Abstract
Recently, gingival margin-derived stem/progenitor cells isolated via STRO-1/magnetic activated cell sorting (MACS) showed remarkable periodontal regenerative potential in vivo. As a second-stage investigation, the present study's aim was to perform in vitro characterisation and comparison of the stem/progenitor cell characteristics of sorted STRO-1-positive (MACS+) and STRO-1-negative (MACS−) cell populations from the human free gingival margin. Cells were isolated from the free gingiva using a minimally invasive technique and were magnetically sorted using anti-STRO-1 antibodies. Subsequently, the MACS+ and MACS− cell fractions were characterized by flow cytometry for expression of CD14, CD34, CD45, CD73, CD90, CD105, CD146/MUC18 and STRO-1. Colony-forming unit (CFU) and multilineage differentiation potential were assayed for both cell fractions. Mineralisation marker expression was examined using real-time polymerase chain reaction (PCR). MACS+ and MACS− cell fractions showed plastic adherence. MACS+ cells, in contrast to MACS− cells, showed all of the predefined mesenchymal stem/progenitor cell characteristics and a significantly higher number of CFUs (P<0.01). More than 95% of MACS+ cells expressed CD105, CD90 and CD73; lacked the haematopoietic markers CD45, CD34 and CD14, and expressed STRO-1 and CD146/MUC18. MACS− cells showed a different surface marker expression profile, with almost no expression of CD14 or STRO-1, and more than 95% of these cells expressed CD73, CD90 and CD146/MUC18, as well as the haematopoietic markers CD34 and CD45 and CD105. MACS+ cells could be differentiated along osteoblastic, adipocytic and chondroblastic lineages. In contrast, MACS− cells demonstrated slight osteogenic potential. Unstimulated MACS+ cells showed significantly higher expression of collagen I (P<0.05) and collagen III (P<0.01), whereas MACS− cells demonstrated higher expression of osteonectin (P<0.05; Mann–Whitney). The present study is the first to compare gingival MACS+ and MACS− cell populations demonstrating that MACS+ cells, in contrast to MACS− cells, harbour stem/progenitor cell characteristics. This study also validates the effectiveness of the STRO-1/MACS+ technique for the isolation of gingival stem/progenitor cells. Human free gingival margin-derived STRO-1/MACS+ cells are a unique renewable source of multipotent stem/progenitor cells.
Similar content being viewed by others
Introduction
The gingiva is the component of the periodontium covering the tooth-bearing alveolar bone and the necks of the teeth. One of its eminent characteristics is its remarkable wound healing and regenerative capacity, with rapid reconstitution of the tissue architecture showing little, if any, evidence of scarring.1 The multiple functions of gingival fibroblasts, their variable responsiveness to growth factors and their ability to produce specific extracellular matrix proteins during the healing process demonstrate that they represent a heterogeneous population of cells.2,3,4,5,6 These properties also indicate the presence of a population of stem/progenitor cells, similar to other periodontal components, which gives rise to these heterogeneous cells.
Representing a key component of the periodontium, the free gingival margin has a unique developmental origin, arising from the outer layer of the dental follicle, the perifollicular mesenchyme,7 as well as partly from the inner layer of the dental follicle, the dental follicle proper,8 from which stem/progenitor cells have been isolated.9 In addition, the free gingival margin partially arises from the periodontal ligament cells,2 which themselves originate from the dental follicle proper;7 periodontal ligament stem/progenitor cells have also been obtained from this tissue10 (Figure 1a). In a recent study, porcine free gingival margin-derived stem/progenitor cells, that were isolated via a minimally invasive procedure and magnetically sorted using anti-STRO-1 antibodies, demonstrated remarkable periodontal regenerative capacity in vivo.11 This finding clearly challenged the classical compartmentalisation theory declaring that the gingival connective tissue does not contribute to periodontal regeneration and that it should be excluded during guided tissue regeneration (GTR) techniques,12 instead showing that this tissue harbours multipotent stem/progenitor cells with remarkable regenerative potential. As a second-stage study, the aim of the present study was to perform in vitro characterisation and comparison of the stem/progenitor cell characteristics of magnetically sorted STRO-1-positive (magnetic activated cell sorting (MACS)+) and -negative (MACS−) cell fractions isolated from the human free gingival margin.
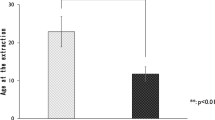
Schema of free gingival margin development, CFU assay, and flow cytometric analysis of the surface marker expression profile of the gingival marginderived cells. (a) Schema of free gingival margin development. (b) Schema of free gingival margin cell isolation. Microscopic appearance and colony formation: (c) phase contrast microscopic appearance of the adherent tissue mass with outgrowing cells (first week) and (d) after the first cell passage. (e) Viability staining using fluorescein diacetate–propidium iodide. The green colour indicates living cells, and the dead cells are labelled in red. (f) CFUs of MACS+ cells (arrows, crystal violet). (g) Phase contrast microscopic appearance of the MACS+ cells (crystal violet). (h) Scattered appearance of the MACS− cells (crystal violet) and (i) phase contrast microscopic appearance of the MACS− cells (crystal violet). (j) CFU assay of MACS+ and MACS− cells (box-and-whisker plots with medians and quartiles). Significant differences are marked with asterisks (n=6, **P<0.01; Mann–Whitney). (k) Flow cytometric analysis of the surface marker expression profile of the MACS+ cells. (l) Flow cytometric analysis of the surface marker expression profile of the MACS− cells. CEJ, cemento-enamel junction; CFU, colony-forming unit; MACS, magnetic activated cell sorting.
Material and methods
Isolation and culture of the tissues
After obtaining informed consent from patients (IRB Approval number D 444/10), healthy, partially impacted third molar teeth with free gingival soft tissue collars were surgically removed from six individuals (n=6) at the Department of Oral Surgery of the Christian Albrechts University, Kiel, Germany. The free gingival tissue collars were detached (Figure 1b, dotted incision line), de-epithelized under magnification, cut into small pieces (approximately 2 mm×2 mm), rinsed several times with Eagle's minimum essential medium alpha modification (Sigma-Aldrich GmbH, Hamburg, Germany) supplemented with antibiotics (100 U⋅mL−1 penicillin, 100 µg⋅mL−1 streptomycin) and 1% amphotericin (all from Biochrom, Berlin, Germany) and placed into dry 75 mL culture flasks (Sarstedt, Nümbrecht, Germany) for 30 min to allow them to adhere to the bottoms of the flasks. Subsequently, the basic medium, consisting of Eagle's minimum essential medium alpha modification supplemented with 15% foetal calf serum (HyClone, Logan, UT, USA), 400 mmol⋅mL−1 L-glutamine (Biochrom, Berlin, Germany), 100 U⋅mL−1 penicillin, 100 µg⋅mL−1 streptomycin and 1% amphotericin, was carefully added. The flasks were incubated in 5% carbon dioxide at 37 °C, and the cells were allowed to grow. The culture flasks were periodically checked using phase contrast inverted microscopy, and the basic medium was changed three times per week.
After reaching 80%–85% confluence, the cells were washed with 5 mL phosphate-buffered saline (PBS) (Biochrom, Berlin, Germany). Two millilitres of 0.10% trypsin-ethylenediaminetetraacetic acid (EDTA) (Biochrom, Berlin, Germany) was added, and the culture flasks were incubated for 1 min to detach the cells. Subsequently, 5 mL of the basic medium was added. The medium containing the cells was transferred to sterile Falcon 50 mL polypropylene conical tubes (Becton Dickinson, Heidelberg, Germany) and centrifuged at 2 000g for 10 min. The supernatant was discarded, and the cells were re-suspended in 2 ml of the basic medium. The cells were counted and tested for viability using Trypan Blue (Sigma-Aldrich GmbH, Hamburg, Germany) and were finally seeded in basic medium at a density of 30 cells⋅cm−2 in 75 mL culture flasks; the flasks were incubated in 5% carbon dioxide at 37 °C.
Fluorescein diacetate–propidium iodide staining
To determine the viability of the seeded cells, fluorescein diacetate–propidium iodide) staining was used. Briefly, stock solutions of fluorescein diacetate (5 mg⋅mL−1 in acetone) and propidium iodide (0.02 mg⋅mL−1 in Dulbecco's PBS) were stored at 4 °C in the dark. Staining was performed by adding a solution containing 2 mg of fluorescein diacetate and 0.6 mg of propidium iodide to the cells and allowing them to stand for 3 min. The cell viability of was investigated using a fluorescence microscope with 520 nm and 590 nm filters.
Immunomagnetic cell sorting
After the first-passage cells reached 80%–85% confluence, they were subjected to immunomagnetic cell sorting using STRO-1 (BioLegend, San Diego, CA, USA) and anti-IgM MicroBeads (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturers' instructions (MACS; Miltenyi Biotec, Bergisch Gladbach, Germany). The positive (MACS+ cells) and the negative (MACS− cells) sorted cell fractions were seeded in basic medium in new 75 mL flasks at a density of 30 cells⋅cm−2.
Flow cytometric analysis
After reaching confluence, samples from second-passage MACS+ cells and second-passage MACS− cells were characterized by flow cytometry using antibodies specific for CD14, CD34, CD45, CD73, CD90 and CD105 (all from Becton Dickinson, Heidelberg, Germany), CD146/MUC18 (eBioscience, NatuTec, Frankfurt, Germany) and STRO-1 (BioLegend, San Diego, CA, USA). The binding of the primary antibodies and the corresponding isotype controls was performed according to standard protocols using FcR Blocking Reagent (Miltenyi Biotec, Bergisch Gladbach, Germany) and was evaluated with FACSCalibur E6370 and FACSComp 5.1.1 software (Becton Dickinson, Heidelberg, Germany).
Colony-forming unit assay
To assess their colony-forming efficiency, MACS+ cells were cultured in basic medium at a density of 1.63 cells⋅cm−1. Aggregates of 50 or more cells were scored as colonies. As controls, MACS− cells were cultured under the same conditions. On the twelfth day, the cultures were fixed with 4% formalin and stained with 0.1% crystal violet, and the numbers of colonies were statistically evaluated.
Multilineage differentiation potential
Osteogenic differentiation
To test for osteogenic differentiation potential, third-passage MACS+ cells and third-passage MACS− cells were cultured on six-well culture plates in osteogenic inductive medium (PromoCell, Heidelberg, Germany) at a density of 2×104 cells per well. As controls, MACS+ cells and MACS− cells were cultured in basic medium. The media were renewed three times per week. At day 14, the cell cultures were stained with Alizarin Red (Sigma-Aldrich GmbH, Hamburg, Germany)13 to label calcified deposits, while the expression of runt-related-transcription-factor-2 (Cbfa1/Runx2) and alkaline phosphatase (ALP) was assessed using real-time polymerase chain reaction (PCR; LightCycler; Roche Molecular Biochemicals, Indianapolis, IN, USA).
Adipogenic differentiation
To test the adipogenic differentiation potential, third-passage MACS+ cells and third-passage MACS− cells were cultured on six-well culture plates in adipogenic inductive medium (PromoCell, Heidelberg, Germany) at a density of 3×105 cells per well. As controls, MACS+ cells and MACS− cells were cultured in basic medium. The media were renewed three times per week. The presence of lipid drops was evaluated by staining the cells with Oil Red O (Sigma-Aldrich GmbH, Hamburg, Germany),13 and the expression of peroxisome proliferator-activated receptor gamma (PPAR-γ; an early adipogenic marker) and lipoproteinlipase (LPL; a late adipogenic marker) was assessed by PCR at day 21.14
Chondrogenic differentiation
To test the chondrogenic differentiation potential, third-passage MACS+ cells and third-passage MACS− cells were incubated with chondrogenic inductive medium (PromoCell, Heidelberg, Germany) in 1.5 mL Eppendorf tubes (Eppendorf, Hamburg, Germany) at a density of 3×104 cells per tube. As controls, MACS+ cells and MACS− cells were cultured in basic medium. The media were renewed three times per week. Chondrogenic differentiation was evaluated at day 35 by staining glycosaminoglycans with Alcian Blue (Sigma-Aldrich GmbH, Hamburg, Germany)13 and by testing for the expression of aggrecan (ACAN), also known as cartilage-specific proteoglycan core protein.
RNA extraction and cDNA synthesis
RNA extraction was performed on MACS+ cells and MACS− cells using an RNeasy kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. The obtained RNA was purified using RNase-free-DNase (Promega, Mannheim, Germany) and quantified photometrically. Complementary cDNA was synthesized from 1–13 µL of RNA (1 µg⋅μL−1) by reverse transcription using a SuperScript reverse transcription kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions (Mastercycler gradient; Eppendorf, Hamburg, Germany). Real-time PCR (LightCycler; Roche Molecular Biochemicals, Indianapolis, IN, USA) was performed as previously described15 using the primers in Table 1.
Statistical analysis
The Shapiro–Wilk test was used to evaluate the normality of the data distribution. Differences in colony-forming unit (CFU) counts and in the mRNA expression of all tested genes between the MACS+ and MACS− cells were examined using the nonparametric Mann–Whitney test with SPSS software (SPSS version 11.5; SPSS, Chicago, IL, USA). The level of significance was set at P=0.05.
Results
Phase contrast inverted microscopy and fluorescein diacetate–propidium iodide staining
Following the initial adherence phase, cells grew out of the gingival tissue masses (Figure 1c). Cells formed adherent fibroblast-like clusters (Figure 1d) and were viable when tested with fluorescein diacetate–propidium iodide staining (Figure 1e).
Colony formation
Twelve days after seeding, CFUs were observed in the MACS+ cell cultures (Figure 1f and 1g). In contrast, MACS− cells seeded under the same culture conditions showed a more diffuse distribution (Figure 1h and 1i). The number of CFUs was significantly higher in the MACS+ cell cultures, with a median of 5 CFUs per 20 MACS+ cells seeded, than in the MACS− cell cultures (P<0.01; Mann–Whitney, Figure 1j).
Flow cytometric analysis
MACS+ cells were negative for CD14, CD34 and CD45 and positive for CD73, CD90, CD105, CD146/MUC18 and STRO-1. The expression of CD73, CD90 and CD105 was above 95% (Figure 1k). MACS− cells showed almost no expression of CD14 and STRO-1, >95% expression of CD73, CD90 and CD146/MUC18 in addition to the positive expression of the haematopoietic markers CD34, CD45 and CD105 (Figure 1l).
Multilineage differentiation potential
Osteogenic differentiation of MACS+ cells was demonstrated by the formation of calcified deposits labelled with Alizarin Red and by the significantly higher expression of Cbfa1/Runx2 (P<0.05; Mann–Whitney) and ALP (P<0.01; Mann–Whitney) than in the controls (Figure 2a–d). Adipogenic differentiation of MACS+ cells resulted in the formation of lipid droplets that were positively stained with Oil Red O and in the significantly higher expression of PPAR-γ (P<0.01; Mann–Whitney) and LPL (P<0.01; Mann–Whitney) than in the controls (Figure 2e–h). Chondrogenic differentiation of MACS+ cells resulted in the formation of glycosaminoglycans positively stained with Alcian Blue and in the higher expression of ACAN (P<0.05; Mann–Whitney), than in the controls (Figure 2i–k). MACS− cells showed no Alizarin Red-positive deposits and a low level of expression of ALP (P<0.05; Mann–Whitney, Figure 2l–o). Adipogenic differentiation was not evident in MACS− cells (Figure 2p–s). Chondrogenic differentiation of MACS− cells was not demonstrated, as was evident by the lack of expression of the cartilage-specific proteoglycan core protein ACAN. MACS− cells and their controls (in sharp contrast to MACS+ cell controls) showed uniform staining of glycosaminoglycans (Figure 2t–v). Chondrogenic lacuna-like structures visible in the stimulated MACS+ cells (Figure 2i) were absent from the stimulated MACS− cells (Figure 2t).
Multilineage differentiation potential of MACS+ cells and MACS− cells. Alizarin Red staining of the osteogenically stimulated MACS+ cells (a) and their controls (b). Cbfa1/Runx2 (c) and ALP (d) expression in stimulated and unstimulated MACS+ cells (box-and-whisker plots with medians and quartiles). Oil Red O staining of the adipogenically stimulated MACS+ cells (e) and their controls (f). PPAR-γ (g) and LPL (h) expression in stimulated and unstimulated MACS+ cells (box-and-whisker plots with medians and quartiles). Alcian Blue staining of the chondrogenically stimulated MACS+ cells (i) and their controls (j). ACAN (k) expression in stimulated and unstimulated MACS+ cells. Alizarin Red staining of the osteogenically stimulated MACS− cells (l) and their controls (m). Cbfa1/Runx2 (n) and ALP (o) expression in stimulated and unstimulated MACS− cells (box-and-whisker plots with medians and quartiles). Oil Red O staining of the adipogenically stimulated MACS− cells (p) and their controls (q). PPAR-γ (r) and LPL (s) expression in stimulated and unstimulated MACS− cells (box-and-whisker plots with medians and quartiles). Alcian Blue staining of the chondrogenically stimulated MACS− cells (t) and their controls (u). ACAN (v) expression in stimulated and unstimulated MACS− cells (box-and-whisker plots with medians and quartiles). Significant differences are marked with asterisks (n=6, *P<0.05, **P<0.01; Mann–Whitney). ACAN, aggrecan; ALP, alkaline phosphatase; Cbfa1/Runx2, runt-related-transcription-factor-2; GAPDH, glyceraldehyde 3-phosphate dehydrogenase; LPL, lipoproteinlipase; MACS, magnetic activated cell sorting; PPAR-γ, peroxisome proliferator-activated receptor gamma.
Gene expression profile
In general, early osteogenic markers such as collagens I and III were more highly expressed than were osteopontin and osteonectin in both cell populations. MACS+ cells tended to show higher expression of early osteogenic markers such as ALP, with significantly different levels reached for collagens I (P<0.05) and III16 (P<0.01). MACS− cells showed a tendency towards higher expression of late osteogenic markers such as osteonectin (P<0.05) and osteopontin, and the expression of collagens I and III and of ALP was lower than in MACS+ cells (Figure 3).
Expression profile of osteogenic markers. mRNA expression profiles for collagen I, collagen III, alkaline phosphatase, osteonectin and osteopontin (box-and-whisker plots with medians and quartiles) in MACS+ and MACS− cells. Significant differences are marked with asterisks (n=6, *P<0.05, **P<0.01; Mann–Whitney). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; MACS, magnetic activated cell sorting.
Discussion
The free gingival margin constitutes a distinctive, as well as a pivotal, component of the human periodontium in both developmental and anatomical terms. This tissue is widely available for use and is routinely removed during dental crown lengthening and periodontal surgical procedures. In a recent study, porcine free gingival margin-derived STRO-1/MACS+ stem/progenitor cells isolated via a minimally invasive procedure were tested and demonstrated remarkable periodontal regenerative capacity in vivo.11 The aim of the present study was to perform in vitro characterisation and comparison of the stem/progenitor cell characteristics of the MACS+ and MACS− cell populations of the human free gingival margin.
Recent investigations of gingival stem/progenitor cells demonstrated their many promising qualities for tissue engineering, including an immunomodulatory property,17 as well as compatibility with alginate hydrogel microbead scaffolds.18 Earlier studies reported the isolation of progenitor cells from oral soft tissues,19 including the rugae and incisive papillae of the palate,20 the maxillary tuberosity,21 the oral mucosa,22 the whole,23 the attached gingiva24,25,26 and hyperplastic gingiva.27 Along with the difference in anatomical location, the free gingival margin partly differs in its developmental origin from the previously described soft tissue sources. In addition to a common neural crest ectomesenchymal origin lined by ectoderm for all oral soft tissues, the inner layer of the dental follicle, the dental follicle proper,8 the outer layer of the dental follicle, the perifollicular mesenchyme7 and the periodontal ligament cells2 are suggested to participate in the development of the gingival connective tissues at the free gingival margin of the tooth, unlike the non-tooth-bearing soft tissues of the oral cavity, which are anatomically devoid of dental follicle and periodontal cells. Developmentally, upon tooth eruption, the lamina propria of the free gingival margin is thought to be formed from cells stemming from the outer layer of the dental follicle.7 Nevertheless, earlier studies demonstrated the presence of fibroblasts stemming from the inner layer of the dental follicle in the free gingival lamina propria at the cemento-enamel junction8 and further suggested that the dentogingival fibre system originates in part from periodontal ligament cells.2 The developmental contribution provided by the dental follicle proper and the periodontal ligament cells to the perifollicular mesenchyme accounts for the anatomical distinctiveness of the free gingival margin from the previously investigated oral soft tissues.
Similar to the first-stage in vivo study,11 the putative stem cell marker STRO-1, which was implemented to isolate and purify bone marrow stromal stem cells28 and alveolar bone proper-derived stem/progenitor cells29 using immunomagnetic cell selection, was used in the current study to isolate multipotent postnatal stem/progenitor cells (MACS+ cells) from heterogeneous gingival connective tissue cells (MACS− cells). This was based on the fact that the latter, in contrast to the targeted multipotent stem/progenitor cells, do not express the distinctive STRO-1 stem/progenitor cell marker.
The MACS+ cell fraction showed all of the previously defined classical characteristics of multipotent postnatal stem/progenitor cells.13,30,31 Regarding the surface marker expression profile, the results showed that MACS+ cells were positive for CD73, CD90, CD105 (all above 95%), CD146/MUC18 and STRO-1, and negative for CD14, CD45 and CD45, in accord with the marker expression profile defined for multipotent stromal cells in the International Society for Cellular Therapy position statement.13 The level of STRO-1 expression was comparable to that observed in the porcine cells in the in vivo study.32 The decrease in the level of STRO-1 expression after the magnetic sorting step has been previously described29,33 and suggests a possible downregulation of the ‘second tier’33 surface marker STRO-1 during the cells' time in culture34 before they reach confluence and attain an adequate cell count to be submitted to flow cytometric analysis. Despite this decrease in expression during culture, the employment of the STRO-1/MACS+ technique resulted in the selection of MACS+ cells that showed all of the ‘first tier’33 stem/progenitor cell surface markers noted in the International Society for Cellular Therapy's predefined percentages and constellation.13 The selected MACS+ cells demonstrated remarkable CFU capacity and showed multilineage differentiation potential, which was evident by their differentiation along the osteogenic, adipogenic and chondrogenic lineages. Finally, unstimulated MACS+ cells expressed all of the tested markers for mineralized tissue.
In contrast, the MACS− cells lacked many of the predefined stem/progenitor cell characteristics,13,30,31 with a different surface marker expression profile from MACS+ cells and almost no expression of CD14 and STRO-1, >95% expression of CD73, CD90 and CD146/MUC18, positive expression of the haematopoietic markers CD34 and CD45, which are not normally expressed in mesenchymal stem/progenitor cells, and CD105 expression below the predefined cutoff of 95%.13 No multilineage differentiation potential was evident in MACS− cells apart from an up-regulation of ALP mRNA expression following osteogenic induction. The uniform staining of glycosaminoglycans observed in the cultures of chondrogenically stimulated MACS− cells and their controls (in sharp contrast to the MACS+ cell controls) demonstrates the fact that MACS− cells harbour the differentiated/committed population of gingival connective tissue cells, which normally lay down glycosaminoglycans (which stain positive for Alcian Blue) as a part of their normal gingival extracellular connective tissue matrix production. This positive staining further underlines the fact that the MACS+ cell controls harboured undifferentiated stem/progenitor cells that were unable to lay down extracellular glycosaminoglycan matrix components in the basic medium. Chondrogenic lacunae-like structures evident in the stimulated MACS+ cells were absent from the stimulated MACS− cells. Expression of the cartilage-specific proteoglycan core protein ACAN was also absent from the MACS− cells.
The common standard markers for mineralized tissue, which are usually used as hallmarks for the identification of multipotent postnatal stem/progenitor cells, including adipose-derived stromal cells35 and bone marrow stromal stem cells,36 were assessed for in the human free gingival margin-derived stem/progenitor cells. Indeed, in the present study, both the free gingival margin-derived stem/progenitor cells (MACS+ cells) and the gingival connective tissue cells (MACS− cells) expressed transcripts encoding most of the tested mineralized tissue markers, albeit in different quantities.
In line with their gingival origin, collagen types I and III were expressed at substantially higher levels in both MACS+ and MACS− cells than were osteonectin and osteopontin.31,32 Significantly higher levels of collagen types I and III were expressed in MACS+ cells than in MACS− cells, along with a tendency to express more ALP. Osteonectin, although minimally expressed in both cell types, was expressed at higher levels in MACS− cells. This is in accord with the results of earlier studies that reported low expression of osteonectin37,38 and osteopontin33 in mature gingival connective tissue. The elevated expression of the late markers osteopontin and osteonectin by the MACS− cells could be considered an indicator of their more differentiated/committed cellular states39,40,41. These findings are consistent with those of earlier studies on mesenchymal stem/progenitor cells and the relationship of their temporal expression of mineralized tissue markers to their cellular developmental process. In terms of matrix synthesis, immature cells are expected to express high levels of early mineralized tissue markers, such as collagen. When the expression of most of the early markers, including collagen, decreases, then the expression of late osteogenic markers increases, denoting a shift from an immature to a more differentiated/committed cellular state39,40,41. In this context, the difference in mineralized tissue marker expression between the immature free gingival margin-derived stem/progenitor cells (MACS+ cells) and the more differentiated/committed gingival connective tissue cells (MACS− cells) can be explained. Whether a time-dependent quantification of the shift in the marker expression profile could be clinically employed to indicate the developmental stage of gingival/periodontal cells remains a very interesting point to be investigated.
Conclusion
The human free gingival margin provides a readily accessible and renewable source of multipotent postnatal stem/progenitor cells that can easily be obtained for cellular approaches for periodontal and other tissues' regeneration. The present results demonstrate that the MACS+ cell population, in contrast to the MACS− population, harbours cells with stem/progenitor cell characteristics, and validate the effectiveness of the STRO-1/MACS+ technique for the isolation of free gingival stem/progenitor cells.
References
Larjava H, Wiebe C, Gallant-Behm C et al. Exploring scarless healing of oral soft tissues. J Can Dent Assoc 2011; 77: b18.
Pitaru S, McCulloch CA, Narayanan SA . Cellular origins and differentiation control mechanisms during periodontal development and wound healing. J Periodont Res 1994; 29 ( 2): 81–94.
Sempowski GD, Borrello MA, Blieden TM et al. Fibroblast heterogeneity in the healing wound. Wound Repair Regen 1995; 3 ( 2): 120–131.
Schor SL, Ellis I, Irwin CR et al. Subpopulations of fetal-like gingival fibroblasts: characterisation and potential significance for wound healing and the progression of periodontal disease. Oral Dis 1996; 2 ( 2): 155–166.
Phipps RP, Borrello MA, Blieden TM . Fibroblast heterogeneity in the periodontium and other tissues. J Periodont Res 1997; 32 ( 1 Pt 2): 159–165.
Häkkinen L, Uitto VJ, Larjava H . Cell biology of gingival wound healing. Periodontol 2000 2000; 24: 127–152.
Cho MI, Garant PR . Development and general structure of the periodontium. Periodontol 2000 2000; 24: 9–27.
Ten Cate AR, Mills C, Solomon G . The development of the periodontium. A transplantation and autoradiographic study. Anat Rec 1971; 170 ( 3): 365–379.
Morsczeck C, Götz W, Schierholz J et al. Isolation of precursor cells (PCs) from human dental follicle of wisdom teeth. Matrix Biol 2005; 24 ( 2): 155–165.
Seo BM, Miura M, Gronthos S et al. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet 2004; 364 ( 9429): 149–155.
Fawzy El-Sayed KM, Paris S, Becker ST et al. Periodontal regeneration employing gingival margin-derived stem/progenitor cells: an animal study. J Clin Periodontol 2012; 39 ( 9): 861–870.
Gottlow J, Nyman S, Karring T et al. New attachment formation as the result of controlled tissue regeneration. J Clin Periodontol 1984; 11 ( 8): 494–503.
Dominici M, Le Blanc K, Mueller I et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006; 8 ( 4): 315–317.
Amin HD, Olsen I, Knowles J et al. A procedure for identifying stem cell compartments with multi-lineage differentiation potential. Analyst 2011; 136 ( 7): 1440–1449.
Paris S, Wolgin M, Kielbassa AM et al. Gene expression of human beta-defensins in healthy and inflamed human dental pulps. J Endod 2009; 35 ( 4): 520–523.
Maehata Y, Takamizawa S, Ozawa S et al. Type III collagen is essential for growth acceleration of human osteoblastic cells by ascorbic acid 2-phosphate, a long-acting vitamin C derivative. Matrix Biol 2007; 26 ( 5): 371–381.
Zhang QZ, Shi SH, Liu Y et al. Mesenchymal stem cells derived from human gingiva are capable of immunomodulatory functions and ameliorate inflammation-related tissue destruction in experimental colitis. J Immunol 2009; 183 ( 12): 7787–7798.
Moshaverinia A, Chen C, Akiyama K et al. Alginate hydrogel as a promising scaffold for dental-derived stem cells: an in vitro study. J Mater Sci Mater Med 2012; 23 ( 12): 3041–3051.
Fournier BP, Larjava H, Häkkinen L . Gingiva as a source of stem cells with therapeutic potential. Stem Cells Dev 2013; 22 ( 24): 3157–3177.
Widera D, Zander C, Heidbreder M et al. Adult palatum as a novel source of neural crest-related stem cells. Stem Cells 2009; 27 ( 8): 1899–1910.
Mitrano TI, Grob MS, Carrión F et al. Culture and characterization of mesenchymal stem cells from human gingival tissue. J Periodontol 2010; 81 ( 6): 917–925.
Marynka-Kalmani K, Treves S, Yafee M et al. The lamina propria of adult human oral mucosa harbors a novel stem cell population. Stem Cells 2010; 28 ( 5): 984–995.
Fournier BP, Ferre FC, Couty L et al. Multipotent progenitor cells in gingival connective tissue. Tissue Eng Part A 2010; 16 ( 9): 2891–2899.
Tomar GB, Srivastava RK, Gupta N et al. Human gingiva-derived mesenchymal stem cells are superior to bone marrow-derived mesenchymal stem cells for cell therapy in regenerative medicine. Biochem Biophys Res Commun 2010; 393 ( 3): 377–383.
Fawzy El-Sayed KM, Dorfer C, Fandrich F et al. Adult mesenchymal stem cells explored in the dental field. Adv Biochem Eng Biotechnol 2013; 130: 89–103.
Fawzy El-Sayed KM, Dorfer C, Fandrich F et al. Erratum to: Adult mesenchymal stem cells explored in the dental field. Adv Biochem Eng Biotechnol 2013; 130: 301–302.
Tang L, Li N, Xie H et al. Characterization of mesenchymal stem cells from human normal and hyperplastic gingiva. J Cell Physiol 2011; 226 ( 3): 832–842.
Gronthos S, Akintoye SO, Wang CY et al. Bone marrow stromal stem cells for tissue engineering. Periodontol 2000 2006; 41: 188–195.
Fawzy El-Sayed KM, Paris S, Becker S et al. Isolation and characterization of multipotent postnatal stem/progenitor cells from human alveolar bone proper. J Craniomaxillofac Surg 2012; 40 ( 8): 735–742.
Bartold PM, Shi S, Gronthos S . Stem cells and periodontal regeneration. Periodontol 2000 2006; 40: 164–172.
Friedenstein AJ, Deriglasova UF, Kulagina NN et al. Precursors for fibroblasts in different populations of hematopoietic cells as detected by the in vitro colony assay method. Exp Hematol 1974; 2 ( 2): 83–92.
Fawzy El-Sayed KM, Paris S, Becker ST et al. Periodontal regeneration employing gingival margin-derived stem/progenitor cells: an animal study. J Clin Periodontol 2012; 39 ( 9): 861–870.
Boxall SA, Jones E . Markers for characterization of bone marrow multipotential stromal cells. Stem Cells Int 2012; 2012: 975871.
Itaya T, Kagami H, Okada K et al. Characteristic changes of periodontal ligament-derived cells during passage. J Periodont Res 2009; 44 ( 4): 425–433.
Wu L, Zhu F, Wu Y et al. Dentin sialophosphoprotein-promoted mineralization and expression of odontogenic genes in adipose-derived stromal cells. Cells Tissues Organs 2008; 187 ( 2): 103–112.
Larsen KH, Frederiksen CM, Burns JS et al. Identifying a molecular phenotype for bone marrow stromal cells with in vivo bone-forming capacity. J Bone Miner Res 2010; 25 ( 4): 796–808.
Tung PS, Domenicucci C, Wasi S et al. Specific immunohistochemical localization of osteonectin and collagen types I and III in fetal and adult porcine dental tissues. J Histochem Cytochem 1985; 33 ( 6): 531–540.
Jeon YM, Kook SH, Son YO et al. Role of MAPK in mechanical force-induced up-regulation of type I collagen and osteopontin in human gingival fibroblasts. Mol Cell Biochem 2009; 320 ( 1/2): 45–52.
Van Vlasselaer P, Falla N, Snoeck H et al. Characterization and purification of osteogenic cells from murine bone marrow by two-color cell sorting using anti-Sca-1 monoclonal antibody and wheat germ agglutinin. Blood 1994; 84 ( 3): 753–763.
Yoon K, Buenaga R, Rodan GA . Tissue specificity and developmental expression of rat osteopontin. Biochem Biophys Res Commun 1987; 148 ( 3 ): 1129–1136.
Lian JB, Stein GS . Development of the osteoblast phenotype: molecular mechanisms mediating osteoblast growth and differentiation. Iowa Orthop J 1995; 15: 118–140.
Acknowledgements
The authors would like to thank Mrs Mojgan Paymard-Stolz, Mrs Regina Marquat, Mrs Hebke Hinz and Mrs Kerstin Marx for their excellent technical assistance. The study was supported in part by a scholarship from the German-Academic-Exchange-Service (DAAD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permissing from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
El-Sayed, K., Paris, S., Graetz, C. et al. Isolation and characterisation of human gingival margin-derived STRO-1/MACS+ and MACS− cell populations. Int J Oral Sci 7, 80–88 (2015). https://doi.org/10.1038/ijos.2014.41
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijos.2014.41
Keywords
This article is cited by
-
Analysis of cell-biomaterial interaction through cellular bridge formation in the interface between hGMSCs and CaP bioceramics
Scientific Reports (2020)
-
Comparative differentiation analysis of distinct oral tissue-derived cells in response to osteogenic stimulation
Clinical Oral Investigations (2019)
-
Mesenchymal stromal/stem cell separation methods: concise review
Cell and Tissue Banking (2017)
-
Vitamin C stimulates human gingival stem cell proliferation and expression of pluripotent markers
In Vitro Cellular & Developmental Biology - Animal (2016)