Abstract
Introduction:
Disruption of circadian rhythms is one of the proposed mechanisms linking late sleep timing to obesity risk but few studies have evaluated biological markers outside of the laboratory. The goal of this study was to determine the relationship between the timing and alignment of melatonin and sleep onset (phase angle) with body mass index (BMI), body fat and obesity-related behaviors. We hypothesized that circadian alignment (relationship of melatonin to sleep timing) rather than circadian (melatonin) timing would be associated with higher BMI, body fat, dietary intake and lower physical activity.
Subjects/Methods:
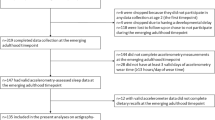
Adults with sleep duration ⩾6.5 h completed 7 days of wrist actigraphy, food diaries and SenseWear arm band monitoring. Circadian timing, measured by dim light melatonin onset was measured in the clinical research unit. Circadian alignment was calculated as the duration between dim light melatonin onset and average sleep onset time in the prior week (phase angle). Body fat was evaluated using dual-energy X-ray absorptiometry. Data were analyzed using bivariate correlations and multivariable regression analyses controlling for age, sex, sleep duration and evening light exposure.
Results:
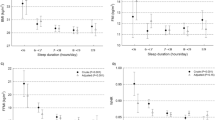
Participants included 97 adults (61 F, age 26.8±7.3 years) with average sleep duration 443.7 (s.d.=50.4) minutes. Average phase angle was 2.2 h (s.d.=1.5). Circadian alignment was associated with circadian timing (P<0.001) and sleep duration (P=0.005). In multivariable analyses, later circadian timing was associated with lower BMI (P=0.04). Among males only, circadian alignment was associated with percent body fat (P=0.02) and higher android/gynoid fat ratio (P=0.04). Circadian alignment was associated with caloric intake (P=0.049) carbohydrate intake (P=0.04) and meal frequency (P=0.03) among both males and females.
Conclusion:
Circadian timing and alignment were not associated with increased BMI or body fat, among healthy adults with ⩾6.5 h of sleep, but circadian alignment was associated with dietary intake. There may be sex differences in the relationship between circadian alignment and body fat.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Arble DM, Ramsey KM, Bass J, Turek FW . Circadian disruption and metabolic disease: findings from animal models. Best Pract Res Clin Endocrinol Metab 2010; 24: 785–800.
Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB . Social Jetlag, Chronotype, and Cardiometabolic Risk. J Clin Endocrinol Metab 2015; 100: 4612–4620.
Merikanto I, Lahti T, Puolijoki H, Vanhala M, Peltonen M, Laatikainen T et al. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol Int 2013; 30: 470–477.
Baron KG, Reid KJ, Kern AS, Zee PC . Role of sleep timing in caloric intake and BMI. Obesity 2011; 19: 1374–1381.
Lucassen EA, Zhao X, Rother KI, Mattingly MS, Courville AB, de Jonge L et al. Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One 2013; 8: e56519.
Arora T, Taheri S . Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes 2015; 39: 39–44.
Sato-Mito N, Shibata S, Sasaki S, Sato K . Dietary intake is associated with human chronotype as assessed by both morningness-eveningness score and preferred midpoint of sleep in young Japanese women. Int J Food Sci Nutr 2011; 62: 525–532.
Baron KG, Reid K . Circadian misalignment and heatlh. Int Rev Psychiatry 2014; 26: 139–154.
Antunes LC, Levandovski R, Dantas G, Caumo W, Hidalgo MP . Obesity and shift work: chronobiological aspects. Nutr Res Rev 2010; 23: 155–168.
Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K et al. A longitudinal study on the effect of shift work on weight gain in male Japanese workers. Obesity (Silver Spring) 2008; 16: 1887–1893.
Ruger M, Scheer FA . Effects of circadian disruption on the cardiometabolic system. Rev Endocr Metab Disord 2009; 10: 245–260.
Sack RL, Auckley D, Auger RR, Carskadon MA, Wright Jr KP, Vitiello MV et al. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep 2007; 30: 1460–1483.
Morris CJ, Yang JN, Garcia JI, Myers S, Bozzi I, Wang W et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc Natl Acad Sci USA 2015; 112: E2225–E2234.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA . Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 2009; 106: 4453–4458.
Buxton OM, Cain SW, O'Connor SP, Porter JH, Duffy JF, Wang W et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 2012; 4: 129ra43.
Gronfier C, Wright Jr KP, Kronauer RE, Czeisler CA . Entrainment of the human circadian pacemaker to longer-than-24-h days. Proc Natl Acad Sci USA 2007; 104: 9081–9086.
Eckel RH, Depner CM, Perreault L, Markwald RR, Smith MR, McHill AW et al. Morning circadian misalignment during short sleep duration impacts insulin sensitivity. Curr Biol 2015; 25: 3004–3010.
Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ et al. Measuring melatonin in humans. J Clin Sleep Med 2008; 4: 66–69.
Burgess HJ, Eastman CI . The dim light melatonin onset following fixed and free sleep schedules. J Sleep Res 2005; 14: 229–237.
Burgess HJ, Savic N, Sletten T, Roach G, Gilbert SS, Dawson D . The relationship between the dim light melatonin onset and sleep on a regular schedule in young healthy adults. Behav Sleep Med 2003; 1: 102–114.
Cain SW, Dennison CF, Zeitzer JM, Guzik AM, Khalsa SB, Santhi N et al. Sex differences in phase angle of entrainment and melatonin amplitude in humans. J Biol Rhythms 2010; 25: 288–296.
Van Reen E, Sharkey KM, Roane BM, Barker D, Seifer R, Raffray T et al. Sex of college students moderates associations among bedtime, time in bed, and circadian phase angle. J Biol Rhythms 2013; 28: 425–431.
Duffy JF, Dijk DJ, Klerman EB, Czeisler CA . Later endogenous circadian temperature nadir relative to an earlier wake time in older people. Am J Physiol 1998; 275: R1478–R1487.
Duffy JF, Zeitzer JM, Rimmer DW, Klerman EB, Dijk DJ, Czeisler CA . Peak of circadian melatonin rhythm occurs later within the sleep of older subjects. Am J Physiol Endocrinol Metab 2002; 282: E297–E303.
Baehr EK, Revelle W, Eastman CI . Individual differences in the phase and amplitude of the human circadian temperature rhythm: with an emphasis on morningness-eveningness. J Sleep Res 2000; 9: 117–127.
Wright Jr KP, Gronfier C, Duffy JF, Czeisler CA . Intrinsic period and light intensity determine the phase relationship between melatonin and sleep in humans. J Biol Rhythms 2005; 20: 168–177.
Wittmann M, Dinich J, Merrow M, Roenneberg T . Social jetlag: misalignment of biological and social time. Chronobiol Int 2006; 23: 497–509.
Lewy AJ, Emens JS, Songer JB, Sims N, Laurie AL, Fiala SC et al. Winter depression: integrating mood, circadian rhythms, and the sleep/wake and light/dark cycles into a bio-psycho-social-environmental model. Sleep Med Clin 2009; 4: 285–299.
Emens J, Lewy A, Kinzie JM, Arntz D, Rough J . Circadian misalignment in major depressive disorder. Psychiatry Res 2009; 168: 259–261.
Hasler BP, Buysse DJ, Kupfer DJ, Germain A . Phase relationships between core body temperature, melatonin, and sleep are associated with depression severity: further evidence for circadian misalignment in non-seasonal depression. Psychiatry Res 2010; 178: 205–207.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C . Social jetlag and obesity. Curr Biol 2012; 22: 939–943.
Radloff LS . The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measure 1977; 1: 385–401.
Ng SS, Chan TO, To KW, Ngai J, Tung A, Ko FW et al. Validation of a portable recording device (ApneaLink) for identifying patients with suspected obstructive sleep apnoea syndrome. Intern Med J 2009; 39: 757–762.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ . The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213.
Voultsios A, Kennaway DJ, Dawson D . Salivary melatonin as a circadian phase marker: validation and comparison to plasma melatonin. J Biol Rhythms 1997; 12: 457–466.
Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ . Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc 2010; 42: 2134–2140.
Fruin ML, Rankin JW . Validity of a multi-sensor armband in estimating rest and exercise energy expenditure. Med Sci Sports Exerc 2004; 36: 1063–1069.
Drenowatz C, Eisenmann JC . Validation of the SenseWear Armband at high intensity exercise. Eur J Appl Physiol 2011; 111: 883–887.
Li C, Ford ES, Zhao G, Balluz LS, Giles WH . Estimates of body composition with dual-energy X-ray absorptiometry in adults. Am J Clin Nutr 2009; 90: 1457–1465.
Kanaley JA, Heden TD, Liu Y, Fairchild TJ . Alteration of postprandial glucose and insulin concentrations with meal frequency and composition. Br J Nutr 2014; 112: 1484–1493.
Heden TD, Liu Y, Sims LJ, Whaley-Connell AT, Chockalingam A, Dellsperger KC et al. Meal frequency differentially alters postprandial triacylglycerol and insulin concentrations in obese women. Obesity (Silver Spring) 2013; 21: 123–129.
Mills JP, Perry CD, Reicks M . Eating frequency is associated with energy intake but not obesity in midlife women. Obesity (Silver Spring) 2011; 19: 552–559.
Reid KJ, Baron KG, Zee PC . Meal timing influences daily caloric intake in healthy adults. Nutr Res 2014; 34: 930–935.
McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc Natl Acad Sci USA 2014; 111: 17302–17307.
Carskadon MA, Acebo C, Jenni OG . Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci 2004; 1021: 276–291.
Boivin DB, Czeisler CA, Dijk DJ, Duffy JF, Folkard S, Minors DS et al. Complex interaction of the sleep-wake cycle and circadian phase modulates mood in healthy subjects. Arch Gen Psychiatry 1997; 54: 145–152.
Borbely AA . A two process model of sleep regulation. Hum Neurobiol 1982; 1: 195–204.
Baker FC, Driver HS . Circadian rhythms, sleep, and the menstrual cycle. Sleep Med 2007; 8: 613–622.
Heo M, Faith MS, Pietrobelli A, Heymsfield SB . Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–2004. Am J Clin Nutr 2012; 95: 594–602.
Benloucif S, Guico MJ, Reid KJ, Wolfe LF, L'Hermite-Baleriaux M, Zee PC . Stability of melatonin and temperature as circadian phase markers and their relation to sleep times in humans. J Biol Rhythms 2005; 20: 178–188.
Wyatt JK, Stepanski EJ, Kirkby J . Circadian phase in delayed sleep phase syndrome: predictors and temporal stability across multiple assessments. Sleep 2006; 29: 1075–1080.
Sletten TL, Vincenzi S, Redman JR, Lockley SW, Rajaratnam SM . Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol 2010; 1: 137.
Fonken LK, Nelson RJ . The effects of light at night on circadian clocks and metabolism. Endocr Rev 2014; 35: 648–670.
Acknowledgements
We thank Leland Bardsley, Leah Hecht, David Clough and Lori Koch for their assistance with data collection and analyses. Research reported in this publication was supported, in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant Number UL1TR000150 and by the National Institute of Health’s Heart Lung Blood and Sleep Institute Grant Number 1K23HL109110-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Support: grants 1K23HL109110-01, UL1TR000150.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Zee reports she is a consultant for Merck, Philips, Research grants to Northwestern University from Jazz Pharmaceuticals and stock ownership in Teva Pharmaceuticals. The remaining authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Baron, K., Reid, K., Kim, T. et al. Circadian timing and alignment in healthy adults: associations with BMI, body fat, caloric intake and physical activity. Int J Obes 41, 203–209 (2017). https://doi.org/10.1038/ijo.2016.194
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.194
This article is cited by
-
Identification of the Relationship Between DNA Methylation of Circadian Rhythm Genes and Obesity
Biochemical Genetics (2024)
-
Circadian Timing, Information processing and Metabolism (TIME) study: protocol of a longitudinal study of sleep duration, circadian alignment and cardiometabolic health among overweight adults
BMC Endocrine Disorders (2023)
-
Circadian Factors in Stroke: A Clinician’s Perspective
Cardiology and Therapy (2023)
-
Shift Work and Obesity Risk—Are There Sex Differences?
Current Diabetes Reports (2022)
-
Late bedtime is associated with lower weight loss in patients with severe obesity after sleeve gastrectomy
International Journal of Obesity (2021)