Abstract
A convergent total synthesis platform led to the discovery of TP-2758 from a series of novel 7-methoxy-8-heterocyclyl tetracycline analogs. TP-2758 demonstrated high in vitro potency against key Gram-negative pathogens including extended spectrum β-lactamases- and carbapenemase-producing Enterobacteriaceae and Acinetobacter spp. strains. This compound was efficacious when administered either intravenously or orally in multiple murine infection models and displayed a favorable preclinical pharmacological profile supporting its advancement into clinical development.
Similar content being viewed by others
Introduction
The rising number of infections caused by multidrug-resistant (MDR) bacteria, especially extensively drug-resistant Gram-negative bacteria, is a serious public health threat.1 Current and emerging antibiotic-resistant pathogens place high demands on the performance of antibiotics in clinical use. To replenish and expand on the current pipeline of new antibiotics,2 discovery efforts have taken multiple approaches including structure-based drug design,3 natural products screening4 and semi-synthetic derivatization of natural products.5 In a unique approach taken by Tetraphase, novel tetracycline antibiotics, traditionally derived from natural products, are created using a convergent total synthesis platform. This platform, originally discovered by the Myers group at Harvard University6, 7 and later optimized at Tetraphase, has allowed the practical and efficient access to almost every position of the tetracycline core for chemical modifications, including positions previously inaccessible or difficult to access by semi-synthesis. This approach dramatically expanded the tetracycline chemical space and led to the discovery of several new tetracycline antibiotics currently in various stages of clinical development (phase 1–3).8
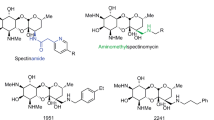
In a previous study,9 we outlined the discovery of a series of novel 7-R-8-heterocyclyl tetracycline compounds, including a 7-trifluoromethyl-8-pyrrolidinyltetracycline analog with enhanced potency against Pseudomonas aeruginosa. In addition to developing agents against P. aeruginosa, another goal was to develop orally available tetracycline compounds with activity against other MDR Gram-negative bacteria listed as Priority 1 pathogens in the recently published World Health Organization Priority Pathogens List for R&D of New Antibiotics.10 We reported several 7-methoxy-8-aminomethyl tetracycline analogs with good oral bioavailability and enhanced Gram-negative antibacterial activities.11 Therefore, we extensively explored the 7-methoxy-8-heterocyclyl tetracycline scaffold and discovered TP-2758, a 7-methoxy-8-pyrrodinyltetracycline analog (11c, Table 1) with potency against a wide range of MDR Gram-negative pathogens and greater oral bioavailability than tetracycline in cynomolgus monkeys. Herein we describe the details of the discovery and biological evaluation of TP-2758.
Results and discussion
Chemistry
A representative approach for the synthesis of 7-methoxy-8-heterocyclyl tetracycline analogs is shown in Scheme 1. Using a similar strategy previously described,9 metal-halogen exchange of bromide 111 with Turbo Grignard followed by addition to 1-Boc-2-pyrrolidinone yielded the desired amino ketone 2, which was then treated with trifluoroacetic acid in dichloromethane to afford the cyclic imine 3, with concomitant removal of the Boc protecting group. Re-protection of the phenol group with di-tert-butyl dicarbonate in the presence of 4-dimethylaminopyridine gave imine 4 in 70% overall yield. Imine 4 was then reduced with sodium borohydride in methanol to afford pyrrolidine 5. Protection of the pyrrolidine nitrogen in compound 5 with trityl chloride gave the desired D-ring precursor 6, which was used directly for the subsequent Michael–Dieckmann reaction without purification. Following our standard Michael–Dieckmann reaction procedure,12 compound 6 reacted with enone 713, 14 to afford the desired pentacyclic intermediate 8 in 86% isolated yield over three steps. The two diastereomers of compound 8 could be readily separated by preparative reverse phase HPLC. Removal of the trityl group under aqueous acidic conditions gave pyrrolidine 9, which was then alkylated either by reductive alkylation with aldehydes or by substitution with alkyl halides. The final global deprotection steps (aqueous hydrogen fluoride for the removal of the Boc and TBS groups; catalytic hydrogenation for cleavage of the benzyl group and opening of the isoxazole ring) provided the desired 7-methoxy-8-pyrrolidinyl tetracycline analogs 11.
Structure–activity relationships of 7-methoxy-8-heterocyclyl tetracycline analogs
The in vitro antibacterial activities of the 7-methoxy tetracycline analogs were determined in minimum inhibitory concentration (MIC) assays, using standardized Clinical Laboratory Standards Institute screening methodology,15 against a panel of tetracycline-susceptible and tetracycline-resistant, Gram-positive and Gram-negative pathogens. As observed previously,9 in most cases the diastereomeric pairs showed very different antibacterial activities across the entire panel. For example, 11c (TP-2758, diastereomer A, S configuration at the C2 position of the pyrrolidine ring16) is two to six dilutions more potent than 11d (diastereomer B, Table 1) across the screening panel of organisms. In Table 1, each of 11b and 11e–h were isolated and tested as a ~1:1 mixture of the respective diastereomers. For clarity, for the remaining compounds, only the relatively more active diastereomer from each diastereomeric set was included in Table 1. Without any substitution on the pyrrolidine nitrogen, compound 11a was barely active in the panel tested. Adding small alkyl groups on the pyrrolidine nitrogen (11b to 11h) resulted in a dramatic potency increase across the entire panel as compared with 11a. With an ethyl group on the pyrrolidine nitrogen, compound 11c (TP-2758) showed the best overall activity against the screening panel and was up to three dilutions more potent than tigecycline against all the Gram-negative strains. However, against Gram-positive bacteria, 11c was less active than tigecycline, especially for the strains with tet(M) genes, probably due to the lack of a C9 side chain, which is known to increase potency against tet(M) strains for both eravacycline12 and tigecycline.17, 18 Incorporation of an additional hydroxy group in 11i and 11j reduced their potency against the tet(M) strains and all of the Gram-negative strains.
We next investigated other heterocyclic ring systems at the C8 position (Table 2). Once again, only the most active diastereomer from each diastereomeric set was included in Table 2 except for 49c, which was isolated and tested as a mixture of the two diastereomers. For the 3,5-fused ring scaffold (28a–d), as observed in the pyrrolidine series, the small alkyl groups on the ring nitrogen are preferred for better antibacterial activity across the panel. With a methyl group substituent on the ring nitrogen, analog 28b showed reduced potency against all the tet(M) strains, whereas its potency against the Gram-negative pathogens is comparable to 11c. Interestingly, with an isopropyl group on the ring nitrogen, compound 28d showed improved potency against Gram-positive pathogens, especially the tet(M) strains, as compared with 11c. However, the potency of 28d against the Gram-negative pathogens either remained the same or decreased by one to two dilutions, except for Stenotrophomonas maltophilia SM256, where its potency was improved by two dilutions. For the bridged ring system analog 35, the activity was decreased significantly across the screening panel. For analogs with the six-membered ring substitution at C8 (42a–d), the overall antibacterial activity was comparable to that of 11c, with slightly less potency (one to three dilutions) against some of the pathogens. Incorporation of an oxygen atom in the ring (49a–d) reduced the potency against the tet(M) strains and all the Gram-negative strains. Thus, compound 11c (TP-2758) remained the most potent compound against the Gram-negative pathogens in the panel.
In vitro potency of TP-2758 against key pathogens
The antibacterial activity of TP-2758 was further evaluated against large panels of Gram-negative and Gram-positive pathogens possessing MDR phenotypes to determine the MIC inhibiting 50% and 90% of the organisms in a given panel (MIC50 and MIC90, respectively) (Table 3 and Table 4). Notably, for Gram-negative pathogens, TP-2758 consistently showed 2- to 4-fold greater potency by MIC90 than tigecycline, and had comparable or better MIC90 values against all clinical comparators tested (Table 3). In a strain-by-strain comparison of TP-2758 activity to tigecycline, TP-2758 was 2- to ⩾8-fold more potent against 95% of A. baumannii isolates (56 out of 59), 90% of Klebsiella pneumoniae isolates (147 out of 164) and 92% of Escherichia coli isolates (111 out of 121).
TP-2758 also showed good potency against MDR strains expressing the New Delhi metallo-β-lactamase-1,19 with MIC values of 4, 0.06 and 2 μg ml−1 against New Delhi metallo-β-lactamase-1 expressing strains K. pneumoniae KP1142, E. coli EC1143 and Enterobacter cloacae EC1144, respectively. Further, it was shown that the addition of 25 μg ml−1 of the efflux inhibitor phenylalanine-arginine-β-naphthylamide (PAβN) could improve the activity of TP-2758 against KP1142 (MICPAβN=0.25 μg ml−1) and EC1144 (MICPAβN=0.12 μg ml−1), indicating that TP-2758 activity is likely limited by intrinsic efflux co-expressed with New Delhi metallo-β-lactamase-1 in these isolates.20
TP-2758 was generally 2- to 16-fold less active than tigecycline, by MIC90, against most Gram-positive pathogens tested (Table 4). However, MIC90 values remained low, ranging from 0.06 (MRSA, Panton-Valentine Leukocidin+) to 2 μg ml−1 (Enterococcus spp.), supporting the broad-spectrum potential of TP-2758. TP-2758 was active (MIC90=0.06 μg ml−1) against community-acquired methicillin-resistant Staphylococcus aureus MRSA expressing Panton-Valentine Leukocidin, a toxin that destroys polymorphonuclear leukocytes and is associated with tissue necrosis and increased virulence.21 TP-2758 also retained good activity against vancomycin-resistant Enterococcus spp., with MIC90=1 μg ml−1.
In vivo oral (PO) and i.v. efficacy of TP-2758 in animal models
A diasteromeric mixture of TP-2758 and its diastereomer 11d provided 100% protection when administered either PO (30 mg kg−1) or i.v. (3 mg kg−1) in a mouse systemic infection model with S. aureus SA100 (ATCC 13709) employed as a screen for oral bioavailability (TP-2758 MIC=0.13 μg ml−1).11 In a BALB/c murine pyelonephritis model challenged with tetracycline-resistant (tet(B)) uropathogenic E. coli EC200 (Figures 1a and e), TP-2758 (MIC=0.06 μg ml−1) produced 3.1 and 4.0 log10 reductions in bacterial colony-forming units (CFUs) in kidney, versus the untreated control group, when dosed at 2 mg kg−1 PO and 5 mg kg−1 i.v., respectively. In the same model, levofloxacin (MIC=0.03 μg ml−1) produced 4.7 and 4.9 log10 CFU reductions when dosed at 2 mg kg−1 PO and 2 mg kg−1 i.v., respectively. In a similar pyelonephritis model challenged with tetracycline- and levofloxacin-resistant extended spectrum β-lactamase-producing (SHV) K. pneumoniae KP453 (Figures 1b and f), TP-2758 (MIC=0.5 μg ml−1) produced 1.5 and 3.8 log10 CFU reductions, versus the untreated control group, when dosed at 50 mg kg−1 PO and 20 mg kg−1 i.v., respectively. In the same model, meropenem/cilastatin (meropenem MIC=0.03 μg ml−1) produced 2.1 and 2.4 log10 CFU reductions when dosed i.v. at 20/20 mg kg−1 t.i.d. and 30/30 mg kg−1 b.i.d., respectively. In a neutropenic murine lung infection model challenged with tetracycline-resistant (tet(M)) MRSA SA191 (Figures 1c and g), TP-2758 (MIC=0.5 μg ml−1) produced 2.5 and 3.1 log10 CFU reductions, versus the untreated control group, when dosed 50 mg kg−1 PO and 10 mg kg−1 i.v., respectively. In the same model, linezolid (MIC=2 μg ml−1) produced 2.3 and 1.2 log10 CFU reductions, when dosed 30 mg kg−1 PO and 30 mg kg−1 i.v., respectively. In a neutropenic murine lung infection model challenged with tetracycline-resistant (tet(M)) Streptococcus pneumoniae SP160 (Figures 1d and h), TP-2758 (MIC=0.06 μg ml−1) produced a 2.5 log10 CFU reduction, versus the untreated control group, when dosed at 30 mg kg−1 PO; linezolid (MIC=0.5 μg ml−1) produced a 2.4 log10 CFU reduction when dosed PO at 30 mg kg−1. When TP-2758 was dosed at 10 mg kg−1 i.v., the resulting lung CFUs were below the level of detection (>6.0 log10 CFU reduction) and linezolid at 30 mg kg−1 PO produced a 2.6 log10 CFU reduction.
In vivo efficacy of TP-2758 and comparators in murine pyelonephritis and lung infection models. Infection models were conducted as described in Materials and Methods and data is represented in bar graphs as mean log10 CFU per gram of tissue. Panels a and e and panels b and f show BALB/c murine pyelonephritis models challenged with E. coli EC200 and K. pneumoniae KP453, respectively. Panels c and g and panels d and h show neutropenic murine lung infection models challenged with MRSA SA191 and S. pneumoniae SP160, respectively. Dark gray bars indicate untreated control group CFUs at the start of dosing (first dark gray bar) and at time of killing (second dark gray bar). Light gray bars indicate CFUs at time of sacrifice in TP-2758-treated groups. White bars indicate CFUs at time of sacrifice in groups treated with comparator antibiotics (levofloxacin for EC200, meropenem/cilastatin for KP453 and linezolid for SA191 and SP160 models). Antibiotic doses were given twice (BID) via the route indicated in each graph, or as noted otherwise, as described in Experimental Section. BLD, below limit of detection. Error bars indicate s.e.m.
TP-2758 pharmacokinetics in rats and monkeys
The pharmacokinetics of TP-2758 were evaluated in fasted male Sprague–Dawley rats by administration of 1 mg kg−1 intravenously into the jugular vein and 10 mg kg−1 by oral gavage. As shown in Table 5, the oral bioavailability (%F) of TP-2758 in rats was 8.62%. As a comparison, using similar methodology and comparable doses in other studies conducted by Tetraphase, the oral bioavailability of tetracycline and tigecycline in rats was 14.9% and 1.0%, respectively (not shown).
The pharmacokinetics of TP-2758 was also studied in non-naive cynomolgus monkeys. As shown in Table 6, the oral bioavailability of TP-2758 in monkeys was 30.4%, exceeding the oral bioavailability observed in rats. Tetracycline has only 6.7% oral bioavailability in monkeys (data from other studies conducted by Tetraphase), but notably >70% in humans,22 suggesting that TP-2758 could have even higher oral exposure in humans. After a 1 mg kg−1 i.v. dose, TP-2758 also showed an average of 5.11±0.16 and 6.49±0.40 μg ml−1 in urine collected between 0–8 and 8–24 post-dose, respectively.
Conclusions
TP-2758 showed in vitro and in vivo potency against a spectrum of MDR Gram-negative and Gram-positive bacteria, supporting its candidacy for development as an antibiotic for empiric use against serious hospital infections with a high incidence of Gram-negative pathogens, including hospital-acquired and ventilator-associated pneumonia, complicated urinary tract infections and complicated intra-abdominal infections. TP-2758 showed good oral bioavailability in cynomolgus monkeys. If the preclinical oral bioavailability seen in cynomolgus monkeys translates to humans, TP-2758 may hold promise as a new i.v./oral antibiotic for use against difficult-to-treat multi-drug-resistant infections. TP-2758 was advanced to phase 1 clinical studies with oral dosing in healthy volunteers.
Experimental Procedures
Chemistry
All reactions involving air-sensitive reagents were performed under nitrogen in flame-dried glassware using syringe-septum cap technique. Unless otherwise specified, all reagents were used as received without further purifications. The progress of all reactions was monitored by LC-MS using a Waters Alliance system (Waters Corporation, Milford, MA, USA) (column, SunFire C18, 5 μm, 4.6 mm × 50 mm; solvent A, water with 0.1% formic acid; solvent B, acetonitrile with 0.1% formic acid; MS detector, Waters 3100). TLC analysis was performed on Merck silica-gel 60 F254 (EMD Millipore, Billerica, MA, USA) and visualized under UV light or by immersion of the plate in a basic solution of potassium permanganate in water followed by heating. Flash chromatography was performed on a Biotage Isolera One purification system using Biotage SNAP cartridges (Biotage, Charlotte, NC, USA). Reverse-phase preparative HPLC was performed on a Waters Autopurification system with mass-directed fraction collection. Unless otherwise noted, all final tetracycline compounds were isolated as mono-, di-, or trihydrochloride salts following freeze-drying. 1H NMR (nuclear magnetic resonance) spectra were recorded on a 400 MHz JEOL ECX-400 (JEOL USA, Inc., Peabody, MA, USA) spectrometer. Purity of tested compounds was determined to be ≥95% by reverse-phase analytical HPLC/MS analysis.
Phenyl 4-(4-{[(tert-butoxy)carbonyl]amino}butanoyl)-6-{[(tert-butoxy)carbonyl]oxy}-3-methoxy-2-methylbenzoate (2)
A solution of i-PrMgCl•LiCl in THF (1.2 M, 4.95 ml, 5.94 mmol, 1.5 eq) was added dropwise to a solution of compound 1 (1.73 g, 3.96 mmol, 1 eq) in THF (20 ml) at 0 °C. The resulting yellow reaction mixture was then stirred at 0 °C for 2 h. The reaction was cooled to –78 °C and N-Boc pyrrolidinone (1.35 ml, 7.92 mmol, 2 eq) was added. The reaction was warmed up to room temperature (rt) and partitioned between saturated aqueous NH4Cl (150 ml) and EtOAc (200 ml). The organic layer was separated, dried over MgSO4 and concentrated under reduced pressure to yield compound 2, which was used directly in the next step without further purification.
Phenyl 4-(3,4-dihydro-2H-pyrrol-5-yl)-6-hydroxy-3-methoxy-2-methylbenzoate (3)
The above compound 2 was dissolved in CH2Cl2 (4 ml). Trifluoroacetic acid (4 ml) was added slowly at rt (gas evolution). The resulting light brown solution was stirred at rt for 20 min and concentrated under reduced pressure. Saturated aqueous NaHCO3 was added. The resulting mixture was extracted with CH2Cl2 (100 ml × 1, 20 ml × 2). The combined organic extracts were dried over MgSO4, filtered and concentrated to a volume of about 30 ml to yield a CH2Cl2 solution of intermediate 3. This solution was used directly for the next reaction.
Phenyl 6-{[(tert-butoxy)carbonyl]oxy}-4-(3,4-dihydro-2H-pyrrol-5-yl)-3-methoxy-2-methylbenzoate (4)
To the above solution was added di-tert-butyl dicarbonate (950 mg, 4.36 mmol, 1.1 eq) and N,N-dimethylaminopyridine (48 mg, 0.396 mmol, 0.1 eq). The reaction mixture was stirred for 15 min at rt and concentrated. The residue was purified by flash column chromatography (5–50% ethyl acetate-hexanes) to afford the desired product 4 as a white solid (1.18 g, 70% over three steps): 1H NMR (400 MHz, CDCl3) δ 7.52 (s, 1 H), 7.42-7.45 (m, 2 H), 7.24–7.30 (m, 3 H), 4.04 (t, J=6.7 Hz, 2 H), 3.71 (s, 3 H), 3.02 (t, J=7.6 Hz, 2 H), 2.45 (s, 3 H), 2.05 (p, J=7.9 Hz, 2 H), 1.43 (s, 9 H); MS (ESI) m/z 426.68 (M+H).
Phenyl 6-{[(tert-butoxy)carbonyl]oxy}-3-methoxy-2-methyl-4-(pyrrolidin-2-yl)benzoate (5)
Sodium borohydride (3.25 g, 86 mmol, 5 eq) was added in portions to a solution of 4 (7.32 g, 17.2 mmol, 1 eq) in CH3OH (70 ml) at 0 °C. Gas evolution was observed. The cold bath was removed, and the reaction mixture was stirred at rt for 10 min. Aqueous HCl (1 N, 60 ml) was added slowly. The resulting white suspension was basified with saturated aqueous NaHCO3 (60 ml) to pH=8–9 and extracted with CH2Cl2 (200 ml × 1, 100 ml × 2). The combined organic extracts were dried over Na2SO4 and concentrated. The crude product was used directly for the next reaction. A small sample was purified by flash column chromatography (50–100% ethyl acetate-hexanes) to afford the desired product 5 as a colorless oil for analysis: 1H NMR (400 MHz, CDCl3) δ 7.39–7.42 (m, 2 H), 7.31 (s, 1 H), 7.22–7.27 (m, 3 H), 4.48 (t, J=7.6 Hz, 1 H), 3.75 (s, 3 H), 3.17–3.22 (m, 1 H), 3.03–3.10 (m, 1 H), 2.41 (s, 3 H), 2.23–2.31 (m, 1 H), 2.12 (br s, 1 H), 1.82–1.96 (m, 2 H), 1.57-1.67 (m, 1 H), 1.41 (s, 9 H); MS (ESI) m/z 428.68 (M+H).
Phenyl 6-{[(tert-butoxy)carbonyl]oxy}-3-methoxy-2-methyl-4-[1-(triphenylmethyl)pyrrolidin-2-yl]benzoate (6)
Trityl chloride (5.75 g, 20.64 mmol, 1.2 eq) and triethylamine (3.12 ml, 22.36 mmol, 1.3 eq) were added to a solution of the above crude compound 5 (17.2 mmol, 1 eq) in CH2Cl2 (100 ml) at rt. The reaction mixture was stirred at rt for 2 h and concentrated. The residue was partitioned between EtOAc (300 ml) and water (100 ml). The organic phase was washed with water (50 ml × 2) and brine (50 ml), dried over MgSO4 and concentrated under reduced pressure to give the desired product 6: MS (ESI) m/z 670.55 (M+H). This crude product was further dried by azeotroping several times from toluene and used in subsequent reactions without further purification.
(1R,3S,4S,11S)-8-(Benzyloxy)-11-[(tert-butyldimethylsilyl)oxy]-4-(dimethylamino)-12-hydroxy-19-methoxy-10,14-dioxo-18-[1-(triphenylmethyl)pyrrolidin-2-yl]-6-oxa-7-azapentacyclo[11.8.0.03,11.05,9.015,20]henicosa-5(9),7,12,15(20),16,18-hexaen-16-yl tert-butyl carbonate (8)
n-BuLi (10.0 ml, 2.4 M/hexanes, 24.08 mmol, 1.4 eq) was added dropwise to a solution of diisopropylamine (3.4 ml, 24.08 mmol, 1.4 eq) in THF (150 ml) at –72 °C. The reaction mixture was warmed up to 0 °C and re-cooled to –74 °C. N,N,N′,N′-tetramethylethylenediamine (3.61 ml, 24.08 mmol, 1.4 eq) was added. The reaction solution was stirred at –78 °C for 10 min. A solution of crude 6 (17.2 mmol) in THF (50 ml) was added dropwise via a cannula between –73→–74 °C over 25 min. The resulting red orange solution was stirred at –74 °C for 45 min, and cooled to –98 °C using a EtOH/liquid N2 bath. A pre-cooled (–78 °C) solution of enone 7 (8.30 g, 17.2 mmol, 1 eq) in THF (50 ml) was added to the reaction mixture via a cannula at –97→–98 °C. The reaction mixture was allowed to gradually warm up to –83 °C over 1 h. Lithium hexamethyldisilazide (17.20 ml, 1.0 M/THF, 17.20 mmol, 1 eq) was added. The reaction mixture was gradually warmed up to –15 °C over 105 min. Aqueous HCl (1 N, 85 ml), phosphate buffer (pH=7, 200 ml) and saturated aqueous NH4Cl (200 ml) were added to the reaction. The reaction mixture was extracted with EtOAc (200 ml). The organic extract was washed with brine (100 ml), dried over Na2SO4 and concentrated under reduced pressure. The crude product was purified by preparative reverse phase HPLC on a Waters Autopurification system using a Sunfire Prep C18 OBD column (5 μm, 19 × 50 mm; flow rate, 20 ml min−1; Solvent A: H2O with 0.1% HCO2H; Solvent B: CH3CN with 0.1% HCO2H; injection volume: 4.0 ml (CH3CN); gradient: 95→100% B in A over 7 min; UV (350 nm) directed fraction collection). The first 350 nm UV peak was collected and concentrated to give compound 8 diastereomer A (8A) as an orange solid (7.81 g, 43% over three steps) and the second 350 nm UV peak was collected and concentrated to give compound 8 diastereomer B (8B) as an orange solid. A crude sample was also purified by flash column chromatography (5–10% ethyl acetate-hexanes) to give the desired product 8 as a 1:1 mixture of the two diastereomers (pale yellow solid): 1H NMR (400 MHz, CDCl3) δ 15.784, 15.776 (s, 1 H), 7.66 (s, 0.5 H), 7.60 (s, 0.5 H), 7.48–7.57 (m, 8 H), 7.30–7.38 (m, 3 H), 7.09–7.21 (m, 9 H), 5.31–5.39 (m, 2 H), 4.68–4.72 (m, 1 H), 4.05 (d, J=10.4 Hz, 0.5 H), 3.94 (d, J=10.4 Hz, 0.5 H), 3.42–3.50 (m, 1 H), 3.28 (s, 1.5 H), 3.20 (dd, J=4.9, 15.3 Hz, 0.5 H), 2.90–3.07 (m, 4 H), 2.38–2.52 (m, 9 H), 2.10 (d, J=14.0 Hz, 1 H), 1.81–1.91 (m, 1 H), 1.75–1.67 (m, 1 H), 1.60 (s, 4.5 H), 1.59 (s, 4.5 H), 1.43–1.54 (m, 2 H), 0.87 (s, 4.5 H), 0.83 (s, 4.5 H), 0.28 (s, 1.5 H), 0.27 (s, 1.5 H), 0.17 (s, 1.5 H), 0.13 (s, 1.5 H); MS (ESI) m/z 1058.84 (M+H).
(1R,3S,4S,11S)-8-(Benzyloxy)-11-[(tert-butyldimethylsilyl)oxy]-4-(dimethylamino)-12-hydroxy-19-methoxy-10,14-dioxo-18-(pyrrolidin-2-yl)-6-oxa-7-azapentacyclo[11.8.0.03,11.05,9.015,20]henicosa-5(9),7,12,15(20),16,18-hexaen-16-yl tert-butyl carbonate (9)
Compound 8 (72 mg, 1:1 mixture of diastereomers, 0.068 mmol, 1 eq) was dissolved in a pre-mixed solution of 0.5 M HCl in THF (83 μl of 6 N HCl dissolved in 917 μl THF). The reaction solution was stirred at rt for 45 min. Saturated aqueous NaHCO3 was added dropwise until bubbling stopped. Phosphate buffer solution (pH=7) was added. The resulting mixture was extracted with EtOAc (40 ml). The organic extract was dried over Na2SO4 and concentrated to give desired the product 9 as a yellow solid: MS (ESI) m/z 816.72 (M+H). The crude product was used without further purification. Following the same procedure, single diastereomer 9A was prepared from single diastereomer 8A.
(1R,3S,4S,11S)-8-(Benzyloxy)-11-[(tert-butyldimethylsilyl)oxy]-4-(dimethylamino)-12-hydroxy-19-methoxy-18-(1-methylpyrrolidin-2-yl)-10,14-dioxo-6-oxa-7-azapentacyclo[11.8.0.03,11.05,9.015,20]henicosa-5(9),7,12,15(20),16,18-hexaen-16-yl tert-butyl carbonate (10b)
General procedure A: HCHO (37% in water, 1.7 μl, 0.023 mmol, 3 eq), acetic acid (1.3 μl, 0.023 mmol, 3 eq) and sodium triacetoxyborohydride (3.3 mg, 0.015 mmol, 2 eq) were added sequentially to a solution of compound 9 (5.4 mg, 7.7 μmol, 1 eq) in 1,2-dichloroethane (1 ml) at 23 °C. After stirring for 45 min, the reaction mixture was quenched with aqueous potassium phosphate buffer (pH=7.0) and extracted with dichloromethane (15 ml, 10 ml). The combined organic extracts were dried over anhydrous sodium sulfate and concentrated. The crude product was used without further purification. MS (ESI) m/z 830.77 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-8-(1-methylpyrrolidin-2-yl)-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11b)
General procedure B: Aqueous hydrogen fluoride (48–50%, 0.3 ml) was added to a solution of the above intermediate 10b in THF (0.6 ml) in a polypropylene reaction vessel at 23 °C. The mixture was stirred vigorously at 23 °C overnight and poured into aqueous K2HPO4 (3.6 g dissolved in 30 ml water). The mixture was extracted with EtOAc (30 ml, 15 ml). The combined organic phase was dried over anhydrous sodium sulfate and concentrated. The residue was used directly in the next step without further purification. MS (ESI) m/z 616.56 (M+H).
Pd-C (10 wt%, 3 mg) was added in one portion to a solution of the above crude product in a mixture of HCl/CH3OH (0.5 N, 31 μl, 2 eq) and CH3OH (1 ml) at 23 °C. The reaction vessel was sealed and purged with hydrogen by briefly evacuating the flask followed by flushing with hydrogen gas (1 atm). The reaction mixture was stirred under a hydrogen atmosphere (1 atm) at 23 °C for 1 h and filtered through a small Celite pad. The filtrate was concentrated. The residue was purified by preparative reverse-phase HPLC on a Waters Autopurification system using a Phenomenex Polymerx 10 μ RP-γ 100 A column (10 μm, 150 × 21.20 mm; flow rate, 20 ml min−1; Solvent A: 0.05 N HCl/water; Solvent B: CH3CN; injection volume: 3.0 ml (0.05 N HCl/water); gradient: 10→50% B over 15 min; mass-directed fraction collection). Fractions containing the desired product, eluting at 6.5–9.0 min, were collected and freeze-dried to yield compound 11b (2.7 mg, di-HCl salt, 57% for 3 steps): 1H NMR (400 MHz, CD3OD, a mixture of diastereomers) δ 7.07 (s, 0.6 H), 7.02 (s, 0.4 H), 4.80–4.84 (m, 0.6 H), 4.71 (dd, J=7.3, 10.5 Hz, 0.4 H), 4.10 (s, 1 H), 3.79–3.89 (m, 1 H), 3.76 (s, 1.2 H), 3.69 (s, 1.8 H), 3.32–3.36 (m, 1 H), 3.16–3.26 (m, 1 H), 2.97–3.04 (m, 8 H), 2.83, 2.80 (s, 3 H), 2.57–2.63 (m, 1 H), 2.37–2.44 (m, 1 H), 2.14–2.35 (m, 4 H), 1.61–1.71 (m, 1 H); MS (ESI) m/z 528.51 (M+H).
The following compounds were prepared from 9 or 9A and the corresponding aldehydes or ketones by following general procedures A and B.
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-8-[(2S)-pyrrolidin-2-yl]-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11a)
Prepared by deprotection of 9A (34 mg, 0.042 mmol) according to general procedure B (16.1 mg, 65% for 3 steps): 1H NMR (400 MHz, CD3OD, hydrochloride) δ 6.95 (s, 1 H), 4.89–4.82 (m, 1 H), 4.10 (s, 1 H), 3.74 (s, 3 H), 3.49–3.43 (m, 1 H), 3.38–3.32 (m, 1 H), 3.24 (dd, J=4.1, 15.1 Hz, 1 H), 3.04–2.97 (m, 8 H), 2.52-2.47 (m, 1 H), 2.41 (t, J=14.4 Hz, 1 H), 2.29–2.16 (m, 4 H), 1.71–1.61 (m, 1 H); MS (ESI) m/z 514.29 (M+H).
(1R,3S,4S,11S)-8-(Benzyloxy)-11-[(tert-butyldimethylsilyl)oxy]-4-(dimethylamino)-18-[(2S)-1-ethylpyrrolidin-2-yl]-12-hydroxy-19-methoxy-10,14-dioxo-6-oxa-7-azapentacyclo[11.8.0.03,11.05,9.015,20]henicosa-5(9),7,12,15(20),16,18-hexaen-16-yl tert-butyl carbonate (10c)
Compound 8A (7.81 g, 7.38 mmol, 1 eq) was treated with dilute HCl to remove the trityl group. The resulting free amine 9A was dissolved in 1,2-dichloroethane (120 ml) and cooled to 0 °C. Acetic acid (0.85 ml, 14.76 mmol, 2 eq) and sodium triacetoxyborohydride (3.13 g, 14.76 mmol, 2 eq) were added sequentially. Acetaldehyde (0.83 ml, 14.76 mmol, 2 eq) was added via a syringe (pre-cooled with dry ice). The reaction mixture was stirred at 0 °C for 25 min. Saturated aqueous NaHCO3 (300 ml) was added. The reaction mixture was stirred for 20 min and extracted with dichloromethane (400 ml). The organic extract was dried over anhydrous sodium sulfate and concentrated. The residue was purified by flash column chromatography (8–66% ethyl acetate-hexanes) to yield compound 10c as a pale yellow solid (3.45 g, 55% over two steps): 1H NMR (400 MHz, CDCl3) δ 15.73 (s, 1 H), 7.47–7.49 (m, 2 H), 7.30–7.38 (m, 4 H), 5.34 (s, 2 H), 3.97 (d, J=10.4 Hz, 1 H), 3.68 (s, 3 H), 3.63–3.74 (m, 1 H), 3.30–3.43 (m, 1 H), 3.25 (dd, J=4.9, 15.9 Hz, 1 H), 2.94–3.02 (m, 1 H), 2.37–2.56 (m, 10 H), 2.10–2.20 (m, 3 H), 1.80–1.92 (m, 2 H), 1.48–1.62 (m, 2 H), 1.52 (s, 9 H), 0.98–1.02 (m, 3 H), 0.82 (s, 9 H), 0.26 (s, 3 H), 0.12 (s, 3 H); MS (ESI) m/z 844.75 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-8-[(2S)-1-ethylpyrrolidin-2-yl]-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11c)
Compound 10c was deprotected according to general procedure B. Purification on a Si-Cyano column (35 g, eluting with 0.05 N aqueous HCl) yielded the desired compound 11c as a yellow solid (1.33 g, HCl salt, 67% for two steps): 1H NMR (400 MHz, CD3OD, hydrochloride) δ 7.10 (s, 1 H), 4.10 (s, 1 H), 3.81–3.91 (m, 1 H), 3.68 (s, 3 H), 3.32–3.37 (m, 1 H), 3.25 (dd, J=4.6, 15.6 Hz, 1 H), 2.96–3.21 (m, 11 H), 2.55–2.62 (m, 1 H), 2.40 (t, J=14.6 Hz, 1 H), 2.23–2.34 (m, 4 H), 1.61–1.70 (m, 1 H), 1.25 (t, J=7.3 Hz, 3 H); MS (ESI) m/z 542.35 (M+H). A chiral synthesis of 11c (TP-2758) was later developed to support preclinical and clinical development.16
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-8-[(2R)-1-ethylpyrrolidin-2-yl]-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11d)
Prepared from 9B according to similar procedures used for 11c: 1H NMR (400 MHz, CD3OD, hydrochloride) δ 7.20 (s, 1 H), 4.79 (m, 1 H), 4.18 (s, 1 H), 3.92 (m, 1 H), 3.77 (s, 3 H), 3.34–3.37 (m, 1 H), 2.99–3.23 (m, 11 H), 2.58 (m, 1 H), 2.30–2.40 (m, 4 H), 2.13–2.15 (m, 1 H), 1.64–1.66 (m, 1 H), 1.30 (br t, J=7.3 Hz, 3 H); MS (ESI) m/z 542.48 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-8-(1-propylpyrrolidin-2-yl)-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11e)
Prepared from 9 and propionaldehyde according to general procedures A and B. 1H NMR (400 MHz, CD3OD, hydrochloride, a mixture of diastereomers) δ 7.12 (s, 0.67 H), 7.07 (s, 0.33 H), 4.75–4.80 (m, 0.33 H), 4.12 (s, 1 H), 3.82–3.93 (m, 1.67 H), 3.77 (s, 2 H), 3.69 (s, 1 H), 3.34–3.38 (m, 1 H), 2.97–3.27 (m, 11 H), 2.55–2.63 (m, 1 H), 2.12–2.48 (m, 5 H), 1.62–1.74 (m, 3 H), 0.87–0.93 (m, 3 H); MS (ESI) m/z 556.55 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-8-[1-(propan-2-yl)pyrrolidin-2-yl]-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11f)
Prepared from 9 and acetone according to general procedures A and B. 1H NMR (400 MHz, CD3OD, hydrochloride, a mixture of diastereomers) δ 7.13 (s, 0.55 H), 7.08 (s, 0.45 H), 4.07 (s, 1 H), 3.75 (s, 1.35 H), 3.64 (s, 1.65 H), 3.58–3.64 (m, 1 H), 3.38–3.46 (m, 2 H), 2.93–3.20 (m, 10 H), 2.54–2.55 (m, 1 H), 2.04–2.39 (m, 5 H), 1.58–1.68 (m, 1 H), 1.22–1.30 (m, 6 H); MS (ESI) m/z 556.59 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-8-[1-(2-methylpropyl)pyrrolidin-2-yl]-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11g)
Prepared from 9 and isobutyraldehyde according to general procedures A and B. 1H NMR (400 MHz, CD3OD, hydrochloride, a mixture of diastereomers) δ 7.17 (s, 0.5 H), 7.10 (s, 0.5 H), 4.78-4.82 (m, 1 H), 4.12 (s, 1 H), 3.89-4.00 (m, 1 H), 3.78 (s, 1.5 H), 3.69 (s, 1.5 H), 3.34-3.41 (m, 1 H), 3.15-3.26 (m, 1 H), 2.84-3.09 (m, 9 H), 2.55-2.60 (m, 1 H), 2.40 (t, J=14.6 Hz, 1 H), 2.12-2.34 (m, 4 H), 1.94-2.02 (m, 1 H), 1.61-1.70 (m, 1 H), 0.88-0.98 (m, 6 H); MS (ESI) m/z 570.58 (M+H).
(4S,4aS,5aR,12aS)-8-[1-(Cyclopropylmethyl)pyrrolidin-2-yl]-4-(dimethylamino)-3,10,12,12a-tetrahydroxy-7-methoxy-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11h)
Prepared from 9 and 2-cyclopropylacetaldehyde according to general procedures A and B. 1H NMR (400 MHz, CD3OD, hydrochloride, a mixture of diastereomers) δ 7.11 (s, 0.5 H), 7.06 (s, 0.5 H), 4.76–4.83 (m, 1 H), 4.11 (s, 1 H), 3.91–4.02 (m, 1 H), 3.75 (s, 1.5 H), 3.68 (s, 1.5 H), 3.40–3.46 (m, 1 H), 3.14–3.27 (m, 1 H), 2.92–3.12 (m, 9 H), 2.57–2.61 (m, 1 H), 2.12–2.43 (m, 5 H), 1.60–1.70 (m, 1 H), 0.98–1.03 (m, 1 H), 0.60–0.66 (m, 2 H), 0.33–0.40 (m, 1 H), 0.20–0.27 (m, 1 H); MS (ESI) m/z 568.58 (M+H).
(1R,3S,4S,11S)-8-(benzyloxy)-11-[(tert-butyldimethylsilyl)oxy]-4-(dimethylamino)-12-hydroxy-18-[(2S)-1-(2-hydroxyethyl)pyrrolidin-2-yl]-19-methoxy-10,14-dioxo-6-oxa-7-azapentacyclo[11.8.0.03,11.05,9.015,20]henicosa-5(9),7,12,15(20),16,18-hexaen-16-yl tert-butyl carbonate (10i)
General procedure C: K2CO3 (7 mg, 0.050 mmol, 1.2 eq), NaI (1.3 mg, 0.008 mmol, 0.2 eq) and bromoethanol (3.3 μl, 0.046 mmol, 1.1 eq) were added to a solution of 9A (34 mg, 0.042 mmol, 1.0 eq) in THF (1 ml) at rt. The reaction mixture was heated at 50 °C for 2 h. Additional bromoethanol (5.0 μl, 0.070 mmol, 1.7 eq) was added and the reaction mixture was heated at 60 °C for 2 days. The reaction mixture was cooled to rt, diluted with EtOAc (30 ml) and washed with phosphate buffer (pH=7, 20 ml) and brine (20 ml). The resulting organic phase was dried over Na2SO4, filtered and concentrated under reduced pressure. The crude product was purified by preparative reverse-phase HPLC on a Waters Autopurification system using a Sunfire Prep C18 OBD column (5 μm, 19 × 50 mm; flow rate, 20 ml min−1; Solvent A: H2O with 0.1% HCO2H; Solvent B: CH3CN with 0.1% HCO2H; injection volume: 2.0 ml (CH3CN); gradient: 10→100% B in A over 15 min; mass-directed fraction collection). Fractions with the desired MW, eluting at 8.6–9.5 min, were collected and concentrated on a RotaVap at rt to remove most of the acetonitrile. The resulting mostly aqueous solution was neutralized with saturated NaHCO3 solution and extracted with EtOAc. The organic extract was dried over Na2SO4 and concentrated to yield the desired product 10i (9.3 mg, 26%): 1H NMR (400 MHz, CDCl3) δ 16.20 (br s, 1 H), 7.50–7.46 (m, 4 H), 7.39–7.25 (m, 7 H), 5.35 (s, 2 H), 5.19 (ABq, J=12.8, 16.5 Hz, 2 H), 4.01 (d, J=10.4 Hz, 1 H), 3.88–3.82 (m, 1 H), 3.64 (s, 3 H), 3.67–3.61 (m, 2 H), 3.49–3.41 (m, 2 H), 3.24 (dd, J=4.3, 15.9 Hz, 1 H), 2.96–2.90 (m, 1 H), 2.78–2.72 (m, 1 H), 2.54–2.42 (m, 8 H), 2.35–2.17 (m, 3 H), 2.11 (d, J=14.0 Hz, 1 H), 1.79–1.87 (m, 2 H), 1.62–1.49 (m, 1 H), 1.40–1.39 (m, 1 H), 0.84 (s, 9 H), 0.27 (s, 3 H), 0.14 (s, 3 H); MS (ESI) m/z 850.53 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-8-[(2S)-1-(2-hydroxyethyl)pyrrolidin-2-yl]-7-methoxy-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11i)
Compound 11i was obtained by deprotection of compound 10i according to general procedure B: 1H NMR (400 MHz, CD3OD, hydrochloride) δ 7.14 (s, 1 H), 4.94-4.87 (m, 1 H), 4.10 (s, 1 H), 3.98–3.92 (m, 1 H), 3.80–3.66 (m, 2 H), 3.69 (s, 3 H), 3.44–3.37 (m, 1 H), 3.25 (dd, J=4.6, 15.6 Hz, 1 H), 3.20–3.17 (m, 2 H), 3.07–2.97 (m, 8 H), 2.61–2.54 (m, 1 H), 2.41 (t, J=14.4 Hz, 1 H), 2.35–2.21 (m, 4 H), 1.71–1.61 (m, 1 H); MS (ESI) m/z 558.27 (M+H).
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-3,10,12,12a-tetrahydroxy-8-[(2S)-1-(3-hydroxypropyl)pyrrolidin-2-yl]-7-methoxy-1,11-dioxo-1,4,4a,5,5a,6,11,12a-octahydrotetracene-2-carboxamide (11j)
Prepared from 9A and bromopropanol according to general procedures C and B: 1H NMR (400 MHz, CD3OD, hydrochloride) δ 7.09 (s, 1 H), 4.92–4.88 (m, 1 H), 4.10 (s, 1 H), 3.92–3.86 (m, 1 H), 3.70 (s, 3 H), 3.63–3.50 (m, 2 H), 3.38–3.32 (m, 1 H), 3.25–3.17 (m, 3 H), 3.04–2.97 (m, 8 H), 2.62–2.57 (m, 1 H), 2.41 (t, J=14.4 Hz, 1 H), 2.36–2.22 (m, 4 H), 1.85–1.82 (m, 2 H), 1.71–1.62 (m, 1 H); MS (ESI) m/z 572.30 (M+H).
Biology.
In vitro microbiology
Minimum inhibitory concentration assays were performed following Clinical Laboratory Standards Institute standards15 for broth microdilution susceptibility assays in cation-adjusted Mueller–Hinton broth (BD, Franklin Lakes, NJ), Haemophilus Test Medium (HTM, Remel, San Diego, CA), or cation-adjusted Mueller–Hinton broth with 5% lysed horse blood (Quad Five, Ryegate, MT, USA) as required. Species-appropriate control antibiotics from commercial sources (Sigma Aldrich, St Louis, MO; VWR, Radnor, PA, USA) and media-appropriate ATCC quality-control strains were used on each test day. Assays were performed in-house at Tetraphase Pharmaceuticals or at Eurofins Medinet (Chantilly, VA, USA). For in-house testing, isolates were sourced from Eurofins Medinet, International Health Management Associates (Schaumburg, IL), Walter Reed Army Institute of Research (Silver Spring, MD, USA), Centers for Disease Control (Atlanta, GA, USA), the Network on Antimicrobial Resistance in S. aureus (Manassas, VA, USA), the University of Calgary (Calgary, AL, Canada) and the laboratory of Marilyn Roberts at the University of Washington (Seattle, WA, USA). Strain resistance classifications were based upon PCR and sequencing characterizations performed at Tetraphase Pharmaceuticals and/or the strain sources.
Animal studies
All efficacy and pharmacokinetic studies were performed using approved institutional animal care and use committee protocols and conforming to Office of Laboratory Animal Welfare standards.
TP-2758 in vivo efficacy testing
In vivo efficacy models were conducted by Vivisource Labs (Waltham, MA, USA) as previously described.23 Pathogen-free female mice, CD-1 or BALB/c, purchased from Charles River Laboratories, Inc. (Wilmington, MA, USA), were acclimated for a minimum of 5 days prior to the start of the studies. The animals had free access to food and water throughout the study. Compounds were dosed i.v. in sterile saline via tail vein, or orally (PO) in sterile water via gavage, unless otherwise noted.
For the murine sepsis screening model, inoculation of S. aureus ATCC 13709 were optimized to achieve an inoculum that resulted in 100% mortality within 48 h when infected by the intraperitoneal route with 0.5 ml of inoculum. Six CD-1 mice per group received a single treatment of either PO (30 mg kg−1) or i.v. (3 mg kg−1) 1 h after infection.
For the murine pyelonephritis infection models, six BALB/c mice per group were challenged with either tetracycline-resistant E. coli strain uropathogenic EC200 or K. pneumoniae KP453 via tail vein intravenous injection of an inoculum of 1.3 × 108 to 1.6 × 08 CFU per mouse for E. coli, or 9.5 × 105 to 9.9 × 105 CFU per mouse in 0.2% carageenen (Sigma Aldrich) for K. pneumoniae, in 0.2 ml. For the E. coli pyelonephritis model, animals were dosed at 12 and 24 h post infection with either TP-2758 (5 mg kg−1 i.v. or 2 mg kg−1 PO, in 0.5% methylcellulose/0.2% Tween 80 (MCT)), levofloxacin (2 mg kg−1 i.v. or 2 mg kg−1 PO, in MCT), or vehicle. For the K. pneumoniae pyelonephritis model, animals were dosed at 9 and 24 h post infection with TP-2758 (20 mg kg−1 i.v. or 50 mg kg−1 PO) or vehicle; meropenem/cilastatin was dosed either at 30/30 mg kg−1 i.v. at 9 and 24 h, or at 20/20 mg kg−1 PO at 6, 15 and 24 h post infection. At 36 h post initiation of treatment, mice were killed by CO2 inhalation and the kidneys of mice were aseptically removed, weighed, homogenized, serially diluted and plated on tryptic soy agar plates. Plates were incubated overnight at 37 °C in 5% CO2. Colonies were enumerated and CFU per gram of tissue was calculated and data graphed using GraphPad Prism (version 4.03, GraphPad Software, Inc., La Jolla, CA, USA).
For the lung infection models, neutropenia was induced as previously described23 and six to eight BALB/c mice per group were challenged intranasally under light anesthesia with tetracycline-resistant MRSA SA191 or S. pneumoniae SP160 using an inoculum of 5.0 × 107 to 5.5 × 107 CFU per mouse for MRSA, or 4.6 × 106 to 8.5 × 106 CFU per mouse for S. pneumoniae (50 μl). For the MRSA model, animals were dosed at 2 and 12 h post infection with TP-2758 (10 mg kg−1 i.v. or 50 mg kg−1 PO), linezolid (30 mg kg−1 i.v. or 30 mg kg−1 PO) or vehicle. For the S. pneumoniae model, animals were dosed at 2 and 12 h post infection with TP-2758 (10 mg kg−1 i.v. or 30 mg kg−1 PO), linezolid (30 mg kg−1 PO), or vehicle. Twenty-four hours post initiation of treatment, mice were killed by CO2 inhalation. The lungs of the mice were aseptically removed, weighed, homogenized, serially diluted and plated on tryptic soy agar plates. The plates were incubated overnight at 37 °C in 5% CO2. Colonies were enumerated and CFU per gram of tissue was calculated and data graphed using GraphPad Prism (version 4.03).
TP-2758 pharmacokinetic studies
Pharmacokinetic studies were performed at WuXi Apptec (Suzhou, China). TP-2758 was evaluated in fasted (no food for 18 h before dosing) male Sprague–Dawley rats (each dose group had three animals) by administration of 1 mg kg−1 intravenously into the jugular vein and 10 mg kg−1 by oral gavage. Ten plasma samples were drawn for each dosing route up to 24 h into heparin-coated vacutainer tubes. The plasma concentration of the compound was quantified by LC/MS/MS using an internal standard. Quality control samples (low, medium and high) and standard curves (in duplicate) were included in the bioanalytical run. Dose formulations were verified with a five-point calibration curve. WinNonLin (v. 5.2, Pharsight Corp., Sunnyvale, CA, USA) was used to determine individual and mean pharmacokinetics parameters±s.d.
TP-2758 was evaluated in three non-naive cynomolgus monkeys. Each animal received a single i.v. dose of 1 mg kg−1 and after a 7-day washout a single PO dose of 10 mg kg−1. Nine to 10 plasma samples were drawn for each dosing route up to 24 h into heparin-coated vacutainer tubes. Urine was collected from the i.v. dose group over ice at intervals before dosing (pre-dose), 0–8 and 8–24 h post dose. Dose formulations were verified with a five-point calibration curve. The plasma and urine concentration of the compound was quantified by LC/MS/MS using an internal standard. Quality control samples (low, medium and high; minimum of six standards with LLOQ<3 ng ml−1) and standard curves (in duplicate) were included in the bioanalytical run. WinNonLin (v. 5.2) was used to determine individual and mean pharmacokinetics parameters±s.d.

Synthesis of 7-methoxy-8-pyrrolidinyl tetracycline. Tetracycline analogs with several other C8 heterocyclic side chains including fused and bridged azabicyclo-ring systems 28 and 35, as well as piperidinyl analogs 42 and morpholinyl analogs 49, were prepared via similar approaches. The corresponding synthetic schemes are included in the Supplementary Information.
References
Centers for Disease Control and Prevention (CDC) 2013 Antibiotic resistance threats in the United States, 2013 http://www.cdc.gov/drugresistance/threat-report-2013.
The PEW Charitable Trusts Antibiotics currently in clinical development. December 2016 http://www.pewtrusts.org/~/media/assets/2016/12/antibiotics_datatable_201612.pdf?la=en.
Cain, R., Narramore, S., McPhillie, M., Simmons, K. & Fishwick, C. W. Applications of structure-based design to antibacterial drug discovery. Bioorg. Chem. 55, 69–76 (2014).
Katz, L. & Baltz, R. H. Natural product discovery: past, present, and future. J. Ind. Microbiol. Biotechnol. 43, 155–176 (2016).
Silver, L. L. Natural products as a source of drug leads to overcome drug resistance. Future Microbiol. 10, 1711–1718 (2015).
Charest, M. G., Lerner, C. D., Brubaker, J. D., Siegel, D. R. & Myers, A. G. A convergent enantioselective route to structurally diverse 6-deoxytetracycline antibiotics. Science 308, 395–398 (2005).
Charest, M. G., Siegel, D. R. & Myers, A. G. Synthesis of (–)-tetracycline. J. Am. Chem. Soc. 127, 8292–8293 (2005).
Sun, C. & Xiao, X.-Y. in Topics in Medicinal Chemistry. Fully synthetic tetracyclines: increasing chemical diversity to combat multidrug-resistant bacterial infections. In: Fisher, J. F. (eds). in press (Springer International Publishing AG 2017) (e-pub ahead of print 5 May 2017, doi: 10.1007/7355_2017_11).
Deng, Y et al. Heterocyclyl tetracyclines. 1. 7-Trifluoromethyl-8-pyrrolidinyltetracyclines: potent, broad spectrum antibacterial agents with enhanced potency against Pseudomonas aeruginosa. J. Med. Chem. 60, 2498–2512 (2017).
World Health Organization Global priority list of antibiotic-resistant bacteria to guide research, discovery and development of new antibiotics (2017) http://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf?ua=1.
Clark, R. B. et al. Synthesis and biological evaluation of 8-aminomethyltetracycline derivatives as novel antibacterial agents. J. Med. Chem. 56, 8112 (2013).
Xiao, X.-Y. et al. Fluorocyclines. 1. 7-Fluoro-9-pyrrolidinoacetamideo-6-demethyl-6-deoxytetracycline: a potent, broad spectrum antibacterial Agent. J. Med. Chem. 55, 597 (2012).
Brubaker, J. D. & Myers, A. G. A practical, enantioselective synthetic route to a key precursor to the tetracycline antibiotics. Org. Lett. 9, 3523 (2007).
Zhang, W.-Y. et al. Process research and development of TP-808: a key intermediate for the manufacture of synthetic tetracyclines. Org. Process Res. Dev. 21, 377 (2017).
Clinical Laboratory Standards Institute (CLSI) in: Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard, 8th edn, (Vol 20), no. 2. CLSI document M07-A8., vol. CLSI, 940 West Valley Road, Suite 1400 (Clinical Lab Standards Institute, Wayne, Pennsylvania, 2009).
Zhang, W.-Y. et al. Process development and scale-up of fully synthetic tetracycline TP-2758: a potent antibacterial agent with excellent oral bioavailability. Org. Process Res. Dev. 20, 284 (2016).
Sum, P.-E. et al. Glycylcyclines. 1. A new generation of potent antibacterial agents through modification of 9-aminotetracyclines. J. Med. Chem. 37, 184 (1994).
Orth, P. et al. Crystallization and preliminary X-ray analysis of the Tet-repressor/operator complex. Acta Crystallogr. Set. D. Biol. Crystallogr. D54, 99 (1998).
Kumarasamy, K. K. et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. 2010. Lancet Infect. Dis. 10, 597 (2010).
Nordmann, P., Naas, T. & Poirel, L. Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg. Infect. Dis. 17, 1791 (2011).
Boyle-Vavra, S. & Daum, R. S. Community-acquired methicillin-resistant Staphylococcus aureus: the role of Panton-Valentine leukocidin. Lab. Invest. 87, 3 (2007).
Agwuh, K. N. & MacGowan, A. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J. Antimicrob. Chemother. 58, 256 (2006).
Grossman, T. H., Murphy, T. M., Slee, A. M., Lofland, D. & Sutcliffe, J. A. Eravacycline (TP-434) is efficacious in animal models of infection. Antimicrob. Agents Chemother. 59, 2567 (2015).
Acknowledgements
This paper is dedicated to Professor Kyriacos C. Nicolaou. We are grateful to Professor Andrew Myers, Dr Eric Gordon and Dr Joaquim Trias for valuable discussions. We are also grateful to Dr Shu-hui Chen and his colleagues at WuXi AppTec for external chemistry support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on The Journal of Antibiotics website
Supplementary information
Rights and permissions
About this article
Cite this article
Sun, C., Deng, Y., Hunt, D. et al. Heterocyclyl tetracyclines. 2. 7-Methoxy-8-pyrrolidinyltetracyclines: discovery of TP-2758, a potent, orally efficacious antimicrobial against Gram-negative pathogens. J Antibiot 71, 287–297 (2018). https://doi.org/10.1038/ja.2017.86
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2017.86