Abstract
Crotalicidin (Ctn), a 34-residue cathelicidin from a South American rattlesnake, and its fragment (Ctn[15–34]) have shown anti-infective and cytotoxic activities against Gram-negative bacteria and certain tumor lines, respectively. The extent of such effects has been related to physicochemical characteristics such as helicity and hydrophobicity. We now report the anti-fungal activity of Ctn and its fragments (Ctn[1–14]) and (Ctn[15–34]). MIC determination and luminescent cell viability assays were used to evaluate the anti-infective activity of Ctn and its fragments (Ctn[1–14]) and (Ctn[15–34]) as anti-fungal agents against opportunistic yeast and dermatophytes. Cytotoxicity towards healthy eukaryotic cells was assessed in vitro with healthy human kidney-2 (HK-2) cells and erythrocytes. The checkerboard technique was performed to estimate the effects of combining either one of the peptides with amphotericin B. Ctn was the most active peptide against dermatophytes and also the most toxic to healthy eukaryotic cells. Fragments Ctn[1–14] and Ctn[15–35] lost activity against dermatophytes, but became more active against pathogenic yeasts, including several Candida species, both clinical isolates and standard strains, with MICs as low as 5 μm. Interestingly, the two peptide fragments were less cytotoxic to healthy HK-2 cells and less hemolytic to human erythrocytes than the standard-of-care amphotericin B. Also noteworthy was the synergy between Ctn peptides and amphotericin B, with consequent reduction in MICs of both drug and peptides. Altogether, Ctn and its fragments, particularly Ctn[15–34], are promising leads, either alone or in combined regimen with amphotericin B, for the treatment of fungal diseases.
Similar content being viewed by others
Introduction
Human mycoses are caused by primary pathogenic fungi that invade the tissues of a healthy host, or by opportunistic fungi that invade the tissues of individuals with severe alterations in the immune system. Dermatomycosis is one of the most frequent dermal lesions that affect humans and animals, and is often caused by dermatophytes of the genera Epidermophyton, Microsporum and Trichophyton. These fungi infect keratinized tissue such as skin, nails and scalp, causing lesions characterized by irritation, scaling, local redness, swelling and inflammation.1, 2 In addition, some dermatomycoses may be associated with the presence of opportunistic yeast pathogens, including the genus Candida, that can quickly colonize damaged nails or skin, especially the mucous membranes.3
Candidemia and other forms of invasive candidiasis are unquestionably the most prevalent among invasive mycoses worldwide. Candida species belong to the normal microbiota of an individual’s mucosal oral cavity, gastrointestinal tract and vagina, and are responsible for various clinical manifestations from mucocutaneous overgrowth to bloodstream infections.4
The pathogenicity of Candida species is attributed to capabilities such as adherence and biofilm formation (on host tissues and on medical devices), as well as to production of tissue-damaging enzymes (proteases, phospholipases, hemolysins) and other virulence factors that allow the fungus to evade host defenses.5 The risk of candidiasis is increased by underlying malignancies such as immunosuppressive diseases, hematopoietic stem cell or solid organ transplantation, the use of wide-spectrum antibiotics or corticosteroids, invasive interventions, aggressive chemotherapy, parenteral nutrition alimentation and contaminated internal prosthetic devices.6 The situation is worsened by the rapid development of resistance against many currently used anti-fungals—e.g., fluconazole, itraconazole and amphotericin B (AMB)—that can seriously compromise anti-fungal therapies. Therefore, the discovery and the development of new anti-fungals is a pressing, urgent need.7, 8
Prospective therapeutic application of anti-microbial peptides (AMPs) has received much attention recently, because of their broad spectrum of activity and reduced likelihood of inducing resistance.9 AMPs are gene-encoded products made by the innate immune cells of plants and animals and acting as a first line of defense against invading pathogens. Also called host defense peptides, their primary mechanism of action is the destabilization of pathogen membranes, mainly by electrostatic interaction between the cationic AMP and negatively charged cell wall/membrane components such as phospholipids, teichoic acids and lipopolysaccharides in bacteria,10, 11 and mannoproteins or membrane-bound enzymes such as β-glucan and chitin synthases in fungi.12 Recent studies have also pointed out that AMPs may act on intracellular targets such as nucleic acids and/or components of the protein synthesis machinery,13 as well as on organelles such as the mitochondria, where apoptosis can be initiated.14 Moreover, AMPs can have an important role as multieffector immunomodulatory agents connecting innate and adaptive immunity responses. For example, in an epithelial invasion by Candida hyphae, AMPs such as β-defensins, alarmins and cathelicidins stimulate immune cells to secrete chemotactic proteins to recruit other immune cells to fight the pathogen. Once the pathogen is eliminated, AMPs also contribute to promote epithelial remodeling and barrier repair.15, 16, 17
Cathelicidins are among the most important classes of AMPs. Found in the tissue of organisms of distinct phyla, from primitive hagfish to humans, all cathelicidins share in common a conserved N-terminal preproregion containing the signal peptide and a cathelin—cathepsin L inhibitor—domain. The anti-microbial activity is confined to a variable C-terminal domain (mature sequence) that is released by proteolysis at an inflammatory site. Distinct cathelicidin precursors generate diverse peptide sequences that can adopt different secondary structures such as α-helixes, β-hairpins, dimeric β-hairpins and linear non-α-helixes.18, 19 The in vitro efficiency of cathelicidins as anti-bacterial agents has been extensively and systematically documented. In contrast, the anti-fungal activity of these peptides is less well defined, and has not yet been comparatively evaluated, although there is sufficient evidence that they should also be effective in this respect.20, 21 Examples include the porcine protegrins and human cathelicidin hCAP18/LL-37, the only human multieffector cathelicidin reported to date.22, 23
In previous studies, cathelicidin precursors from the venom glands of South American pit vipers were reported. These precursors encode mature cathelicidin-like sequences, named collectively vipericidins (cathelicidins from pit vipers), that display good anti-bacterial activities, especially against Gram-negative species, as well as low cytotoxic profiles.24 More recently, one of these vipericidins—i.e., crotalicidin (Ctn) from the South American rattlesnake Crotalus durissus terrificus—was structurally and functionally dissected into two fragments, termed Ctn[1–14] and Ctn[15–34]. Although Ctn[1–14] kept the α-helical structure of Ctn, it lost all anti-bacterial and anticancer activity of the parental peptide. On the other hand, largely random coil Ctn[15–34] preserved the anti-bacterial and anticancer activities of Ctn, with much lower toxicity to healthy eukaryotic cells than the full sequence.25
Herein, we have continued the anti-infective evaluation of Ctn and its fragments (Ctn[1–14] and Ctn[15–34]) by assessing their anti-fungal activities on different opportunistic yeast and dermatophyte strains. Ctn was the most active peptide against dermatophytes and also the most toxic to eukaryotic cells, while the two fragments, especially Ctn[15–34], were less toxic and more active against yeasts. When combined with a standard anti-fungal such as AMB, the doses of both Ctn[15–34] and AMB could be significantly reduced, their synergy providing a basis for an efficient and safe chemotherapy against invasive mycoses.
Materials and methods
Peptides
Ctn (KRFKKFFKKVKKSVKKRLKKIFKKPMVIGVTIPF-amide) and its fragments (Ctn[1–14] (KRFKKFFKKVKKSV-amide) and Ctn[15–34] (KKRLKKIFKKPMVIGVTIPF-amide)) were prepared by solid-phase synthesis, purified by HPLC and characterized by MS analysis, as reported previously.24, 25 For all experiments, 1 mm peptide stock solutions were prepared by weighting and dissolving in deionized water the right amount of each peptide to give a final concentration of 1 mm. Peptide stock solutions were stored at 4 °C for up to 6 weeks. Physicochemical properties such as net charge at neutral pH, hydrophobicity and hydrophobic moment of Ctn, Ctn[1–14] and Ctn[15–34], were obtained by the ‘Peptide property calculator’ (http://www.pepcalc.com) and ‘Heliquest’ (http://heliquest.ipmc.cnrs.fr/) softwares.
Fungi
The yeast and dermatophyte strains used in this study were kindly donated by Santa Casa de Misericordia Hospital at Sobral (Ceara, Brazil). Identification of yeast strains was performed with CHROMagar-Candida (CHROMagar Company, Paris, France) in a VITEK 2-automated system (BioMerieux, Marcy-l'Étoile, France) with YST card. The dermatophyte strains were identified by their morphological characteristics and biochemical profiles. Yeast strains were grown on Sabouraud agar plates at 30 °C for 48 h. Inoculum suspensions were prepared by picking and suspending five colonies in 5 ml of sterile phosphate-buffered saline (PBS) (phosphate 35 mm, NaCl 150 mm, pH 7.4). Dermatophytes were grown on Sabouraud agar slants at 30 °C for 7 days. The fungal colonies were then covered with 3 ml of PBS and gently scraped with a sterile pipette. The resulting suspensions were transferred to sterile tubes, and heavy particles were allowed to settle. The turbidity of the conidial spore suspensions was measured at 600 nm and was adjusted to obtain an appropriate inoculum.
Anti-fungal assays
The MICs of the peptides against the fungal strains were determined by the broth microdilution method, based essentially on documents M27-A326 and M38-A227 for yeasts and dermatophytes, respectively, from the Clinical and Laboratory Standards Institute (CLSI). Determination of these MICs for all fungal strains was carried out in 96-well microtiter plates (E & K Scientific, Santa Clara, CA, USA). The peptide stock solutions (at 1 mm) were prepared as above and used to make twofold serial dilutions with RPMI-1640 medium to a final volume of 100 μl per well. Subsequently, 100 μl of fungal suspension, containing 2 × 106 CFU ml−1 (equivalent to 0.5 in the McFarland’s scale), in RPMI were added to each well. Final peptide concentrations ranged from 0.0195 to 40 μm. AMB and ketoconazole (Sigma Chemical, St Louis, MO, USA) were used as controls for yeasts and dermatophytes, respectively. MIC was defined as the lowest peptide concentration at which no fungal growth was visually observed after 48 h at 30 °C for yeasts and after 5 days at room temperature for dermatophytes.
Microbial cell viability assays
After MIC determination, Ctn, Ctn[1–14], Ctn[15–34] and AMB were incubated again with the yeast strains (Cryptococcus laurentii and Candida spp.). The yeast suspensions (100 μl) containing 2 × 106 CFU ml−1 were added to 100 μl of peptide dilutions in 96-well microtiter plates, with final peptide and AMB concentrations in the 2.5–40 and 0.06–1 μm range, respectively. After 48 h incubation at 30 °C, 100 μl of BacTiter-Glo (Promega, Madison, WI, USA) was added to each well and plates were reincubated for 15 min at room temperature with gentle shaking. Luminescence was then measured in a Synergy HT (BioTek, Winooski, VT, USA) multidetection microplate reader. Untreated yeast suspensions were used as positive controls and wells containing only RPMI-1640 medium were used to obtain background luminescence values. The assays were carried out in triplicate.
Cell culture
The healthy human kidney-2 (HK-2) cell lineage was obtained from the Cancer Cell Line Repository of the Institute Municipal d’Investigaciò Mèdica (IMIM) at the Barcelona Biomedical Research Park (Barcelona, Spain). Cells were cultured in RPMI-1640 medium supplemented with fetal bovine serum 10%, penicillin/streptomycin 1%, l-glutamine 1% and ITS-G (insulin-transferin-selenium) 0.5% solutions, and maintained in T-75 cm2 flasks at 37 °C in a humidified atmosphere with 5% CO2. Cells were subcultured every time they reached 80–90% confluence after being harvested with a solution of trypsin 0.25% and EDTA 2.21 mm.
Evaluation of potential peptide nephrotoxicity
HK-2 cells (5 × 103 per well) were seeded in 96-well plates. After 24 h incubation at 37 °C and 5% CO2, the medium was removed and new medium containing fetal bovine serum 2% and either peptides or AMB in twofold serial dilutions (0.39–400 μm) was added. After an additional 30 min incubation, 15 μl of Cell Titer Blue (Promega) were added to each well and plates were reincubated for 24 h. Fluorescence intensity was then measured at λem=590 and λex=530 nm in a Synergy HT (BioTek) reader. Relative HK-2 cell viability was calculated with cells treated with only RPMI-1640 containing 2% fetal bovine serum as controls, and the assays were carried out in triplicate.
Hemolytic activity
Fresh blood (10 ml) was collected in EDTA tubes and centrifuged at 1000 g for 10 min at 4 °C. After plasma removal, the pellet containing red blood cells was washed five times with PBS and resuspended in PBS to obtain an 8% (v v−1) suspension. One hundred microliters of aliquots of this suspension were added to different microcentrifuge tubes, each containing 100 μl of twofold serially diluted peptides or AMB, ranging from 0.2 to 200 μm. The final concentrations were as follows: erythrocyte (red blood cell) suspension 4% (v v−1) and 0.1–100 μm of peptides or AMB. These resulting suspensions were incubated with agitation for 1 h at 37 °C. After incubation, samples were centrifuged for 2 min at 1000 g. Supernatants were transferred to 96-well plates and hemoglobin release was measured at 540 nm in a Synergy HT (Biotek) reader. Triton X-100 1% and untreated red blood cells 4% (v v−1) in PBS were used as positive and negative controls, respectively. Percentage hemolysis was calculated as ((OD540 nm (treated)−OD540 nm (untreated)/(OD540 nm (Triton X-100-treated)−Abs540nm (untreated)) × 100, and experiments were carried out in triplicate.
Checkerboard assays
The anti-fungal activity of Ctn, Ctn[1–14] and Ctn[15–34] peptides when combined with AMB was determined by the checkerboard technique, a method used to estimate drug interaction by calculating the fractional inhibitory concentration (FIC) index. In 96-well microtiter plates, 50 μl of fungal suspensions (with 2 × 106 CFU ml−1≈0.5 in the McFarland’s scale) in RPMI medium were added to wells containing twofold serial dilutions of one of the peptides and AMB in the same final concentration ranges (0.0195–40 μm peptides, 0.0312–16 μm AMB) as previously used for the MIC determination. Cells treated with either peptides or AMB alone, at their respective MIC values, along with untreated fungal suspensions were used as controls. After 48 h incubation at 30 °C, results were visually observed and the FIC index (FICI) was calculated as FICI=FICP+FICA, where ‘P’ represents peptides (Ctn or Ctn[1–14] or Ctn[15–34]) and ‘A’ AMB. FICP, in turn, was calculated as the MICP (combined)/MICP (alone) ratio, whereas FICA was calculated as the MICA (combined)/MICA (alone) ratio. Drug interaction was classified as synergism if FICI⩽0.5; no interaction when 0.5
Results and discussion
Ctn, Ctn[1–14] and Ctn[15–34] peptides
Ctn and its fragments (Ctn[1–14] and Ctn[15–34])24, 25 were obtained by solid-phase synthesis in high purity (>95% by HPLC) and with the expected molecular weights as determined by LC-MS and summarized in Table 1. Some physicochemical properties, such as their secondary structures, hydrophobicities, hydrophobic moments and net charge (at neutral pH) are also listed in Table 1, which will be useful for later insights on structure–activity relationships.
Anti-fungal activity
The in vitro anti-fungal activities of Ctn and its fragments (Ctn[1–14] and Ctn[15–34]) against standard and clinical isolates of yeasts and dermatophytes were determined as MIC values (Table 2). As to controls, AMB showed MIC values ranging from 0.5 to 2 μm (0.265–1.85 μg ml−1) for yeasts and ketoconazole from 0.25 to 0.5 μm (0.133–0.265 μg ml−1) for dermatophytes.
Ctn showed differing activities towards the various fungal types. On the one hand, it was the only peptide with significant MIC values for the three dermatophyte strains, in the low micromolar range (1.25 μm against Microsporum canis and 5 μm against both Trichophyton rubrum strains). On the other hand, it needed higher concentrations (from 10 to above 40 μm, the highest concentration tested) to inhibit yeast growth. For their part, fragments Ctn[1–14] and Ctn[15–34] differed substantially from Ctn in anti-fungal activities. Thus, while both fragments were basically inactive against dermatophytes, toward yeasts they had, in general, better MIC values compared with the parental peptide. In particular, Ctn[15–34], with MICs ranging mostly from 5 to 10 μm (11.85–23.7 μg ml−1), was the best-performing peptide against yeasts, with MIC values only slightly higher (2.5-fold, on a molar basis) compared with the AMB control against clinically isolated strains of Candida albicans, Candida parapsilosis and Candida tropicalis.
As previously found for bacteria24, 25 (also see Table 1), it appears that the full-sized (MW=4151) and highly charged (+16) Ctn can interact better with the cell wall and membranes of dermatophytes than with those of yeasts. In contrast, the highly α-helical Ctn[1–14], over 50% shorter (MW=1797) and with about half the net charge (+9) of Ctn, while practically inert against dermatophytes, performed better against yeasts. For its part, the mid-size (MW=2371), mainly unstructured Ctn[15–34]25 was the peptide targeting more efficiently yeast membranes, cell wall and/or—in the case of C. laurentii—the glycoprotein capsule.
It is worth noting that, despite a net charge (+8) similar to Ctn[1–14], Ctn[15–34] has the highest hydrophobicity (H=0.455) and the lowest hydrophobic moment (μH=0.311) among all three peptides. Other factors, in addition to secondary structures (α-helix or random coil) and/or physicochemical properties, that may account for the different peptide anti-infective activities against fungal strains may be the various fungal morphologies, as observed for small drugs.30 In this study, the growth conditions used gave rise to diverse dermatophyte forms, such as macroconidia, microconidia and hyphae, yeasts forms comprising blastoconidia and pseudohyphae. Although most infections by filamentous fungi are characterized by the presence of hyphal elements in tissue, arthroconidia, a type of fungal asexual spore produced by segmentation of fungal hyphae, constitute the primary transmission mode of dermatophyte infections in humans and animals.31 Several studies suggest that the difference in susceptibility between microconidia (small single-celled spore) and arthroconidia depends on the drug and on the strain, and may be one of the causes of therapeutic failure.32 Candida is able to undergo morphological switching between a yeast and a hyphal form, and the diverse virulence factors that promote Candida albicans pathogenicity are also linked to hypha formation.33 Several unique hyphal proteins such as hyphal wall protein 1 and agglutinin-like sequence 3 have been identified as virulence attributes by promoting epithelial attachment and invasion,34 which can also be targeted by the peptides.
As the most prevalent invasive (or systemic) mycoses are caused by yeasts, especially by Candida spp.,35 we focused our remaining studies on these clinically important strains. The anti-fungal activity of Ctn, Ctn[1–14] and Ctn[15–34] was further investigated against selected pathogenic yeast strains by evaluating cell viability with approximately the same concentration ranges used for MIC determinations. Yeast cell viability was determined by a metabolic assay using ATP from viable yeasts to release light with the use of the enzyme luciferase and its substrate luciferin. In this sensitive assay, the luminescent signal recorded is proportional to the amount of ATP present, which accordingly corresponds to the number of viable cells in culture. Results are presented in Figure 1 as relative viability (in percentage) with non-treated yeasts as controls (≈100% viability).
After 48 h, all yeast strains treated with either one of the peptides or AMB at concentrations below their respective MIC values (subinhibitory concentrations) overall kept their viabilities close to untreated cells, except C. krusei with AMB. Once the observed MICs of the drug (peptide or AMB) were reached for each strain, yeast viabilities dropped sharply to ⩽1%.
AMB is a crucial agent in the management of serious systemic fungal infections. In spite of its proven track record, its well-known side effects and toxicity will sometimes require discontinuation of therapy despite a life-threatening systemic fungal infection.36 Therefore, there is a persistent need to find valuable drug candidates that can match the efficacy of AMB without its deleterious toxic effects. The finding that Ctn, Ctn[1–14] and Ctn[15–34], hitherto untested against yeasts, were effective anti-fungal agents led us to investigate their cytotoxicity toward eukaryotic cells.
Comparative toxicity of Ctn, Ctn[1–14], Ctn[15–34] and AMB
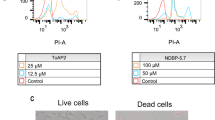
To evaluate possible toxic effects of Ctn, Ctn[1–14] and Ctn[15–34] with healthy eukaryotic cells and compare them with AMB, we carried out two different assays. First, potential nephrotoxicity was assessed in vitro by measuring the human kidney (HK-2) cell viability after treatment for 24 h with either one of the peptides or AMB at increasing concentrations. Percentage relative viability results are presented in Figure 2.
As shown in Figure 2, the known nephrotoxicity of AMB37 was evident in that as low as 12.5 μm of the polyene drug (~1 log above most of the MICs against tested yeasts) killed 50% of HK-2 cells. For their part, Ctn and its fragments (Ctn[1–14] and Ctn[15–34]) displayed kidney cell cytotoxic activities different from each other and from AMB. Ctn, the most toxic peptide, had higher cytotoxicity than AMB (IC50~3.12 μm), in tune with its previously observed low selectivity between pathogens and healthy eukaryotic cells.25 In contrast, Ctn[1–14] and Ctn[15–34] were less toxic to kidney cells compared with either the parental Ctn or AMB, with IC50 values at 400 and 50 μm, respectively.
In a complementary cytotoxicity assay with healthy human kidney cells, shown in Figure 3, the hemolysis profiles of the peptides and AMB were compared using absorbance values from released hemoglobin as readout. As Figure 3 shows, at 1.5 μm, roughly the MIC against most tested strains, AMB already caused substantial (20%) hemolysis. At 12.5 μm, large-scale (70%) hemolysis was observed, in tune with other reports.38, 39 Again, Ctn and its fragments (Ctn[1–14] and Ctn[15–34]) had differing profiles. Thus, Ctn at 1.5 μm was comparable to AMB (20% hemolysis) but no further increase was observed at concentrations up to two orders of magnitude higher. Ctn[1–14] became hemolytic only above 50 μm, whereas Ctn[15–34], even at 100 μm, was inert on red blood cells. Thus, despite its slightly higher MICs (between 5 and 10 μm) against yeast strains (Table 2), Ctn[15–34] has a better selectivity window than AMB. Ctn[15–34] is also more selective against yeasts compared with other cathelicidins such as the human cathelicidin hCAP18/LL-37, whose reported MICs against some Candida albicans strains (15–20 μm)8, 12 were shown to be toxic to healthy eukaryotic cells.19, 22
Ctn, Ctn[1–14] and Ctn[15–34] show synergy with AMB against clinical strains of Candida albicans
As the pharmacotherapy of patients critically ill with invasive mycosis is mainly based on combining two or more anti-fungal drugs,40 we have also investigated the in vitro effects of combining one of the peptides with AMB at the concentration ranges used in the MIC determination. Results of these combined therapies against two clinically isolated Candida albicans strains, the most prevalent yeasts in invasive mycosis,23 were obtained by the checkerboard technique (Table 3).
Table 3 shows and confirms the initially found MICs of the drugs used alone with these strains (Table 2). When associated with AMB, a general decrease in the MICs of both drugs in all combinations was observed, with at least 4- and 64-fold reductions in the MICs of AMB and peptides, respectively. Calculated FIC indexes were around 0.25 and 0.26, well below the ⩽0.50 thresholds for an association to be considered as synergistic. This potentiation of anti-yeast activity by association with AMB was particularly important for the most active peptide Ctn[15–34] and also, to a slightly minor extent, for Ctn[1–14] and Ctn. Therefore, association of either of the peptides with AMB can become a very useful chemotherapeutical approach against invasive yeast infections, inasmuch as the AMB effective dose, hence toxicity and other side effects, may be substantially reduced. This alternative is particularly promising for Ctn[15–34], whose remarkable serum stability (770 min half-life)25 is likely to make association with AMB therapeutically rather promising in vivo.
In conclusion, the anti-fungal activity of Ctn and its fragments (Ctn[1–14] and Ctn[15–34]) completes the already reported anti-bacterial and anticancer profiles of these peptides. Ctn shows once more a limited therapeutic potential because of its low selectivity. Ctn[1–14], for its part, is inactive against bacteria and cancer cells but has an intermediate anti-yeast activity. The relatively modest performances of both Ctn and Ctn[1–14] can be improved towards C. albicans when associated with AMB. Still, the only Ctn-derived peptide emerging as truly promising from our analysis is Ctn[15–34]. Its anti-yeast activity, slightly lower than AMB, is more than compensated by its much lower kidney cell cytotoxicity and practically nil hemolytic activity relative to the polyene antibiotic. In addition, its long half-life in serum and its powerful synergy with AMB make Ctn[15–34] a most valuable candidate for further development as an anti-fungal therapeutic peptide lead, particularly against yeast infections where it could be usefully applied either alone or in combination with a standard antibiotic such as AMB.
References
Gupta, A. K. & Cooper, E. A. Update in antifungal therapy of dermatophytosis. Mycopathologia 166, 353–367 (2008).
Patel, G. A. & Schwartz, R. A. Tinea capitis: still an unsolved problem? Mycoses 54, 183–188 (2011).
Eggimann, P., Garbino, J. & Pittet, D. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect. Dis. 3, 685–702 (2003).
Eggimann, P., Garbino, J. & Pittet, D. Management of Candida species infections in critically ill patients. Lancet Infect. Dis. 3, 772–785 (2003).
Silva, S. et al. Adherence and biofilm formation of non-Candida albicans Candida species. Trends Microbiol 19, 241–247 (2011).
Yapar, N. Epidemiology and risk factors for invasive candidiasis. Ther. Clin. Risk Manag. 10, 95–105 (2014).
van der Warden, N. L., Bleackley, M. R. & Anderson, M. A. Properties and mechanisms of action of naturally occurring antifungal peptides. Cell. Mol. Life Sci. 70, 3545–3570 (2013).
Mehra, T. et al. Alternative approaches to antifungal therapies. Exp. Dermatol. 21, 778–782 (2012).
Reddy, P. A. et al. Synthesis of hemopressin peptides by classical solution phase fragment condensation. Int. J. Pept. 2012, 186034 (2012).
Hancock, R. E. & Sahl, H.G. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat. Biotechnol. 24, 1551–1557 (2006).
Zasloff, M. Antimicrobial peptides of multicellular organisms. Nature 415, 389–395 (2002).
Matejuk, A. et al. Peptide-based antifungal therapies against emerging infections. Drugs Fut. 35, 197 (2010).
Li, Y. et al. Overview on the recent study of antimicrobial peptides: origins, functions, relative mechanisms and application. Peptides 37, 207–215 (2012).
Barlow, P. G. et al. The human cathelicidin LL-37 preferentially promotes apoptosis of infected airway epithelium. Am. J. Respir. Cell. Mol. Biol. 43, 692–702 (2010).
Tomalka, J. et al. Beta-defensin 1 plays a role in acute mucosal defense against Candida albicans. J. Immunol. 194, 1788–1795 (2015).
Yano, J., Noverr, M. C. & Fidel, P. L. Jr. Cytokines in the host response to Candida vaginitis: Identifying a role for non-classical immune mediators, S100 alarmins. Cytokine 58, 118–128 (2012).
Kovach, M. A. et al. Cathelicidin-related antimicrobial peptide is required for effective lung mucosal immunity in Gram-negative bacterial pneumonia. J. Immune 189, 304–311 (2012).
Tomasinsig, L. & Zanetti, M. The cathelicidins—structure, function and evolution. Curr. Protein Pept. Sci. 6, 23–34 (2005).
Bals, R. & Wilson, J. M. Cathelicidins—a family of multifunctional antimicrobial peptides. Cell. Mol. Life Sci. 60, 711–720 (2003).
Lopez-Garcia, B. et al. Anti-fungal activity of cathelicidins and their potential role in Candida albicans skin infection. J. Invest. Dermatol. 125, 108–115 (2005).
Benincasa, M. et al. Fungicidal activity of five cathelicidin peptides against clinically isolated yeasts. J. Antimicrob. Chemother. 58, 950–959 (2006).
Durr, U. H., Sudheendra, U. S. & Ramamoorthy, A. LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochim. Biophys. Acta 1758, 1408–1425 (2006).
Tsai, P. W. et al. Responses of Candida albicans to the human antimicrobial peptide LL-37. J. Microbiol. 52, 581–589 (2014).
Falcao, C. B. et al. Vipericidins: a novel family of cathelicidin-related peptides from the venom gland of South American pit vipers. Amino Acids 46, 2561–2571 (2014).
Falcao, C. B. et al. Structural dissection of crotalicidin, a rattlesnake venom cathelicidin, retrieves a fragment with antimicrobial and antitumor activity. J. Med. Chem. 58, 8553–8563 (2015).
CLSI Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; approved standard third edition. CLSI document M27-A3. (Clinical and Laboratory Standards Institute, Wayne, PA, USA, (2008).
CLSI Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi; approved standard-second edition: CLSI document M38-A2. (Clinical and Laboratory Standards Institute, Wayne, PA, USA, (2008).
Odds, F. C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 52, 1 (2003).
Johnson, M. D. et al. Combination antifungal therapy. Antimicrob. Agents Chemother. 48, 693–715 (2004).
Kohler, L. M. et al. In vitro susceptibility of isolates of Sporothrix schenckii to amphotericin B, itraconazole, and terbinafine: comparison of yeast and mycelial forms. Can. J. Microbiol. 52, 843–847 (2006).
Achterman, R. R. & White, T. C. Dermatophyte virulence factors: identifying and analyzing genes that may contribute to chronic or acute skin infections. Int. J. Microbiol. 2012, 358305 (2012).
Coelho, L. M. et al. In vitro antifungal drug susceptibilities of dermatophytes microconidia and arthroconidia. J. Antimicrob. Chemother. 62, 758–761 (2008).
Naglik, J. R., Richardson, J. P. & Moyes, D. L. Candida albicans pathogenicity and epithelial immunity. PLoS Pathog. 10, e1004257 (2014).
Zhu, W. & Filler, S. G. Interactions of Candida albicans with epithelial cells. Cell Microbiol 12, 273–282 (2010).
Sardi, J. C. et al. Candida species: current epidemiology, pathogenicity, biofilm formation, natural antifungal products and new therapeutic options. J. Med. Microbiol. 62, 10–24 (2013).
Laniado-Laborin, R. & Cabrales-Vargas, M. N. Amphotericin B: side effects and toxicity. Rev. Iberoam. Micol. 26, 223–227 (2009).
Chai, L. Y. et al. An elevated pro-inflammatory cytokine response is linked to development of amphotericin B-induced nephrotoxicity. J. Antimicrob. Chemother. 68, 1655–1659 (2013).
Serrano, D. R. et al. Hemolytic and pharmacokinetic studies of liposomal and particulate amphotericin B formulations. Int. J. Pharm. 447, 38–46 (2013).
Larabi, M. et al. Study of the toxicity of a new lipid complex formulation of amphotericin B. J. Antimicrob. Chemother 53, 81–88 (2004).
Enoch, D. A., Ludlum, H. A. & Brown, N. M. Invasive fungal infections: a review of epidemiology and management options. J. Med. Microbiol 55, 809–818 (2006).
Acknowledgements
Research work at the Institute for Marine Sciences, Federal University of Ceará, was funded by the Program on Toxinology (Issue 2010). We are very thankful to the Coordination for the Improvement of Higher Education Personnel (CAPES), the Ministry of Education (ME) of the Federal Government of Brazil and the Brazilian National Council for Scientific and Technological Development (CNPq) (Proc. 310845/2012-2 and Proc 247970/2013-1), the Ministry of Science, Technology and Innovation (MCTI) for their constant endorsement and financial support to our projects. CBF is an associate researcher from the National Program for Post-Doctorates (CAPES/ME) at the Postgraduate Program in Pharmaceutical Sciences, Faculty of Pharmacy, Dentistry and Nursing, the Federal University of Ceara. CSPC was a recipient fellow from the program ‘Science without Borders’ (CsF/CNPq/MCTI) at the Department of Experimental Health Sciences, Pompeu Fabra University, Barcelona, Spain. Work at Pompeu Fabra University was funded by MINECO (SAF2011-24899 and AGL2014-52395-C2 Grants, to DA).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cavalcante, C., Falcão, C., Fontenelle, R. et al. Anti-fungal activity of Ctn[15–34], the C-terminal peptide fragment of crotalicidin, a rattlesnake venom gland cathelicidin. J Antibiot 70, 231–237 (2017). https://doi.org/10.1038/ja.2016.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2016.135
This article is cited by
-
Nano amphotericin B: a good anti-leishmanial drug with effect on cathelicidin gene expression
Journal of Parasitic Diseases (2021)
-
Murine cathelicidin: as a host defensive response against Leishmania major infection
Journal of Parasitic Diseases (2020)
-
Antiviral Activity of Ctn[15-34], A Cathelicidin-Derived Eicosapeptide, Against Infectious Myonecrosis Virus in Litopenaeus vannamei Primary Hemocyte Cultures
Food and Environmental Virology (2017)