Abstract
Study objectives:
To investigate the potential association between snoring and other symptoms indicative of sleep-disordered breathing and metabolic syndrome (MetS) in Hispanic adolescents and younger adults using a large population-based survey.
Methods:
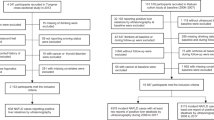
Sleep-related information, anthropometric measurements and fasting blood samples markers of MetS were obtained from subjects aged 15–40 years collected through the 2nd Chilean Health Survey. Regression models were constructed to evaluate the associations of snoring with MetS, hypertension and serum cholesterol levels. The modulating effect of sleep duration was accounted for in the models.
Results:
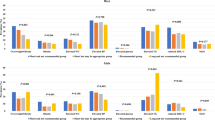
A total of 2147 subjects (42% males, mean age 27.9±7.6 years) were included. Snoring and short sleep duration were present in 43.5 and 25% of the entire population, respectively. MetS was detected in 19.5% of the subjects. In the adjusted regression model, the odds of MetS among snoring subjects were 2.13 times higher (95% confidence interval (CI): 1.52–2.99; P<0.01), and 1.53-fold higher odds of elevated cholesterol also emerged (95% CI: 1.12–2.10; P<0.01). However, the odds of hypertension were not increased by the presence of snoring after adjusting for confounders. In addition, snoring was associated with an increase of 7.26 and 6.56 mg dl−1 for total and low-density lipoprotein cholesterol, respectively, even after adjusting for age, sex and body mass index. Short sleep duration was associated with a small albeit significant risk increase for high systolic blood pressure.
Conclusions:
In this large population-based sample of young Hispanic adults and adolescents, snoring, but not sleep duration, emerged as an independent risk factor for dyslipidemia and MetS, but not for hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Redline S, Storfer-Isser A, Rosen CL, Johnson NL, Kirchner HL, Emancipator J et al. Association between metabolic syndrome and sleep-disordered breathing in adolescents. Am J Respir Crit Care Med 2007; 176: 401–408.
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G . Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol 2013; 62: 569–576.
Gileles-Hillel A, Kheirandish-Gozal L, Gozal D . Biological plausibility linking sleep apnoea and metabolic dysfunction. Nat Rev Endocrinol 2016; 12: 290–298.
Sharma SK, Kumpawat S, Goel A, Banga A, Ramakrishnan L, Chaturvedi P . Obesity, and not obstructive sleep apnea, is responsible for metabolic abnormalities in a cohort with sleep-disordered breathing. Sleep Med 2007; 8: 12–17.
Hakim F, Kheirandish-Gozal L, Gozal D . Obesity and altered sleep: a pathway to metabolic derangements in children? Semin Pediatr Neurol 2015; 22: 77–85.
Gozal D, Capdevila OS, Kheirandish-Gozal L . Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med 2008; 177: 1142–1149.
Lam JC, Lam B, Lam CL, Fong D, Wang JK, Tse HF et al. Obstructive sleep apnea and the metabolic syndrome in community-based Chinese adults in Hong Kong. Respir Med 2006; 100: 980–987.
Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB . Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep 2008; 31: 635–643.
Schmid SM, Hallschmid M, Schultes B . The metabolic burden of sleep loss. Lancet Diabetes Endocrinol 2015; 3: 52–62.
St Onge MP, Schechter MS . Sleep disturbances, body fat distribution, food intake and/or energy expenditure: pathophysiological aspects. Horm Mol Biol Clin Investig 2014; 17: 29–37.
Koren D, Levitt Katz LE, Brar PC, Gallagher PR, Berkowitz RI, Brooks LJ . Sleep architecture and glucose and insulin homeostasis in obese adolescents. Diabetes Care 2011; 34: 2442–2447.
Tasali E, Chapotot F, Wroblewski K, Schoeller D . The effects of extended bedtimes on sleep duration and food desire in overweight young adults: a home-based intervention. Appetite 2014; 80: 220–224.
Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ . The association between self-reported sleep quality and metabolic syndrome. PLoS One 2013; 8: e54304.
Rangaraj VR, Knutson KL . Association between sleep deficiency and cardiometabolic disease: implications for health disparities. Sleep Med 2016; 18: 19–35.
Schafer H, Pauleit D, Sudhop T, Gouni-Berthold I, Ewig S, Berthold HK . Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest 2002; 122: 829–839.
Pallayova M, Steele KE, Magnuson TH, Schweitzer MA, Hill NR, Bevans-Fonti S et al. Sleep apnea predicts distinct alterations in glucose homeostasis and biomarkers in obese adults with normal and impaired glucose metabolism. Cardiovasc Diabetol 2010; 9: 83.
Ip MS, Lam KS, Ho C, Tsang KW, Lam W . Serum leptin and vascular risk factors in obstructive sleep apnea. Chest 2000; 118: 580–586.
Peppard PE, Young T, Palta M, Skatrud J . Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000; 342: 1378–1384.
Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP . Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J 2004; 25: 735–741.
Tsaoussoglou M, Bixler EO, Calhoun S, Chrousos GP, Sauder K, Vgontzas AN . Sleep-disordered breathing in obese children is associated with prevalent excessive daytime sleepiness, inflammation, and metabolic abnormalities. J Clin Endocrinol Metab 2010; 95: 143–150.
Canapari CA, Hoppin AG, Kinane TB, Thomas BJ, Torriani M, Katz ES . Relationship between sleep apnea, fat distribution, and insulin resistance in obese children. J Clin Sleep Med 2011; 7: 268–273.
Koren D, Gozal D, Bhattacharjee R, Philby MF, Kheirandish-Gozal L . Impact of Adenotonsillectomy on insulin resistance and lipoprotein profile in nonobese and obese children. Chest 2016; 149: 999–1010.
Koren D, Gozal D, Philby MF, Bhattacharjee R, Kheirandish-Gozal L . Impact of obstructive sleep apnoea on insulin resistance in nonobese and obese children. Eur Respir J 2016; 47: 1152–1161.
Alexopoulos EI, Gletsou E, Kostadima E, Kaditis D, Zakynthinos E, Gourgoulianis K et al. Effects of obstructive sleep apnea severity on serum lipid levels in Greek children with snoring. Sleep Breath 2011; 15: 625–631.
Tauman R, O'Brien LM, Ivanenko A, Gozal D . Obesity rather than severity of sleep-disordered breathing as the major determinant of insulin resistance and altered lipidemia in snoring children. Pediatrics 2005; 116: e66–e73.
Chilean Ministry of Health. Chilean National Health Survey, 2nd ed. 2010. Available at: www.redsalud.gov.cl.
Brockmann PE, Damiani F, Gozal D . Sleep-disordered breathing in adolescents and younger adults: a representative population-based survey in Chile. Chest 2015; 149: 981–990.
Bouscoulet LT, Vazquez-Garcia JC, Muino A, Marquez M, Lopez MV, de Oca MM et al. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med 2008; 4: 579–585.
Hirshkowitz M, Whiton K, Albert SA, Alessi C, Bruni O, DonCarlos L et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 2015; 1: 40–43.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB . The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med 2003; 163: 427–436.
Hjorth MF, Chaput JP, Damsgaard CT, Dalskov SM, Andersen R, Astrup A et al. Low physical activity level and short sleep duration are associated with an increased cardio-metabolic risk profile: a longitudinal study in 8-11 year old Danish children. PLoS One 2014; 9: e104677.
Holst-Schumacher I, Nuñez-Rivas H, Monge-Rojas R, Barrantes-Santamaría M . Components of the metabolic syndrome among a sample of overweight and obese Costa Rican schoolchildren. Food Nutr Bull 2009; 30: 161–170.
de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N . Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation 2004; 110: 2494–2497.
Casavalle PL, Lifshitz F, Romano LS, Pandolfo M, Caamano A, Boyer PM et al. Prevalence of dyslipidemia and metabolic syndrome risk factor in overweight and obese children. Pediatr Endocrinol Rev 2014; 12: 213–223.
Verhulst SL, Schrauwen N, Haentjens D, Rooman RP, Van Gaal L, De Backer WA et al. Sleep-disordered breathing and the metabolic syndrome in overweight and obese children and adolescents. J Pediatr 2007; 150: 608–612.
Chung JY, Kang HT, Shin YH, Lee HR, Park BJ, Lee YJ . Prevalence of metabolic syndrome in children and adolescents - the recent trends in South Korea. J Pediatr Endocrinol Metab 2013; 26: 105–110.
De Ferranti SD, Osganian SK . Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res 2007; 4: 285–296.
Gozal D, Kheirandish-Gozal L . Obesity and excessive daytime sleepiness in prepubertal children with obstructive sleep apnea. Pediatrics 2009; 123: 13–18.
Marcus JA, Pothineni A, Marcus CZ, Bisognano JD . The role of obesity and obstructive sleep apnea in the pathogenesis and treatment of resistant hypertension. Curr Hypertens Rep 2014; 16: 411.
Drager LF, Lopes HF, Maki-Nunes C, Trombetta IC, Toschi-Dias E, Alves MJ et al. The impact of obstructive sleep apnea on metabolic and inflammatory markers in consecutive patients with metabolic syndrome. PLoS One 2010; 5: e12065.
Bhattacharjee R, Choi BH, Gozal D, Mokhlesi B . Association of adenotonsillectomy with asthma outcomes in children: a longitudinal database analysis. PLoS Med 2014; 11: e1001753.
Verhulst SL, Aerts L, Jacobs S, Schrauwen N, Haentjens D, Claes R et al. Sleep-disordered breathing, obesity, and airway inflammation in children and adolescents. Chest 2008; 134: 1169–1175.
Teodorescu M, Barnet JH, Hagen EW, Palta M, Young TB, Peppard PE . Association between asthma and risk of developing obstructive sleep apnea. JAMA 2015; 313: 156–164.
Agrawal A, Mabalirajan U, Ahmad T, Ghosh B . Emerging interface between metabolic syndrome and asthma. Am J Respir Cell Mol Biol 2011; 44: 270–275.
Kheirandish-Gozal L, Dayyat EA, Eid NS, Morton RL, Gozal D . Obstructive sleep apnea in poorly controlled asthmatic children: effect of adenotonsillectomy. Pediatr Pulmonol 2011; 46: 913–918.
Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G . Sleep in America: role of racial/ethnic differences. Sleep Med Rev 2013; 17: 255–262.
Patel SR, Sotres-Alvarez D, Castaneda SF, Dudley KA, Gallo LC, Hernandez R et al. Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic Community Health Study/Study of Latinos. Sleep 2015; 38: 1515–1522.
Mossavar-Rahmani Y, Jung M, Patel SR, Sotres-Alvarez D, Arens R, Ramos A et al. Eating behavior by sleep duration in the Hispanic Community Health Study/Study of Latinos. Appetite 2015; 95: 275–284.
Redline S, Sotres-Alvarez D, Loredo J, Hall M, Patel SR, Ramos A et al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med 2014; 189: 335–344.
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 2015; 3: 310–318.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Leiby BE, Vela-Bueno A et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160: 2289–2295.
Marcus JA, Bisognano JD . Screening for severe obstructive sleep apnea syndrome in hypertensive outpatients. J Clin Hypertens (Greenwich) 2013; 15: 289–290.
Bhattacharjee R, Kim J, Alotaibi WH, Kheirandish-Gozal L, Capdevila OS, Gozal D . Endothelial dysfunction in children without hypertension: potential contributions of obesity and obstructive sleep apnea. Chest 2012; 141: 682–691.
Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016; 374: 2430–2440.
Acknowledgements
We thank the Chilean Health Ministry (MINSAL) and its Department of Public Health for designing and conducting the second National Health Survey 2009–2010 and providing the corresponding database. We also wish to thank FONDECYT project number 11130573 for supporting the analysis conducted in this study. Chilean Health Ministry (MINSAL) founded the 2nd National Health Survey 2009–2010 used for this study and FONDECYT project number 11130573 the analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Brockmann, P., Damiani, F., Smith, D. et al. Metabolic consequences of snoring in adolescents and younger adults: a population study in Chile. Int J Obes 40, 1510–1514 (2016). https://doi.org/10.1038/ijo.2016.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.133
This article is cited by
-
The association between obstructive sleep apnea syndrome and metabolic syndrome: a confirmatory factor analysis
Sleep and Breathing (2019)
-
Role of sleep duration and sleep-related problems in the metabolic syndrome among children and adolescents
Italian Journal of Pediatrics (2018)