korean individuals, six sequence variants were identified: one in the 5′ flanking region, four in exons (including one nonsynonymous), and one in the 3′ flanking region. Four of these polymorphisms were selected for a larger-scale genotyping (350 SLE patients and 330 normal controls). No significant associations with the risk of SLE were detected. However, further analyses of association with the risk of renal disorder among SLE patients revealed several positive associations. One promoter SNP (–1066G>C), +2630T>C (Ser145Ser), +6235G>C and one haplotype showed weak associations with the risk of nephritis among SLE patients.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is characterized by the accelerated apoptosis of peripheral lymphocytes and the impaired clearance of apoptotic cells. The combination of these defects results in the release of increased amounts of nucleosomes with abnormally methylated and GC-rich DNA and, consequently, an autologous stimulation that could bypass tolerance to systemic autoimmune diseases (Huck et al. 1999). The etiology of SLE is very complex, involving both environmental and genetic factors and probably also a synergistic relationship between these factors. Genetic factors are likely to play a significant role in susceptibility to SLE in determining the disease expression and in the autoantibody profiles of individuals with SLE (Wakeland et al. 2001).
Deoxyribonuclease II, Lysosomal (DNase II, MIM 126350), located on chromosome 19p13.2-q13.4, is an important enzyme for DNA fragmentation and degradation during programmed cell death. Because DNase II is directly implicated in engulfment-mediated DNA, it is very likely that a generalized deficiency in DNA clearance due to the disruption of DNase II expression will lead to some form of autoimmune dysfunction, in particular, SLE. DNase II hydrolyzes the phosphodiester backbone of DNA molecules by a single-strand cleavage mechanism (Baker et al. 1998; Lyon et al. 1996). In mice, the inefficient clearance of nuclear antigens can predispose them to autoimmune diseases such as SLE (Robson and Walport 2001). Classical symptoms of SLE include moderate-to-high levels of anti-DNA antibodies (to both double- and single-stranded DNA) and excessive protein in the urine (proteinuria and glomerulonephritis) (Robson and Walport 2001).
Despite the functional importance of the DNase II gene, polymorphisms of DNase II have not been fully examined. In an effort to discover polymorphism(s) in genes in which variant(s) might be implicated in clinical manifestations of SLE, we scrutinized the genetic polymorphisms in DNase II by direct sequencing. Here we present six genetic variants found in DNase II, among which four were genotyped on a larger scale (n=680), and the results of association analyses with phenotypes of SLE in the Korean population.
Materials and methods
Subjects
A total of 350 Korean SLE patients who fulfilled the 1997 American College of Rheumatology (ACR) criteria for SLE (Hochberg 1997) were consecutively enrolled between September 1998 and February 2002 from the Hospital for Rheumatic Diseases, Hanyang University, Seoul, Korea. The following clinical and laboratory data were obtained: gender, age, age at first symptom onset and clinical diagnosis, ACR diagnosis, and Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) damage index (Gladman et al. 1996). Renal disorder was defined as persistent proteinuria greater than 0.5 g per day or greater than 3+ if quantitation not performed or cellular casts according to ACR criteria and found in 36.2% of patients with SLE (Hochberg 1997). Renal biopsy was performed in 56% of patients with renal disorder and revealed class II (2.4%), III (7.2%), IV (28.0%), V (8.8%), III+V (4.0%), and IV+V (5.6%) according to the World Health Organization (WHO) classification of lupus nephritis (Churg et al. 1995). As a control group, we included 330 healthy ethnically matched subjects in our examination of the genetic association of polymorphisms with susceptibility to SLE and related phenotypes. Testing for antinuclear antibodies (Abs) was carried out by indirect immunofluorescence using IT-1 cells; anti-dsDNA Abs by Crithidia lucilliae assay; and anti-Sm, -SSA (Ro), -SSB (La), and -RNP (ribonuclear protein) Abs by double immunodiffusion.
Sequencing and genotyping analysis of the DNase II gene
We sequenced the whole coding sequence of the DNase II gene, including the promoter region (~1.5 kb), to discover genetic variants in 24 Korean DNA samples using a DNA analyzer (ABI PRISM 3700, Applied Biosystems, Foster City, CA, USA). Eleven primer sets of DNase II for the amplification and sequencing analysis were designed based on GenBank sequences (Ref. Genome seq. for DNase II; NT_011295.10). Information regarding the primers used is available on our Web site (http://www.snp-genetics.com/user/additional_list.asp). Sequence variants were verified by chromatograms. For genotyping of polymorphic sites, amplifying primers and probes were designed for TaqMan (Livak 1999). Information regarding the primers is also available on our Web site (http://www.snp-genetics.com/user/additional_list.asp).
Statistics
We examined Lewontin’s D′ (|D′ |) and the linkage disequilibrium coefficient r2 between all pairs of biallelic loci (Hedrick 1987). Haplotypes of each individual were inferred using the algorithm developed by Stephens et al. (2001) (PHASE), which uses a Bayesian approach incorporating a priori expectations of haplotypic structure based on population genetics and coalescent theory. Genetic effects of inferred haplotypes were analyzed in the same way as polymorphisms. The genotype distributions of DNase II polymorphisms and haplotypes between SLE patients and normal subjects and among SLE patients were analyzed with logistic regression models while controlling for age (continuous variable), gender (male=0, female=1), and/or disease duration (continuous variable) as covariates.
Results and discussion
In order to clarify the association of DNase II polymorphisms with SLE, we scrutinized the genetic polymorphisms in the whole coding sequence of DNase II, including the –1,500-bp promoter region, by direct sequencing in 24 Korean individuals. Six sequence variants were identified: one in the 5′ flanking region, four in exons (including one nonsynonymous), and one in the 3′ flanking region. The frequencies in the Korean population are shown in Fig. 1a. Although –75G>A, which altered the promoter activity, was previously reported in the Japanese population (Yasuda et al. 2000), we could not identify it in this study. Two major haplotypes accounted for over 92% of distribution (Fig. 1b) and were used in further analysis.
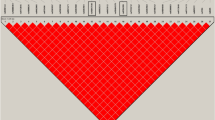
Gene maps and haplotypes of DNase II. Coding exons are marked by black blocks and 5′ and 3′ untranslated regions (UTRs) by white blocks. The first base of the translation start site is denoted as nucleotide +1. Asterisks indicate polymorphisms genotyped in a larger population (n=680). The frequencies of polymorphisms not subjected to larger-scale genotyping were based on sequence data (n=24). a Polymorphisms identified in DNase II on chromosome 19p13.2-q13.4 (Reference Genome Sequence NT_011295.10). b Haplotypes of DNase II. c Linkage disequilibrium coefficients (|D′ | and r2) among DNase II polymorphisms.
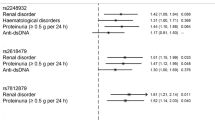
Several complete linkage disequilibriums (LDs) (|D′ |=1 and r2 ≠ 1) were identified among polymorphisms in DNase II (Fig. 1a, c). Four of these polymorphisms were selected for larger-scale genotyping (n=680) by considering their allele frequencies, haplotype-tagging status, and LD coefficients among polymorphisms. The associations between DNase II polymorphisms and the clinical profiles of SLE were analyzed. Although no significant associations with the risk of SLE were detected (please see additional Table ad1 at our Web site, http://www.snp-genetics.com/user/additional_list.asp), further analyses of association with renal disorder [as defined by ACR SLE criteria (Hochberg 1997)], which is important SLE phenotype, revealed that the –1066G>C, +2630T>C (Ser145Ser), +6235G>C, and the most common haplotype (ht1; G-T-G-G, frequency=0.599) showed weak associations with the risk of renal disorder among SLE patients (Table 1).
SLE is a clinically heterogeneous autoimmune disorder that predominantly affects women (approximately 90% of SLE patients) and is much more prevalent and severe in African Americans compared with European Americans (Kaslow and Masi 1978). The etiology of SLE is complex, involving both environmental and genetic factors and, likely, a synergistic relationship between the two. High heritability (>66%) (Lawrence et al. 1987), higher concordance rates among monozygotic twins (25–69%) compared with dizygotic twins and other full siblings (2–3%) (Deapen et al. 1992), and familial aggregation (Sestak et al. 1999) all support the genetic component of this disease. Several genetic factors appear to play roles in SLE susceptibility, determining certain serologic and clinical characteristics of the disease (Wakeland et al. 1999).
DNase I removes DNA and attacks double-stranded DNA and produces 5′ phosphoryl oligonucleotides at sites of high cell turnover whereas DNase II hydrolyzes DNA under acidic conditions (Bernardi 1971). Our previous study revealed that one nonsynonymous SNPs in exon 8, +2373A>G (Gln244Arg), was significantly associated with an increased risk of the production of anti-RNP and anti-dsDNA antibodies among SLE patients (Shin et al. 2004). The present study provides, for the first time, information about genetic polymorphisms in DNase II and positive associations of those polymorphisms with important lupus phenotype (renal disorder) among SLE patients in the Korean population. The effects of DNase II genetic polymorphisms on the risk of renal disorder among SLE patients were not dramatic in the present study. Therefore, it may be argued that Bonferroni correction should be applied to the P values obtained. If Bonferroni correction were strictly adopted, associated P values could not retain the significance [the threshold of significance would be 0.004 (six polymorphisms and two phenotypes analyzed)]. However, although there is a chance of type 1 error due to multiple comparisons, the associations detected in this study might be worth noting when considering the facts (1) that the comparisons were not totally independent of each other due to tight LDs among SNPs/haplotype, and (2) multiple positive associations were detected in a single gene. In addition, epistatic analyses were performed using DNASE I and DNASE II polymorphisms with renal disorder. The genotype DNASE I+2373A>G, which showed significant association with antibody production in SLE patients, was used for analysis. No apparent differences were detected (please see Table ad2 at our Web site http://www.snp-genetics.com/user/additional_list.asp). Further biological and/or functional evidence would be needed to confirm the suggested association of DNase II polymorphisms with nephritis among SLE patients in this study.
In summary, we have identified six polymorphic sites in the DNase II gene, and two common haplotypes were constructed with four genotyped polymorphisms. Statistical analyses revealed that SNPs and haplotypes in the DNase II gene are associated with renal disorder among SLE patients. We suggest that polymorphisms in the DNase II gene might play important roles in controlling renal disorder among SLE patients. The polymorphism/association information identified in this study would be useful for further genetic studies of other autoimmune diseases.
References
Baker KP, Baron WF, Henzel WJ, Spencer SA (1998) Molecular cloning and characterization of human and murine DNase II. Gene 215:281–289
Bernardi G (1971) The enzymes. Academic, New York
Churg J, Bernstein J, Glassock R (1995) Lupus nephritis. In: Renal disease: classification and atlas of glomerular diseases. Igaku-Shoin, New York, pp 151
Deapen D, Escalante A, Weinrib L, Horwitz D, Bachman B, Roy-Burman P, Walker A, Mack TM (1992) A revised estimate of twin concordance in systemic lupus erythematosus. Arthritis Rheum 35:311–318
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, Bacon P, Bombardieri S, Hanly J, Hay E, Isenberg D, Jones J, Kalunian K, Maddison P, Nived O, Petri M, Richter M, Sanchez-Guerrero J, Snaith M, Sturfelt G, Symmons D, Zoma A (1996) The development and initial validation of the systemic lupus international collaborating clinics/American college of rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 39:363–369
Hedrick PW (1987) Gametic disequilibrium measures: proceed with caution. Genetics 117:331–341
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Huck S, Deveaud E, Namane A, and Zouali M (1999) Abnormal DNA methylation and deoxycytosine-deoxyguanine content in nucleosomes from lymphocytes undergoing apoptosis. FASEB J 13:1415–1422
Kaslow RA, Masi AT (1978) Age, sex, and race effects on mortality from systemic lupus erythematosus in the United States. Arthritis Rheum 21:473–479
Lawrence JS, Martins CL, Drake GL (1987) A family survey of lupus erythematosus. 1 Heritability J Rheumatol 14:913–921
Livak KJ (1999) Allelic discrimination using fluorogenic probes and the 5′ nuclease assay. Genet Anal 14:143–149
Lyon CJ, Miranda GA, Piao JS, Aguilera RJ (1996) Characterization of an endonuclease activity which preferentially cleaves the G-rich immunoglobulin switch repeat sequences. Mol Immunol 33:157–169
Robson MG, Walport MJ (2001) Pathogenesis of systemic lupus erythematosus (SLE). Clin Exp Allergy 31:678–685
Sestak AL, Shaver TS, Moser KL, Neas BR, Harley JB (1999) Familial aggregation of lupus and autoimmunity in an unusual multiplex pedigree. J Rheumatol 26:1495–1499
Shin HD, Park BL, Kim LH, Lee HS, Kim TY, Bae SC (2004) Common DNase I polymorphism associated with autoantibody production among systemic lupus erythematosus patients. Hum Mol Genet 13:2343–2350
Stephens M, Smith NJ, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Wakeland EK, Wandstrat AE, Liu K, Morel L (1999) Genetic dissection of systemic lupus erythematosus. Curr Opin Immunol 11:701–707
Wakeland EK, Liu K, Graham RR, Behrens TW (2001) Delineating the genetic basis of systemic lupus erythematosus. Immunity 15:397–408
Yasuda T, Takeshita H, Nakazato E, Nakajima T, Nakashima Y, Mori S, Mogi K, Kishi K (2000) The molecular basis for genetic polymorphism of human deoxyribonuclease II (DNase II): a single nucleotide substitution in the promoter region of human DNase II changes the promoter activity. FEBS Lett 467:231–234
Acknowledgements
This work was supported in part by a grant of the Korea Health 21 R & D Project, Ministry of Health and Welfare, Republic of Korea (01-PJ3-PG6-01GN11-0002).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, H.D., Park, B.L., Cheong, H.S. et al. DNase II polymorphisms associated with risk of renal disorder among systemic lupus erythematosus patients. J Hum Genet 50, 107–111 (2005). https://doi.org/10.1007/s10038-004-0227-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-004-0227-3
Keywords
This article is cited by
-
Genetic studies of systemic lupus erythematosus in Asia: where are we now?
Genes & Immunity (2009)