Abstract
The long-term persistence of antibiotic-resistant bacteria depends on their fitness relative to other genotypes in the absence of drugs. Outside the laboratory, viruses that parasitize bacteria (phages) are ubiquitous, but costs of antibiotic resistance are typically studied in phage-free experimental conditions. We used a mathematical model and experiments with Escherichia coli to show that lytic phages strongly affect the incidence of antibiotic resistance in drug-free conditions. Under phage parasitism, the likelihood that antibiotic-resistant genetic backgrounds spread depends on their initial frequency, mutation rate and intrinsic growth rate relative to drug-susceptible genotypes, because these parameters determine relative rates of phage-resistance evolution on different genetic backgrounds. Moreover, the average cost of antibiotic resistance in terms of intrinsic growth in the antibiotic-free experimental environment was small relative to the benefits of an increased mutation rate in the presence of phages. This is consistent with our theoretical work indicating that, under phage selection, typical costs of antibiotic resistance can be outweighed by realistic increases in mutability if drug resistance and hypermutability are genetically linked, as is frequently observed in clinical isolates. This suggests the long-term distribution of antibiotic resistance depends on the relative rates at which different lineages adapt to other types of selection, which in the case of phage parasitism is probably extremely common, as well as costs of resistance inferred by classical in vitro methods.
Similar content being viewed by others
Introduction
Antibiotic resistance is increasingly problematic for treatment of infectious diseases (Levy and Marshall, 2004; Bergstrom and Feldgarden, 2008). Resistance evolves rapidly and can persist long after antibiotic usage stops (Andersson and Hughes, 2011). Persistence in drug-free conditions is predicted to depend on fitness relative to sensitive genotypes (Andersson and Levin, 1999; Andersson and Hughes, 2010), and in many cases resistance is costly (Björkman and Andersson, 2000; Reynolds, 2000; Gagneux et al., 2006; Andersson and Hughes, 2010). However, viruses that parasitize bacteria (phages) are excluded from typical experiments on antibiotic resistance, despite being ubiquitous outside the laboratory (Brüssow and Hendrix, 2002; Breitbart et al., 2003). Phage populations are diverse (Weinbauer, 2004), spatially structured (Sutherland et al., 2004; Webb et al., 2004; Abedon and Culler, 2007), dynamic (Hennes and Simon, 1995; Chibani-Chennoufi et al., 2004) and undergo continual adaptation to their bacterial hosts (Vos et al., 2009; Koskella, 2013; Levin et al., 2013). Therefore, exposure to novel lytic phages will be common in natural and pathogenic populations. Furthermore, there is renewed interest in using phages to treat bacterial infections of humans or animals (Levin and Bull, 2004; Abedon et al., 2011), particularly where drug treatment has failed because of resistance (Chanishvili et al., 2001).
Understanding the impact of phages is particularly relevant for genetically mixed populations containing antibiotic-resistant and -sensitive genotypes. This is often the case in pathogenic populations (Foweraker et al., 2005; Fothergill et al., 2010; Workentine et al., 2013) because of spatial heterogeneity of drug concentrations (Baquero and Negri, 1997), historical exposure to antibiotics followed by immigration or mutation (Seppälä et al., 1997; Scanvic-Hameg et al., 2002) or the inherently high genetic diversity in chronic infections (Oliver et al., 2000, 2004). Natural populations are also genetically diverse in terms of drug resistance (D'Costa et al., 2006; Martinez, 2009). How does phage parasitism influence the frequencies of antibiotic-resistant and -sensitive genotypes in such scenarios? Evolutionary theory predicts that parasitism can modify selection on costly alleles (Howard and Lively, 1994; West et al., 1999), but experimental evidence is mixed (Haag et al., 2003; Cooper et al., 2005; Buckling et al., 2006). Phages may directly alter the relative growth rates of antibiotic-resistant and -sensitive populations because more rapidly replicating lineages are more commonly infected (‘killing the winner’; Thingstad and Lignell, 1997; Weinbauer and Rassoulzadegan, 2004) or because of direct interactions between antibiotic resistance and phage replication (Constantinou et al., 1986; Hammer et al., 1987; Schmitt et al., 1995; Escobar-Páramo et al., 2012). Alternatively, if phage-resistance mutations are common and their selective benefit is large, frequencies of different lineages over time may depend primarily on the relative rates at which they acquire phage resistance. This will be determined by their relative mutation supply rates (product of population size and mutation rate) that may in turn be influenced by antibiotic resistance. Therefore, phages potentially modify selection on resistance elements through ecological and/or evolutionary effects.
To investigate this, we used experiments with Escherichia coli coupled with a mathematical model of a population of bacteria exposed to phages. To model the appearance of phage-resistance mutations, we used stochastic processes (Parzen, 1999) that have been used elsewhere to determine the probability of a population under strong selection being rescued from extinction by mutation (Alexander and Bonhoeffer, 2012; Martin et al., 2013; Tazzyman and Bonhoeffer, 2014). Our model and assumptions are as follows. The initial population is assumed to be phage sensitive, and consequently declines exponentially in size upon exposure to phage. There are two genetic backgrounds in the population: antibiotic resistant and antibiotic sensitive. We model the appearance of phage-resistance mutations on a given genetic background as a Poisson process (Parzen, 1999, section 4.2) with a rate determined by population size and mutation rate. We use a nonhomogenous birth–death process to incorporate the probability that a given phage-resistance mutation will not go extinct because of stochastic fluctuations while it is rare (Parzen, 1999, section 7.5), and this probability is itself influenced by the cost of antibiotic resistance in terms of intrinsic bacterial growth rate. We focussed on the case where one of the two genetic backgrounds fixes via genetic hitchhiking with a phage-resistance mutation (Maynard Smith and Haigh, 1974; Barton, 2000), and analysed the influence of costs of antibiotic resistance, mutation rates and initial genotype frequencies on the conditional probability that the antibiotic-resistant background fixes.
In experiments, we tested the effects of two phages on genotype frequencies and phage resistance in populations containing antibiotic-sensitive E. coli and genotypes with defined resistance mutations against ciprofloxacin, rifampicin or streptomycin. E. coli and associated phages are common in mammalian gastrointestinal tracts and antibiotic resistance is increasingly problematic in pathogenic strains (Kaper et al., 2004; Tenaillon et al., 2010). Our model indicates that costs of antibiotic resistance, genomic mutation rate and initial genotype frequencies can all influence the outcome of phage selection; we tested these factors experimentally using a metapopulation approach (following average changes in genotype frequencies across many sub-populations, or demes, in metapopulations exposed to different phage treatments), a mutator genotype with defective DNA mismatch repair and by changing the starting ratio of competing genotypes respectively. Finally, to test the robustness of our findings over different ecological conditions, we initiated competitions at different phage-to-bacteria ratios, including different antibiotic-resistant mutants, and over an extended timescale.
Materials and methods
Model
We consider two diallelic loci, one coding for antibiotic resistance (denoted a for the antibiotic-sensitive allele, and A for the antibiotic-resistant allele), and the other coding for phage resistance (p for phage sensitive, and P for phage resistant). We therefore have four possible genotypes: ap, Ap, aP and AP. We denote the number of ap individuals at time t by X[t], and the number of Ap individuals at time t by Y[t]. The initial population is of size N0, and contains only phage-sensitive individuals, hence X[0]+Y[0]=N0. An initial proportion ϕ of the population is antibiotic-resistant, and hence X[0]=(1−ϕ)N0 and Y[0]=ϕ N0.
We do not model phage population dynamics explicitly, instead focussing on a scenario where infectious phages are present in sufficient numbers to increase death rates of p individuals, making phage-resistance allele P beneficial. Our experimental data indicate this is true over a range of initial phage population densities (Supplementary Figure S1).
We denote the per-capita birth rate of ap individuals by b, and the per-capita birth rate of Ap individuals by b(1–c). The term c reflects the cost of antibiotic resistance in the absence of antibiotics (0<c << 1, consistent with our experimental data and typical observations from the literature, as discussed below). The per-capita death rate of both ap and Ap individuals is denoted d. At time t=0, phages become present. Because both genotypes are phage susceptible at t=0, b<d and the numbers of both genotypes decline. The populations are initially large, and hence we model their size deterministically,

We model the (initially nonexistent) populations of aP and AP individuals using branching processes, and thus we assume that the sizes of these populations are independent from one another. In particular, the survival or otherwise of small populations of these genotypes are dependent on their own birth and death rates and nothing else.
Individuals with genotype ap mutate at rate μ into phage-resistant aP individuals. When the lineage descending from a new phage-resistant mutant remains small, there is some probability that it will go extinct because of stochastic fluctuations in population size. We account for this by concentrating on the appearance of rescue mutations, rather than simply phage-resistance mutations. Rescue mutations are defined as those phage-resistance mutations that lead to a lineage that does not go extinct. We treat the appearance of rescue mutants of genotype aP as a nonhomogenous Poisson process with intensity ra[t]=μX[t]paP[t] at time t, where paP[t] is the survival probability of a lineage of aP individuals descending from a single individual at time t (that is, the fixation probability for a new phage-resistant mutant on an a background) (Alexander and Bonhoeffer, 2012; Parzen, 1999 section 4.2, Tazzyman and Bonhoeffer, 2014). The probability-generating function for the number of rescue mutations that have arisen at time t on an a background is then

and hence the probability that no rescue mutations appear, and the antibiotic-sensitive a background goes extinct, is  . Then, the probability of rescue for the a allele is
. Then, the probability of rescue for the a allele is  .
.
It remains to estimate paP[t]. We use a birth–death approach (Parzen, 1999; Alexander and Bonhoeffer, 2012 section 7.5, Tazzyman and Bonhoeffer, 2014). If we define the birth rate of aP individuals as B, and their death rate as D, and suppose B>D, then

for all t (see Supplementary Materials for full details). Then

Individuals with genotype Ap mutate at rate ν to become AP. Supposing that AP individuals pay the same cost of antibiotic resistance as aP individuals, and consequently have birth rate B(1–c) and death rate D, we follow the same procedure as above. The probability-generating function for the number of rescue mutations that have arisen at time t on an A background is

the survival probability pAP[t] is

Thus, increasing costs of antibiotic resistance increase the likelihood that a given phage-resistance mutation on an antibiotic resistant background is lost when rare, consistent with classic models showing that linked deleterious mutations can reduce the fixation probability of beneficial mutations (Peck, 1994; Barton, 1995). As  , our estimate PA for the rescue probability of the A background is
, our estimate PA for the rescue probability of the A background is

In the scenario where a single genetic background emerges from phage-mediated selection (that is, that either the a or the A allele is driven to fixation by hitchhiking with a P rescue allele), we denote by Q the conditional probability that the antibiotic-resistant A allele fixes, given that fixation of either A or a occurs, and have

Organisms and growth conditions
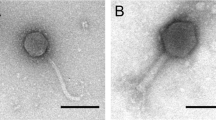
We used E. coli K12 MG1655 at 37 °C for all experiments. Antibiotic-resistant mutants were isolated through a single round of selection by plating independent cultures on agar supplemented with antibiotics as described previously (Hall, 2013). Resistance mutations were identified by sequencing gyrA (encoding DNA gyrase) for ciprofloxacin, rpoB (encoding the β-subunit of RNA polymerase) for rifampicin and rpsL (encoding ribosomal protein S12) for streptomycin. For competitions lasting 24 h, we used the following mutants in addition to the wild type: gyrA D87G (CipR), rpoB S512F (RifR) (Hall, 2013) and rpsL K43N (StrR) (Angst and Hall, 2013). HK578 is a double-stranded DNA Siphovirid phage; T4 is Myovirid. Every bacterial genotype was initially susceptible to lysis by both phages.
Pairwise competitions
We used the same basic protocol for pairwise competitions as previous studies on costs of resistance (Reynolds, 2000; Gagneux et al., 2006; Trindade et al., 2009) and experimental evolution in general (Lenski et al., 1991). Selection coefficients (s) were estimated in competitions with a phenotypically marked wild-type genotype, E. coli K12 MG1655 Δara, that is otherwise isogenic but distinguished by red colonies on tetrazolium arabinose (TA) agar (Trindade et al., 2009). For each competition, we grew independent cultures of both competitors, before mixing them 1:1 v:v and diluting 100-fold into 1 ml liquid Lysogeny Broth (∼107 cells), then incubating with orbital shaking for 24 h. We estimated initial and final genotype frequencies by plating on TA agar, and calculated s=ln(Rfinal/Rinitial), where Rfinal and Rinitial are genotype ratios (Lenski et al., 1991; Travisano and Lenski, 1996; Lopez-Pascua and Buckling, 2008; Gómez and Buckling, 2013; Zhang, 2014), corrected by the cost of the Δara marker (Trindade et al., 2009). This gives the difference in Malthusian growth parameters per day compared with the antibiotic-sensitive wild type grown in phage-free conditions. Unless otherwise stated, competitions were replicated independently six times. We replicated the entire experiment in the presence of each phage, adding ∼107 particles HK578 or T4 at the start of the 24 h competition. Statistical analyses were done in R v2.11.1 (R Development Core Team, 2010); further details are given below and in online Supplementary Information.
Resistance testing
At the end of each competition, we streaked five independent colonies of each competitor against both phages on agar plates, excepting cases where bacteria went extinct or one genotype fixed, in which case we streaked five colonies of the ‘winning’ genotype. This was done by drying a line of 20 μl phage onto an agar plate before streaking bacteria across it with a sterile toothpick and scoring isolates as resistant if there was no evidence of inhibition by phages after 24 h of incubation (Buckling et al., 2006; Brockhurst et al., 2007). For a given population we calculated resistance to the phage they were exposed to as the proportion of colony isolates that were resistant. In some cases a mucoid phenotype was observed (sticky, raised colonies on agar plates: Supplementary Figure S2). We tested for cross-resistance to T5 (Siphoviridae), T6 (Myoviridae) and λ (Siphoviridae) for nine mucoid colonies isolated from independent populations and the wild type.
Cost of antibiotic resistance in metapopulations
Phage-resistance evolution results in stochastic changes in genotype frequencies in individual populations (see below). Therefore, sufficient statistical power to infer any effect of antibiotic resistance on the likelihood that a given genetic background increases or decreases in frequency can only be obtained with a vast number of experimental replicates. To circumvent this problem we used a metapopulation approach (Supplementary Figure S3). For a given metapopulation, 96 independent cultures of each competitor were grown overnight, before being mixed 1:1 v:v, giving 96 independent mixed cultures (demes), and diluted 100-fold into Lysogeny Broth and exposed to phages or phosphate-buffered saline as above. We quantified the average frequency of each bacterial genotype across the entire metapopulation at the start and end of the assay by pooling samples of all demes and plating them on TA agar (Supplementary Figure S3). We ran four metapopulations for each combination of bacterial genotypes in each phage treatment (none, HK578 or T4), amounting to 4608 demes in total. The 16 metapopulations in each phage treatment were initiated with aliquots from the same 16 independent starting metapopulations (where each starting metapopulation constitutes 96 independent demes before dilution and 24 h growth with or without phages). We analysed these data by a linear mixed effects model with bacterial genotype and phage treatment as factors and starting replicate as a random effect.
Varying initial genotype frequencies
In some scenarios the cost of antibiotic resistance will cause antibiotic-resistant genetic backgrounds to decline in frequency. To determine whether the fate of an antibiotic-resistant background depended on its initial frequency upon exposure to phages, we tested whether the outcome of competitions between one antibiotic-resistant genotype (RifR) and antibiotic-sensitive Δara was influenced by their initial frequencies in different phage treatments. We did competitions as above, except that the initial genotype ratio was either 1:4 or 4:1 v:v, and with eight replicate microcosms at each combination of phage and frequency.
Mutator competitions
The mutator we used is isogenic to wild type except for an insertion ΔPmutS::kan::araC::ParaBAD::mutS that represses mutS in the absence of arabinose. This disrupts the methyl-directed mismatch repair pathway, impairing DNA repair (Oliver et al., 2002; Li et al., 2003) and increasing mutation rate ∼50-fold. We assayed the selection coefficient for the mutator by competitions against Δara in the presence of HK578, T4 or no phage as above.
Long-term competitions
We included additional resistant genotypes rpoB D516G (RifR), gyrA S83L (CipR) and rpsL K88R (StrR), and the wild type, giving seven genotypes in total. We competed each genotype against Δara with and without each phage in triplicate, diluting cultures 100-fold into fresh medium every 24 h for eight transfers (∼54 bacterial generations). We measured optical density (OD600) before each transfer to estimate population densities and followed genotype frequencies by plating on TA agar after 1, 2, 4, 6 and 8 transfers. We tested for resistance to phages by streaking assays after 1 and 8 transfers.
Results
Model results
The probability that neither, one or both of the two bacterial types evolve phage resistance and survive phage selection depends on bacterial mutation rate (ν and μ) at a given population size. Specifically, when ν≈μ, a selective sweep is most likely at intermediate mutation rates (Supplementary Figure S4). In this scenario, phages strongly influence the relative frequencies of drug-resistant and drug-sensitive bacteria, and our results below show this was the most common outcome in experiments with E. coli, consistent with other bacteria-phage experiments (Morgan et al., 2012). In such cases the probability Q that the A antibiotic-resistance allele fixes depends on three main factors: the initial frequency of antibiotic resistance ϕ, the ratio ν/μ of the mutation rates of antibiotic-resistant and antibiotic-sensitive types (‘mutational ratio’) and the cost of antibiotic resistance c.
For fixed values of mutational ratio ν/μ and cost of antibiotic resistance c, as initial frequency of antibiotic-resistant genotypes increases, so does the probability that antibiotic resistance fixes (Figure 1). This is because the more antibiotic resistant individuals there are, the more likely that a phage-resistance rescue mutation will occur on an antibiotic-resistant genetic background. The relationship between ϕ and Q is nonlinear (Figure 1). To see why, consider the case where there are n rescue mutation events in total. All else being equal, each mutation has a probability ϕ of being on an antibiotic-resistant background, and (1−ϕ) of being on a wild-type background. The probability that all of them are on an antibiotic-resistant background is then ϕn, whereas the probability that all of them are on a wild-type background is (1−ϕ)n. Thus, the probability that antibiotic resistance fixes, given that n rescue mutations occur, is ϕn /( ϕn+(1 – ϕ)n). If n>1, this probability will be greater than ϕ for values of ϕ>½, and less than ϕ for values of ϕ<½. Because this nonlinearity results from cases where more than one rescue mutation occurs, it will decrease with smaller mutation rates ν and μ (Supplementary Figure S5) at a given population size.
The probability Q that all individuals are genotype AP following strong selection for phage resistance (given that one lineage fixes) as a function of the initial proportion of antibiotic-resistant bacteria ϕ. The heavy black line shows the case with no cost of antibiotic resistance and equal mutation rates for both genotypes. Increasing the mutation rate of the antibiotic-resistant type increases its probability of fixing (left-hand curve), whereas increasing the cost of antibiotic resistance decreases its probability of fixing (right-hand curve). Parameter values: N0=107, μ=10−7.5, B=1, D=0.1, b=1, d=1.2 (all three curves); c=0, ν=2.4 × 10−7.5 (left-hand curve), c=0, ν=10−7.5 (central bold curve) and c=0.25, ν=10−7.5 (right-hand curve).
Given a fixed initial frequency ϕ and cost of antibiotic resistance c, increasing the mutational ratio ν/μ increases the probability that the antibiotic-resistant-type fixes (Figure 1), because it increases the mutation supply rate on this genetic background, making phage-resistance mutations more probable.
Given a fixed initial frequency ϕ and mutational ratio ν/μ, increasing the cost of antibiotic resistance c decreases the probability that the antibiotic-resistant type fixes (Figure 1), because the cost of antibiotic resistance makes the population of antibiotic-resistant types decline more rapidly, and consequently there is less opportunity to produce a phage-resistant mutant. In addition, larger costs of antibiotic resistance increase the probability that phage-resistance mutations on antibiotic-resistant genetic backgrounds are lost because of stochastic processes before they can spread and become rescue mutations.
The negative effects of an increased cost of antibiotic resistance c can be exactly cancelled out by an increased mutational ratio ν/μ, with the resultant Q-value being the same function of ϕ as in the case where c=0 and ν/μ=1. The exact (ν/μ) value that cancels a given c-value depends on birth and death rates b, d, B and D, as well as on c (see Supplementary Materials). For small increases of c, including those observed in our experiments below in the absence of phages, the increase in ν/μ required increases linearly with increasing costs (Figure 2). This suggests that even a small increase in mutational ratio ν/μ will offset the deleterious effects of a cost of antibiotic resistance c. Therefore, if antibiotic-resistant genotypes are hypermutable, the likelihood that antibiotic resistance spreads during a phage-mediated selective sweep is relatively high.
Parameter space with cost of antibiotic resistance c against mutational ratio ν/μ. The effect of different values of c and ν/μ for the probability of fixation of antibiotic resistance under phage selection is shown for initial frequency ϕ=0.5. Combinations of parameters in the white section increase the probability that the antibiotic-resistant type fixes, whereas those in the grey area decrease it. On the black curve the probability of fixation is identical to the case where c=0 and ν/μ=1. In reality, the cost of antibiotic resistance is likely to be small, whereas if resistant types are hypermutable, the mutational ratio may be large.
Phages cause rapid changes in E. coli genotype frequencies
In the absence of phages, selection coefficients varied among different genotypes (analysis of variance: F3, 20=33.88, P<0.0001, Figure 3a), and resistance against each antibiotic was costly (P<0.01 for each genotype compared with wild type by t-tests). In the presence of phage T4 or HK578 (Figures 3b and c), selection coefficients were not affected by antibiotic-resistance mutations on average (Kruskal–Wallis tests: HK578: χ2=0.08, d.f.=3, P=0.99; T4: χ2=2.70, d.f.=3, P=0.44), but the variance among replicate competitions was greater than in the absence of phages (paired t-tests comparing variance of s for all genotypes in the presence and absence of each phage: P<0.02 for both phage treatments). This was frequently associated with fixation of one of the two genetic backgrounds (Table 1) that was approximately equally likely for antibiotic-resistant and -sensitive bacteria (Table 1; χ2 tests for HK578 and T4: P=0.44 and 1).
Selection coefficients in (a) phage-free conditions or the presence of phage (b) HK578 or (c) T4. Circles represent individual competitions and bars show means for genotypes resistant to one of three antibiotics (ciprofloxacin, rifampicin and streptomycin) or the wild type (WT) competed against a marked ancestral strain (Δara). Selection coefficients are shown per day; a per-generation estimate can be obtained in phage-free conditions by dividing by 6.88, the average number of doublings observed in these conditions.
Phage parasitism reduced final population density by ∼98% (T4) and 94% (HK578) on average compared with phage-free populations, imposing strong selection for phage resistance that we detected in 16 out of 18 populations exposed to HK578 and 16 out of 20 exposed to T4, excluding microcosms where bacteria went extinct. In several cases, resistance was linked to a mucoid colony phenotype (Table 1 and Supplementary Figure S1) that is known to be associated with phage resistance (Labrie et al., 2010). Mucoidy evolved on antibiotic-resistant and -sensitive genetic backgrounds and conferred cross-resistance to HK578 and T4 as well as T5, T6 and λ, all of which infect the wild type. Thus, changes in genotype frequencies were predictable from the presence of drug-resistance alleles in the absence of phages or antibiotics, consistent with a cost of resistance in terms of intrinsic growth (Figure 3a). In phage treatments, the presence of drug-resistance alleles offered no predictive power over the final frequencies of different genetic backgrounds at this level of replication. Instead, one or the other genetic background in each population tended to acquire phage resistance during the experiment and rapidly increase in frequency (Figures 3b and c and Table 1).
Phage-infected metapopulations
To increase our statistical power to detect any effect of antibiotic-resistance alleles on the likelihood that a given genetic background spreads under phage selection, we quantified changes in the average frequency of antibiotic-resistant bacteria across metapopulations, each consisting of 96 independent demes. The variance among replicate metapopulations was much smaller than among individual microcosms above (Figures 4b and c compared with Figures 3b and c) and StrR bacteria had a lower average selection coefficient compared with other antibiotic-resistant bacteria and the wild type, although overall variation among different genetic backgrounds was not statistically significant (F3, 12=2.43, P=0.12) and was not significantly altered by phages (genotype × phage interaction: F6, 24=1.87, P=0.13). Thus, any effects of antibiotic resistance alleles were very small (approximately proportional to the cost of antibiotic resistance in the absence of phages) relative to the benefits of phage resistance in individual populations.
Positive frequency-dependent selection
Initial genotype frequency did not influence the cost of antibiotic resistance in the absence of phages (Welch’s t10=0.73, P=0.48, Figure 5a). With HK578, there was strong evidence of positive frequency dependence: drug-resistant bacteria increased in frequency when initially common and declined when initially rare (Welch’s t10=10.67, P<0.0001, Figure 5b). With T4, resistant bacteria declined when rare, but increased in frequency in only two populations when initially common, and there was no average difference in s depending on frequency (Welch’s t5.7=0.40, P=0.70, Figure 5c). Thus, high initial frequency increased the likelihood of fixation in the presence of one of the two phages, consistent with our model. For the other phage, antibiotic-sensitive bacteria fixed in some populations despite low initial frequency.
Competitions initiated at different genotype frequencies. The frequency of a RifR genotype is shown over time for competitions initiated at different frequencies relative to a drug-sensitive genotype with (a) no phages, (b) HK578 or (c) T4. Each line shows a single population (n=8 in each group). In three HK578 and three T4 populations, bacteria were driven extinct by phages, and one or the other genotype appeared to fix in 8 and 10 populations, respectively.
Elevated mutation rate is beneficial under phage selection
Our model predicts that genotypes producing phage-resistance mutations more frequently are more likely to survive under phage selection (Figure 1). We tested this by competitions between wild-type bacteria and a mutator. The selective benefit of an elevated mutation rate was clearly dependent on the presence of phages (Kruskal–Wallis test: χ2=7.89, d.f.=2, P=0.019; Figure 6). Mutators had no selective advantage over the wild type in the absence of phages over this timescale (t5=0.002, P=0.99), but with HK578 or T4, mutators fixed within 24 h in 4 out of 6 and 5 out of 6 microcosms, respectively. Mucoid phenotypes emerged on the mutator background in eight of these microcosms. As above, mucoid colonies were not observed in any phage-free populations.
Effect of phages over longer timescales
Phages had the same qualitative effects as above over the first few generations, causing relatively rapid changes in genotype frequencies (Supplementary Figures S6A–C). Over the entire experiment, the effect of phages on bacterial population size was maintained, despite being strongest early on (Supplementary Figure S6D–F). Moreover, phages caused fixation of one or the other genetic background in a greater number of populations (no phage: 5, HK578: 17, T4: 17; Pearson’s χ2=7.38, d.f.=2, P=0.02; Supplementary Figure S7). Phages did not significantly alter the average frequency of antibiotic-resistant bacteria at the end of the experiment (mixed effects model with genotype as a random effect: F2, 10=1.82, P=0.21; Supplementary Figure S7). Thus, although phages had no net effect on the average frequency of antibiotic-resistant genotypes, in individual populations they had strong demographic effects and usually caused either antibiotic-resistant or -sensitive genetic backgrounds to approach fixation.
Discussion
In the absence of phages and antibiotics, drug-resistance alleles are costly and tend to decline in frequency over time. Upon exposure to a lytic virus, phage-resistance mutations that occur stochastically on different genetic backgrounds are highly beneficial, indirectly favouring other alleles on the same genome because of genetic hitchhiking (Maynard Smith and Haigh, 1974; Barton, 2000), a process that has been demonstrated in microbes in other contexts (Morgan et al., 2012; Waite and Shou, 2012). Our model and experiments suggest that the likelihood of an antibiotic-resistant genetic background spreading under phage selection depends on the cost of antibiotic resistance in terms of intrinsic growth rate (c), the initial frequencies of different genetic backgrounds (ϕ) and the ratio of their genomic mutation rates (ν/μ), because these parameters contribute directly to the relative supply rates of phage-resistance mutations. Our theoretical work suggests that relatively small increases in mutability will more than cancel out the negative effects of a cost of antibiotic resistance on the likelihood that a given genetic background fixes (Figure 2). Consistent with this, the average cost of antibiotic resistance in the absence of phages (s=−0.15 per generation, s.d.=0.10, taking the number of generations in each assay as log2(Nfinal/Ninitial) where N is the final or initial population size; Lenski et al., 1991) was small relative to the benefit of an elevated mutation rate in the presence of phages (s=0.42 per generation s.d.=0.08, conservatively assuming 6.64 doublings following 100-fold dilution) in our experiments. Thus, linkage to mutator alleles in the context of phage-imposed selection is a potential explanation for the persistence of some costly antibiotic-resistance mechanisms in the absence of drugs.
This is potentially relevant outside the laboratory given that mutator bacteria are common in clinical settings, particularly in chronic infections (Oliver et al., 2000; Denamur et al., 2002), and are frequently associated with antibiotic resistance (Giraud et al., 2002; Baquero et al., 2005; Maciá et al., 2005). Crucially, the mutator phenotype of clinical isolates, including E. coli, is frequently because of mutations in mismatch repair genes including mutS (LeClerc et al., 1996; Chopra et al., 2003; Li et al., 2003; Jolivet-Gougeon et al., 2011), the same mechanism as in our experiments. Mutator genotypes typically have mutation rates orders of magnitude higher than nonmutators (LeClerc et al., 1996; Chopra et al., 2003; Maciá et al., 2005), but costs of antibiotic resistance measured in vitro or in vivo are usually <50% (Björkman et al., 2000; Sander et al., 2002; Gagneux et al., 2006). We therefore suggest that hypermutable drug-resistant genetic backgrounds will typically lie in the white region of Figure 2. We note that hitchhiking effects may be disrupted by recombination (Barton, 2000), and that mutator advantage under parasitism also depends on ecological factors such as the structure of the abiotic environment (Gómez and Buckling, 2013). Nevertheless, our finding that an elevated mutation rate is advantageous under phage selection is also consistent with evidence that Pseudomonas fluorescens mutators are favoured during coevolution with phage Φ2 (Pál et al., 2007; O'Brien et al., 2013).
The cost of antibiotic resistance as inferred by classical in vitro methods can also influence the likelihood of fixing under phage selection. This is for two reasons. First, reduced population growth rate lowers the supply rate of phage-resistance mutations. This is equivalent to the effect of genotype frequency (ϕ), and in our metapopulation experiments could result from reduced population growth and in turn a reduced supply of phage-resistance mutations relative to the wild type, both before and during exposure to phages, although any such effects in our experimental system were weak. Second, in our model a phage-resistance mutation on a slower-growing genetic background is more likely to be lost before it can spread and become a rescue mutation. Further experiments would be required to demonstrate conclusively that stochastic loss of beneficial mutations is more likely for slow-growing genotypes. We also note that this effect is expected to be relatively weak when the selective effects of beneficial alleles are relatively large (Johnson and Barton, 2002), as they are here.
Phage resistance was frequently associated with mucoidy. Phage-resistant mucoid mutants have been observed previously in E. coli and other bacteria (Hancock and Reeves, 1975; Mizoguchi et al., 2003; Scanlan and Buckling, 2012). Mucoidy is caused by mutations that increase production of extracellular polysaccharides (Sapelli and Goebel, 1964; Lieberman and Markovitz, 1970). In our experiments, mucoidy conferred cross-resistance to HK578, T4, T5, T6 and λ, and therefore appears to be a general adaptive response to phage parasitism (Labrie et al., 2010).
In other scenarios, such as infection by nonlytic filamentous phages, the selective benefit of phage resistance may be smaller compared with the cost of antibiotic resistance than it was here. In addition, some antibiotic-resistance mechanisms may interfere with phage replication (Constantinou et al., 1986; Hammer et al., 1987; Schmitt et al., 1995; Jalasvuori et al., 2011; Escobar-Páramo et al., 2012), meaning that genotype frequencies and relative likelihoods of evolving phage resistance are influenced by differential susceptibilities to infection. The cost associated with phage resistance may also vary depending on the presence of antibiotic-resistance alleles (Zhang, 2014). This could be incorporated into our modelling framework by including a parameter for the cost of phage resistance on different genetic backgrounds; here we excluded the cost of phage resistance because we are interested in scenarios where infectious phages are present, and therefore the benefits of phage-resistance mutations vastly outweigh their cost in terms of intrinsic growth rate. Despite this, a cost of phage resistance may partially explain the sustained effects of phages on population density in our long-term experiment that is promising for phage therapy. In some scenarios, phages may even prevent antibiotic-resistance evolution from occurring in the first place, such as when phages and antibiotics are applied simultaneously (Zhang and Buckling, 2012). Again, an expanded modelling framework could incorporate this by beginning with only ap genotypes and including mutation to A, with specific death rates in the presence of antibiotics. We suggest, therefore, that in applying phages therapeutically (Brüssow, 2005; Abedon et al., 2011), careful study of interactions between resistance mechanisms will be beneficial.
References
Abedon ST, Culler RR . (2007). Bacteriophage evolution given spatial constraint. J Theor Biol 248: 111–119.
Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM . (2011). Phage treatment of human infections. Bacteriophage 1: 66–85.
Alexander HK, Bonhoeffer S . (2012). Pre-existence and emergence of drug resistance in a generalized model of intra-host viral dynamics. Epidemics 4: 187–202.
Andersson DI, Levin BR . (1999). The biological cost of antibiotic resistance. Curr Opin Microbiol 2: 489–493.
Andersson DI, Hughes D . (2010). Antibiotic resistance and its cost: is it possible to reverse resistance? Nat Rev Microbiol 8: 260–271.
Andersson DI, Hughes D . (2011). Persistence of antibiotic resistance in bacterial populations. FEMS Microbiol Rev 35: 901–911.
Angst D, Hall AR . (2013). The cost of antibiotic resistance depends on evolutionary history in Escherichia coli. BMC Evol Biol 13: 163.
Baquero F, Negri MC . (1997). Selective compartments for resistant microorganisms in antibiotic gradients. Bioessays 19: 731–736.
Baquero MR, Galán JC, Turrientes MD, Cantón R, Coque TM, Martínez JL et al. (2005). Increased mutation frequencies in Escherichia coli isolates harboring extended-spectrum β-lactamases. Antimicrob Agents Chemother 49: 4754–4756.
Barton NH . (1995). Linkage and the limits to natural selection. Genetics 140: 821–841.
Barton NH . (2000). Genetic hitchhiking. Philos Trans R Soc Lond B Biol Sci 355: 1553–1562.
Bergstrom CT, Feldgarden M . (2008). The ecology and evolution of antibiotic-resistant bacteria. In: Stearns SC, Koella JC (eds) Evolution in Health and Disease 2nd edn. Oxford University Press: Oxford, pp 125–137.
Björkman J, Andersson DI . (2000). The cost of antibiotic resistance from a bacterial perspective. Drug Resist Updat 3: 237–245.
Björkman J, Nagaev I, Berg OG, Hughes D, Andersson DI . (2000). Effects of environment on compensatory mutations to ameliorate costs of antibiotic resistance. Science 287: 1479–1482.
Breitbart M, Hewson I, Felts B, Mahaffy JM, Nulton J, Salamon P et al. (2003). Metagenomic analyses of an uncultured viral community from human feces. J Bacteriol 185: 6220–6223.
Brockhurst MA, Morgan AD, Fenton A, Buckling A . (2007). Experimental coevolution with bacteria and phage. The Pseudomonas fluorescens—Φ2 model system. Infect Genet Evol 7: 547–552.
Brüssow H, Hendrix RW . (2002). Phage genomics: small is beautiful. Cell 108: 13–16.
Brüssow H . (2005). Phage therapy: the Escherichia coli experience. Microbiology 151: 2133–2140.
Buckling A, Wei Y, Massey RC, Brockhurst MA, Hochberg ME . (2006). Antagonistic coevolution with parasites increases the cost of host deleterious mutations. Proc R Soc B Biol Sci 273: 45–49.
Chanishvili N, Chanishvili T, Tediashvili M, Barrow PA . (2001). Phages and their application against drug-resistant bacteria. J Chem Technol Biot 76: 689–699.
Chibani-Chennoufi S, Bruttin A, Dillmann ML, Brüssow H . (2004). Phage-host interaction: an ecological perspective. J Bacteriol 186: 3677–3686.
Chopra I, O'Neill AJ, Miller K . (2003). The role of mutators in the emergence of antibiotic-resistant bacteria. Drug Resist Updat 6: 137–145.
Constantinou A, Voelkel-Meiman K, Sternglanz R, McCorquodale MM, McCorquodale DJ . (1986). Involvement of host DNA gyrase in growth of bacteriophage T5. J Virol 57: 875–882.
Cooper TF, Lenski RE, Elena SF . (2005). Parasites and mutational load: an experimental test of a pluralistic theory for the evolution of sex. Proc R Soc B Biol Sci 272: 311–317.
D'Costa VM, McGrann KM, Hughes DW, Wright GD . (2006). Sampling the antibiotic resistome. Science 311: 374–377.
Denamur E, Bonacorsi S, Giraud A, Duriez P, Hilali F, Amorin C et al. (2002). High frequency of mutator strains among human uropathogenic Escherichia coli isolates. J Bacteriol 184: 605–609.
Escobar-Páramo P, Gougat-Barbera C, Hochberg ME . (2012). Evolutionary dynamics of separate and combined exposure of Pseudomonas fluorescens SBW25 to antibiotics and bacteriophage. Evol Appl 5: 583–592.
Fothergill JL, Mowat E, Ledson MJ, Walshaw MJ, Winstanley C . (2010). Fluctuations in phenotypes and genotypes within populations of Pseudomonas aeruginosa in the cystic fibrosis lung during pulmonary exacerbations. J Med Microbiol 59: 472–481.
Foweraker JE, Laughton CR, Brown DF, Bilton D . (2005). Phenotypic variability of Pseudomonas aeruginosa in sputa from patients with acute infective exacerbation of cystic fibrosis and its impact on the validity of antimicrobial susceptibility testing. J Antimicrob Chemother 55: 921–927.
Gagneux S, Long CD, Small PM, Van T, Schoolnik GK, Bohannan BJM . (2006). The competitive cost of antibiotic resistance in Mycobacterium tuberculosis. Science 312: 1944–1946.
Giraud A, Matic I, Radman M, Fons M, Taddei F . (2002). Mutator bacteria as a risk factor in treatment of infectious diseases. Antimicrob Agents Chemother 46: 863–865.
Gómez P, Buckling A . (2013). Coevolution with phages does not influence the evolution of bacterial mutation rates in soil. ISME J 7: 2242–2244.
Haag CR, Sakwinska O, Ebert D . (2003). Test of synergistic interaction between infection and inbreeding in Daphnia magna. Evolution 57: 777–783.
Hall AR . (2013). Genotype-by-environment interactions due to adaptation and antibiotic resistance in Escherichia coli. J Evol Biol 26: 1655–1664.
Hammer K, Jensen KF, Poulsen P, Oppenheim AB, Gottesman M . (1987). Isolation of Escherichia coli rpoB mutants resistant to killing by lambda cII protein and altered in pyrE gene attenuation. J Bacteriol 169: 5289–5297.
Hancock RE, Reeves P . (1975). Bacteriophage resistance in Escherichia coli K-12: general pattern of resistance. J Bacteriol 121: 983–993.
Hennes KP, Simon M . (1995). Significance of bacteriophages for controlling bacterioplankton growth in a mesotrophic lake. Appl Environ Microbiol 61: 333–340.
Howard RS, Lively CM . (1994). Parasitism, mutation accumulation and the maintenance of sex. Nature 367: 554–557.
Jalasvuori M, Friman VP, Nieminen A, Bamford JKH, Buckling A . (2011). Bacteriophage selection against a plasmid-encoded sex apparatus leads to the loss of antibiotic-resistance plasmids. Biol Lett 7: 902–905.
Johnson T, Barton NH . (2002). The effect of deleterious alleles on adaptation in asexual populations. Genetics 162: 395–411.
Jolivet-Gougeon A, Kovacs B, Le Gall-David S, Le Bars H, Bousarghin L, Bonnaure-Mallet M et al. (2011). Bacterial hypermutation: clinical implications. J Med Microbiol 60: 563–573.
Kaper JB, Nataro JP, Mobley HL . (2004). Pathogenic Escherichia coli. Nat Rev Microbiol 2: 123–140.
Koskella B . (2013). Phage-mediated selection on microbiota of a long-lived host. Curr Biol 23: 1256–1260.
Labrie SJ, Samson JE, Moineau S . (2010). Bacteriophage resistance mechanisms. Nat Rev Microbiol 8: 317–327.
LeClerc JE, Li BG, Payne WL, Cebula TA . (1996). High mutation frequencies among Escherichia coli and Salmonella pathogens. Science 274: 1208–1211.
Lenski RE, Rose MR, Simpson SC, Tadler SC . (1991). Long-term experimental evolution in Escherichia coli 1. Adaptation and divergence during 2,000 generations. Am Nat 138: 1315–1341.
Levin BR, Bull JJ . (2004). Population and evolutionary dynamics of phage therapy. Nat Rev Microbiol 2: 166–173.
Levin BR, Moineau S, Bushman M, Barrangou R . (2013). The population and evolutionary dynamics of phage and bacteria with CRISPR-mediated immunity. PLoS Genet 9: e1003312.
Levy SB, Marshall B . (2004). Antibacterial resistance worldwide: causes, challenges and responses. Nat Med 10: S122–S129.
Li B, Tsui HC, LeClerc JE, Dey M, Winkler ME, Cebula TA . (2003). Molecular analysis of mutS expression and mutation in natural isolates of pathogenic Escherichia coli. Microbiology 149: 1323–1331.
Lieberman MM, Markovitz A . (1970). Depression of guanosine diphosphate-mannose pyrophosphorylase by mutations in two different regulator genes involved in capsular polysaccharide synthesis in Escherichia coli K-12. J Bacteriol 101: 965–972.
Lopez-Pascua LDC, Buckling A . (2008). Increasing productivity accelerates host-parasite coevolution. J Evol Biol 21: 853–860.
Maciá MD, Blanquer D, Togores B, Sauleda J, Pérez JL, Oliver A . (2005). Hypermutation is a key factor in development of multiple-antimicrobial resistance in Pseudomonas aeruginosa strains causing chronic lung infections. Antimicrob Agents Chemother 49: 3382–3386.
Martin G, Aguilee R, Ramsayer J, Kaltz O, Ronce O . (2013). The probability of evolutionary rescue: towards a quantitative comparison between theory and evolution experiments. Phil Trans R Soc B 368: 20120088.
Martinez JL . (2009). The role of natural environments in the evolution of resistance traits in pathogenic bacteria. Proc R Soc B Biol Sci 276: 2521–2530.
Maynard Smith J, Haigh J . (1974). The hitch-hiking effect of a favourable gene. Genet Res 23: 23–35.
Mizoguchi K, Morita M, Fischer CR, Yoichi M, Tanji Y, Unno H . (2003). Coevolution of bacteriophage PP01 and Escherichia coli O157:H7 in continuous culture. Appl Environ Microbiol 69: 170–176.
Morgan AD, Quigley BJ, Brown SP, Buckling A . (2012). Selection on non-social traits limits the invasion of social cheats. Ecol Lett 15: 841–846.
O'Brien S, Rodrigues AM, Buckling A . (2013). The evolution of bacterial mutation rates under simultaneous selection by interspecific and social parasitism. Proc Biol Sci 280: 20131913.
Oliver A, Canton R, Campo P, Baquero F, Blázquez J . (2000). High frequency of hypermutable Pseudomonas aeruginosa in cystic fibrosis lung infection. Science 288: 1251–1253.
Oliver A, Baquero F, Blázquez J . (2002). The mismatch repair system (mutS, mutL and uvrD genes) in Pseudomonas aeruginosa: molecular characterization of naturally occurring mutants. Mol Microbiol 43: 1641–1650.
Oliver A, Levin BR, Juan C, Baquero F, Blazquez J . (2004). Hypermutation and the preexistence of antibiotic-resistant Pseudomonas aeruginosa mutants: implications for susceptibility testing and treatment of chronic infections. Antimicrob Agents Chemother 48: 4226–4233.
Pál C, Maciá MD, Oliver A, Schachar I, Buckling A . (2007). Coevolution with viruses drives the evolution of bacterial mutation rates. Nature 450: 1079–1081.
Parzen E . (1999) Stochastic Processes. Society for Industrial and Applied Mathematics: Philadelphia, PA.
Peck JR . (1994). A ruby in the rubbish: beneficial mutations, deleterious mutations and the evolution of sex. Genetics 137: 597–606.
R Development Core Team. (2010) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria.
Reynolds MG . (2000). Compensatory evolution in rifampin-resistant Escherichia coli. Genetics 156: 1471–1481.
Sander P, Springer B, Prammananan T, Sturmfels A, Kappler M, Pletschette M et al. (2002). Fitness cost of chromosomal drug resistance-conferring mutations. Antimicrob Agents Chemother 46: 1204–1211.
Sapelli RV, Goebel WF . (1964). The capsular polysaccharide of a mucoid variant of E. Coli K 12. Proc Natl Acad Sci USA 52: 265–271.
Scanlan PD, Buckling A . (2012). Co-evolution with lytic phage selects for the mucoid phenotype of Pseudomonas fluorescens SBW25. ISME J 6: 1148–1158.
Scanvic-Hameg A, Chachaty E, Rey J, Pousson C, Ozoux ML, Brunel E et al. (2002). Impact of quinupristin/dalfopristin (RP59500) on the faecal microflora in healthy volunteers. J Antimicrob Chemother 49: 135–139.
Schmitt CK, Kemp P, Molineux IJ . (1995). Streptomycin- and rifampin-resistant mutants of Escherichia coli perturb F-exclusion of bacteriophage-T7 by affecting synthesis of the F-plasmid protein PifA. J Bacteriol 177: 1589–1594.
Seppälä H, Klaukka T, Vuopio-Varkila J, Muotiala A, Helenius H, Lager K et al. (1997). The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med 337: 441–446.
Sutherland IW, Hughes KA, Skillman LC, Tait K . (2004). The interaction of phage and biofilms. FEMS Microbiol Lett 232: 1–6.
Tazzyman SJ, Bonhoeffer S . (2014). Plasmids and evolutionary rescue by drug resistance. Evolution 68: 2066–2078.
Tenaillon O, Skurnik D, Picard B, Denamur E . (2010). The population genetics of commensal Escherichia coli. Nat Rev Microbiol 8: 207–217.
Thingstad TF, Lignell R . (1997). Theoretical models for the control of bacterial growth rate, abundance, diversity and carbon demand. Aquat Microb Ecol 13: 19–27.
Travisano M, Lenski RE . (1996). Long-term experimental evolution in Escherichia coli. IV. Targets of selection and the specificity of adaptation. Genetics 143: 15–26.
Trindade S, Sousa A, Xavier KB, Dionisio F, Ferreira MG, Gordo I . (2009). Positive epistasis drives the acquisition of multidrug resistance. PLoS Genet 5: e1000578.
Vos M, Birkett PJ, Birch E, Griffiths RI, Buckling A . (2009). Local adaptation of bacteriophages to their bacterial hosts in soil. Science 325: 833–833.
Waite AJ, Shou W . (2012). Adaptation to a new environment allows cooperators to purge cheaters stochastically. Proc Natl Acad Sci USA 109: 19079–19086.
Webb JS, Lau M, Kjelleberg S . (2004). Bacteriophage and phenotypic variation in Pseudomonas aeruginosa biofilm development. J Bacteriol 186: 8066–8073.
Weinbauer MG . (2004). Ecology of prokaryotic viruses. Fems Microbiol Rev 28: 127–181.
Weinbauer MG, Rassoulzadegan F . (2004). Are viruses driving microbial diversification and diversity? Environ Microbiol 6: 1–11.
West SA, Lively CM, Read AF . (1999). A pluralist approach to sex and recombination. J Evol Biol 12: 1003–1012.
Workentine ML, Sibley CD, Glezerson B, Purighalla S, Norgaard-Gron JC, Parkins MD et al. (2013). Phenotypic heterogeneity of Pseudomonas aeruginosa populations in a cystic fibrosis patient. PLoS One 8: e60225.
Zhang QG, Buckling A . (2012). Phages limit the evolution of bacterial antibiotic resistance in experimental microcosms. Evol Appl 5: 575–582.
Zhang QG . (2014). Exposure to phages has little impact on the evolution of bacterial antibiotic resistance on drug concentration gradients. Evol Appl 7: 394–402.
Acknowledgements
Martin Ackermann, Helen Alexander, Sebastian Bonhoeffer, Angus Buckling, Louis Du Plessis, Pedro Gómez-López and Rolf Kümmerli provided helpful comments and discussion. We thank Arnaud Gutierrez and Ivan Matic for the Δara marker, Dominik Refardt for phages and Tobias Bergmiller for the mutator. Sequencing was done at the Genetic Diversity Centre, ETH Zürich. ARH was funded by a Marie Curie Intra-European Fellowship and the Swiss National Science Foundation and SJT by the European Research Council under the 7th Framework Programme of the European Commission (PBDR: Grant Agreement Number 268540).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on The ISME Journal website
Supplementary information
Rights and permissions
About this article
Cite this article
Tazzyman, S., Hall, A. Lytic phages obscure the cost of antibiotic resistance in Escherichia coli. ISME J 9, 809–820 (2015). https://doi.org/10.1038/ismej.2014.176
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ismej.2014.176
This article is cited by
-
Mutant fixation in the presence of a natural enemy
Nature Communications (2023)
-
Phage–Antibiotic Synergy Inhibited by Temperate and Chronic Virus Competition
Bulletin of Mathematical Biology (2022)