Abstract
Background:
There is a lack of common surveillance systems providing comparable figures and temporal trends of the prevalence of overweight (OW), obesity and related risk factors among European preschool and school children. Comparability of available data is limited in terms of sampling design, methodological approaches and quality assurance. The IDEFICS (Identification and prevention of Dietary- and lifestyle-induced health Effects in Children and infantS) study provides one of the largest European data sets of young children based on state-of-the-art methodology.
Objective:
To assess the European distribution of weight status according to different classification systems based on body mass index (BMI) in children (2.0–9.9 years). To describe the prevalence of weight categories by region, sex, age and socioeconomic position.
Design:
Between 2007 and 2010, 18 745 children from eight European countries participated in an extensive, highly standardised protocol including, among other measures, anthropometric examinations and parental reports on socio-demographic characteristics.
Results:
The combined prevalence of OW/obesity ranges from more than 40% in southern Europe to less than 10% in northern Europe. Overall, the prevalence of OW was higher in girls (21.1%) as compared with boys (18.6%). The prevalence of OW shows a negative gradient with social position, with some variation of the strength and consistency of this association across Europe. Overall, population groups with low income and/or lower education levels show the highest prevalence of obesity. The use of different reference systems to classify OW results in substantial differences in prevalence estimates and can even reverse the reported difference between boys and girls.
Conclusions:
There is a higher prevalence of obesity in populations from southern Europe and in population groups with lower education and income levels. Our data confirm the need to develop and reinforce European public health policies to prevent early obesity and to reduce these health inequalities and regional disparities.
Similar content being viewed by others
Introduction
The prevalence of paediatric overweight (OW)/obesity has become a well-recognised public health problem in Europe as well as in other developed countries. The estimated prevalence of OW (including obesity) in children and adolescents is about 20% in the World Health Organization (WHO) European Region with large differences between countries and socioeconomic groups.1,2 Routine surveillance of OW and obesity is therefore crucial to evaluate the success of policies that aim to reduce excess weight in childhood and eventually halt the ongoing obesity epidemic. However, reliable comparisons between countries are hampered by the use of non-standardised anthropometric measurement methods and varying sampling designs, response proportions and age ranges.3 In addition, different criteria have been used to define OW and obesity in children, leading to considerable variation in prevalence estimates.4
To address this gap, we pooled and re-analysed, using standardised criteria, several existing databases of surveys on childhood OW and obesity—in particular, data from surveys carried out by research groups participating in the IDEFICS (Identification and prevention of Dietary- and lifestyle-induced health Effects in Children and infantS) project in different European countries during the period 1995–2005.5 This exercise confirmed that the validity of comparisons between communities critically depends on the comparability of the survey methods.
Recently, the WHO initiated a common surveillance system to provide comparable figures and time trends of the prevalence of OW, obesity and related risk factors among European children. The results of data collected in 2007/2008 in 12 European countries were published in 2013.6 These data are restricted to the age group 6–9 years and anthropometric variables are restricted to height and weight.6 A recent review based on existing European data showed that information on OW and obesity in preschool children is scarce and that its interpretation is difficult, especially because of different definitions and methods of data collection and analysis—again highlighting the need for standard survey methods in these age groups.7
To date, the IDEFICS study (Identification and prevention of dietary- and lifestyle-induced health effects in children and infants) provides one of the largest European data sets of children from 2.0–9.9 years of age. Although not intended to be strictly nationally representative, the study provides population-based samples that were drawn from communities considered to be typical of their geographical region. Thus, the study sample is informative in describing the distribution of children’s weight status across eight European countries.
The full description of the design and methods of the study and of the large set of variables collected, based on state-of-the-art methodology, has been reported elsewhere.8,9 For the purpose of the present analysis, we use anthropometric measures and indicators of social position like parental education and family income.
In the present analysis, we report the prevalence of weight status categories in eight European regions participating in the IDEFICS study. We describe how prevalence varies by region, sex, age and social position, and also how it varies depending on the cut-offs used, including the body mass index (BMI) categories proposed by International Obesity Task Force (IOTF) and WHO.
Subjects and methods
A short description of the IDEFICS study is provided here. Further details on the overall design, the study protocol and characteristics of the participants can be found in Ahrens et al.9
Study subjects
A cohort of 16 228 children aged 2.0–9.9 years was examined in a population-based baseline survey in eight European countries ranging from north to south and from east to west (Sweden, Germany, Hungary, Italy, Cyprus, Spain, Belgium, Estonia) from autumn 2007 to spring 2008. As indicated, the study was not designed to provide a representative sample for each country. Rather, this baseline survey (T0) was the starting point of the prospective study and constitutes the largest European children’s cohort established to date.9 The total study sample (n=18 745) is comprised of this cohort plus an additional 2517 children aged 2.0–10.9 years who were newly recruited during a second survey (T1) 2 years later. Exactly the same survey modules were deployed at baseline (T0) and at follow-up (T1).
All children in the defined age group who resided in the study regions and who attended the selected primary schools (grades 1 and 2), preschools or kindergartens were eligible for participation. Children were approached via schools and kindergartens to facilitate equal enrolment of all social groups. The minimum requirements for inclusion in the analysis group were valid measurements of height and weight as well as the completion of the parental questionnaire. In addition to the signed informed consent given by parents, each child was asked to give verbal assent immediately before examination. In addition, approval by the local ethics committees was obtained by each of the survey centres.
Questionnaires and examinations
Parents filled in a self-completion questionnaire to assess gestational, behavioural and socio-demographic factors. This included educational attainment according to the International Standard Classification of Education,10 family income (using country-specific categories based on the average net equivalence income), employment status, dependence on social welfare and migration background. Parents also completed a children’s eating habits questionnaire on frequency of food consumption and dietary habits.
The examination programme included standard anthropometric measures11 (see also Nagy et al.,12 this issue) such as weight, height, skinfolds, waist circumference and bioelectrical impedance. The measurement of weight was carried out using an electronic scale (Tanita BC 420 SMA, Tanita Europe, Sindelfingen, Germany) to the nearest 0.1 kg. The children wore only underwear and a T-shirt. Barefoot height was measured using a telescopic height measuring instrument (Seca 225 stadiometer, seca, Birmingham, UK) to the nearest 0.1 cm.
Quality management
All measurements followed detailed standard operation procedures.13 Field personnel from each study centre participated in central training. Adherence of field staff to the standard operation procedures was checked during on-site visits. Questionnaires were developed in English, translated to local languages and then back-translated to check for translation errors. All study centres used the same technical equipment. Databases and computer-assisted questionnaires included automated plausibility checks. All numerical variables were entered twice independently. To further check the quality of data, subsamples of study subjects were examined repeatedly to calculate the inter- and intraobserver reliability of anthropometric measurements:14 the inter- and intraobserver technical error of height measurement was 2.7 and 2.1 cm, respectively, wheraes the inter- and intraobserver technical error of weight measurement was 65 and 55 g, respectively. In addition, the reliability of questionnaires was checked by re-administering selected items of the parental questionnaire to a convenience sample of study participants.15,16
Reference systems to classify the weight status of children
Reference systems that are currently used to describe the weight status of children are based on age- and sex-specific BMI. There is an ongoing debate of the limitations of BMI as a measure of adiposity in children, but there are also several publications that show the usefulness of this simple and robust anthropometric parameter and its high correlation with other measures of adiposity.17,18 At least nine different reference systems have been commonly used to classify OW/obesity in children and adolescents (see Ahrens et al.,19 for an overview). Because these are derived from different populations at different points in time and rely on different methodologies, any prevalence estimates strongly depend on the reference applied. We chose the following four systems for comparison purposes:
-
The reference system of the IOTF20 is based on survey data from six countries in North and South America, Asia and Europe collected between 1963 and 1993. Percentile curves were drawn for each survey such that they passed through the BMI values of 25 and 30 kg/m2 for adult OW and obesity at age 18 years. The resulting curves were averaged to provide age- and sex-specific cut-off points from 2–18 years. These correspond to the 88th (female) and 90th (male) percentile for OW and the 99th percentile for obesity. These calculations were updated by Cole and Lobstein in 2012.21
-
The WHO Child Growth Standards were initially derived for children aged 0–5 years. These growth charts are based on a sample of healthy breastfed infants and young children—assessed between 1997–2003 in Brazil, Ghana, India, Norway, Oman and USA—who were raised under living conditions considered to not constrain growth.22 To model growth curves for school-aged children and adolescents that fit to these growth charts for preschool children and that also align with the BMI cut-offs for adults, data from the 1977 National Center for Health Statistics/WHO growth reference (1–24 years) were merged with data from the above sample (18–71 months) to smooth the transition between the two samples.23 Based on age- and sex-specific z-scores derived from this data set, OW is defined as z⩾1 and obesity as z⩾2.
-
The Centers for Disease Control and Prevention growth charts for the United States24 are based on the US surveys NHES II and III and NHANES I-III conducted between 1963 and 1994 that overlap with the above National Center for Health Statistics data. These charts use the 85th and 95th percentiles of the sex-specific BMI growth curves as cut-offs for OW and obesity, respectively.
-
The reference curves by Kromeyer–Hauschild25 are based on 17 pooled regional surveys conducted in Germany between 1985 and 1999. They use the sex- and age-specific 90th and 97th percentiles as cut-offs.
Statistical analysis
The analysis database is summarised by country-specific distributions of the children across 1-year-old categories. Sex-specific prevalences of thinness, normal weight, OW and obesity are calculated according to Cole and Lobstein21 stratified by country and social position measured by the International Standard Classification of Education (maximum of both parents) and income. We abstain from showing sex-specific tables and figures as a default as long as trends and distributions are largely similar for boys and girls, as these figures and tables are not meant as references from which to read off age- and sex-specific cut-offs. Prevalences of OW and obesity are also calculated according to three other common classification systems22, 23, 24, 25 to allow comparisons with studies that use these classification systems and to assess the impact of different systems on the prevalence estimates.
Results
Participation
We obtained valid data from 51% of children who were invited to take part in the baseline survey. The lowest response proportions were reached in Spain (41%) and Hungary (44%), and the highest in Italy (60%) and Sweden (66%).9 We excluded the age group 10.0–10.9 years, because this age stratum was almost missing in some countries and the number of children was too small to be broken down further, for example, by weight (see Table 2). Overall, 9331 boys and 9170 girls were included in the analysis (Table 1). The analysis group was comparable to the total sample with regard to the age distribution, the attained educational level and income (Table 1). The variable income was missing in 18%—mainly due to item non-response. In addition, we set income levels for all Hungarian children newly recruited at T1 to missing because their values were no longer comparable given that Hungary had suffered from severe inflation between T0 and T1. Sex was about evenly distributed in each age stratum and each country. The total number of children, however, varied by country, ranging from 1539 children in Spain to 3159 children in Hungary. Each 1-year age stratum between 3.0 and 8.9 years included more than 2300 (up to more than 4000) children. The lowest (2.0–2.9) and highest (9.0–9.9) age categories included about 600 children each (see Table 2).
BMI categories by study region, sex, age and social position
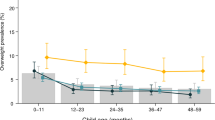
Figure 1 displays the prevalence of four weight categories by country according to the IOTF cut-offs as recently updated by Cole and Lobstein.21 Overall, 7% of the study sample was classified as obese and 12.8% as OW. The highest prevalence of OW and obesity was observed in the Italian (42.4%), Cypriot (23.4%) and Spanish (21.2%) study regions, whereas the lowest prevalence was observed in Belgium (9.4%) and Sweden (11.0%). Overall, we observed a slightly higher prevalence of OW and obesity in girls (21.1%) as compared with boys (18.6%). This tendency was observed in all countries (Table 3). Among preschool children, in particular, girls had a higher prevalence of OW and obesity than boys, whereas this difference was smaller in primary school children (Figure 2, bottom left).
Prevalence of weight categories according to Cole and Lobstein21 by study region (boys and girls combined; number of subjects displayed in bars).
Figure 3 displays the association between weight status and social position according to the variables family income (a) and parental educational attainment (b). Both variables were negatively associated with the prevalence of OW and obesity while they were positively associated—although less strongly—with the proportion of thin children. The strength of these associations was similar in boys and girls. Overall, the prevalence of OW and obesity ranged from 28.8–12.3% and from 29.3–15.9% in the lowest and highest category of income and education, respectively. However, the strength and consistency of this gradient vary across Europe. The prevalence of obesity declines linearly and strongly with income level in Belgium, Germany, Spain and Cyprus, whereas this trend is less strong and/ or less consistent in Sweden, Estonia, Hungary and Italy (Table 4). The inverse association of the obesity prevalence with parental educational attainment is most pronounced in Germany, Spain, Sweden and Cyprus and less strong in Italy, Hungary, Belgium and Estonia (Table 5). These associations are analysed in depth in Bammann et al.26 The prevalence values shown in Tables 4 and 5 are broken down by sex in Supplementary Tables A and B.
Prevalence of weight categories according to Cole and Lobstein21 by income level (a) and by parental education (b) (boys and girls combined; number of subjects displayed in bars).
Comparison of OW/ obesity prevalence by BMI reference systems
Figure 4 displays the age-specific prevalence of OW and obesity combined according to the cut-offs provided by IOTF,21 WHO,22,23 CDC24 and by Kromeyer–Hauschild et al.25 The WHO cut-offs classified the greatest percentage of children as OW or obese (28.4%), followed by CDC (24.2%) and IOTF cut-offs (19.8%), whereas the smallest proportion was classified according to Kromeyer–Hauschild (16.3%). The differences between the classification systems are not uniform across age groups. For example, prevalences according to IOTF and WHO show their maximum difference at age 2–2.9 (14.5 percentage points). This difference stabilises at school age to a level of about 7% points.
The observed differences are consistent across countries and sexes although, as previously reported by Wijnhoven et al.,6 more boys than girls are classified as OW or obese according to WHO, whereas the reference values published by Cole and Lobstein21 show a higher prevalence in girls (see Figure 2). The other two reference systems do not show consistent differences between boys and girls.
Discussion
The IDEFICS surveys, carried out from 2007–2010, provide one of the largest and most up-to-date data sets on the lifestyle and health status of European children. Highly standardised objective measurements of height and weight were obtained from a total of 18 501 girls and boys, aged 2.0–9.9 years, from eight European countries.
About 20% of children were identified as OW/obese according to the IOTF classification, compared with 28.4% according to the WHO classification. Regardless of the classification system, the prevalence of OW and obesity in European children remains high and, given the tracking of body weight from childhood to adult age and its health sequelae, this represents a major public health concern. However, the burden imposed by early obesity is not uniformly distributed in Europe, as indicated by the striking differences between European regions participating in the IDEFICS study. As already suggested by other cross-countries reports,2,5,6 children residing in southern European countries show the highest prevalence of OW and obesity. In our study, the highest proportions were observed in southern Italy (OW and obesity: boys, 40.7%; girls 43.1%), followed by Cyprus and Spain. Although the descriptive data presented here do not allow an aetiological interpretation, there is accumulating evidence that several risk factors for childhood obesity are most prevalent in Mediterranean populations. This is true for lack of physical activity (see Konstabel et al.;27 this issue), insufficient sleep duration,28 non-adherence to a (so-called!) Mediterranean diet29 (see also Tognon et al.,30 this issue), and exposure to TV viewing and excess screen time.31,32
The impact of social position on the risk of obesity in developed countries has been clearly demonstrated in adults;33 data for children are less consistent but nonetheless suggestive.34 As pointed out by Johnson et al.,35 there are various measures to classify social position of which parental education has shown the most consistent association with OW in childhood. Johnson et al. thus argue that economic factors are not the primary drivers of the association of social position with OW and obesity observed in western countries. The causality of this association, however, may be questioned; certainly, it remains unclear whether nutritional education and better knowledge of healthy eating would diminish the elevated risk of obesity in children of less educated parents. There are further mediating factors that have to be considered when assessing the causality of the association between social position and childhood obesity.35 Our results clearly confirm the inverse relationship between the prevalence of OW and obesity in children and the social position of the family, either measured as family income or as parental educational attainment.
The interpretation of income levels requires some caution because we had to apply country-specific cut-offs to define income categories. Also, family income was missing in a relatively high proportion of children—mainly due to item non-response. However, even though minor changes in assigning reported family incomes to one of the six categories resulted in substantial increases or reductions of the number of children in the middle income strata in some countries, the overall association with the prevalence of OW and obesity remained quite stable.
There is general consensus that studies of childhood obesity prevalence should be reported according to different references.4 In epidemiological settings, the IOTF21 and WHO22,23 definitions should be used, possibly complemented by additional references such as the CDC24 or national references.25 In order to make the results of our analysis useful for comparison at the international level, we reported the prevalence of OW and obesity in eight European countries according to four classifications. Besides the internationally adopted IOTF and WHO classifications, we also calculated prevalence of OW and obesity according to the CDC cut-offs and to the Kromeyer–Hauschild references, the latter being particularly used in Central Europe countries.
The advantages and limitations of the different classification systems for OW and obesity in childhood have been extensively discussed.3,4,36,37 The higher prevalence of obesity observed using the WHO references is consistent with previous reports.36,38 The difference between the IOTF and the WHO classification system is not uniform across age groups. It shows a maximum at early age, decreases until school age and then remains about constant until the age of 10. In their systematic review of the clinical and epidemiological definitions of childhood obesity, Reilly et al.37 noted that the IOTF classification may underestimate the prevalence of excess weight, particularly obesity, in children and adolescents when compared with national reference standards. Despite this, the same authors rated the value of this classification for international comparisons as high.37 Thus, the differences observed in IDEFICS as well as in other recent studies illustrate the need to consider the applied reference systems in interpreting and comparing prevalence data from different sources. At the same time, the methodological approaches of sampling and measurement have to be taken into account.
A strength of the present study is the use of highly standardised measurement methods across the eight European countries participating in the surveys. As indicated, all measurements were conducted by trained personnel according to detailed standard operating procedures. In particular, subsamples of study subjects were examined repeatedly to calculate the inter- and intraobserver reliability of anthropometric measurements.14
The limitations of the IDEFICS study have been extensively discussed in a previous paper.9 We are aware of the fact that BMI is not the ideal measure of adiposity, as it is an indicator of both fat mass and fat-free mass. However, as discussed above, BMI is highly correlated with other measures of adiposity, and it is a robust measure most widely used in population-based studies that facilitates the assessment of temporal trends and allows for comparisons with other studies on a population level.
An important issue is the representativeness of the European population samples participating in the surveys. In the accompanying editorial of this special issue, compelling arguments are offered to justify the use of an unselected population sample, such as the IDEFICS cohort, for the assessment of prevalences and reference values. It is particularly interesting to note that the prevalence data reported in this paper are comparable to those recently published by the WHO European Childhood Obesity Surveillance Initiative.6 The two data sets, although different with regard to geographical regions, methodology, sample size and age range, confirmed the scale of the problem of childhood OW and obesity in Europe, including the large prevalence variations between countries. An added value of the IDEFICS study is the assessment of OW and obesity in preschool children, which fills a previous lack in our knowledge.7
In conclusion, the IDEFICS study has generated the first fully comparable data on the prevalence of OW and obesity in children below the age of 10 years across Europe. Our findings may serve as a reference for the comparison of the prevalence of OW and obesity in childhood at the national and the European level. In addition, they confirm the need to develop and reinforce European public health policies to prevent early obesity. Given the higher prevalence in Southern Europe and population groups with low education and low income, we believe there is a special need to reduce health inequalities and regional disparities. Finally, the follow-up of the IDEFICS cohort in the ongoing I.Family study39 will augment our database and allow the investigation of changes in body composition from early childhood to adolescence in Europe.
References
Branca F, Nikogosian H, Lobstein T (eds). The Challenge of Obesity in the WHO European Region and the Strategies for Response. WHO Regional Office for Europe: Copenhagen, Denmark, 2007.
Manios Y, Costarelli V . Childhood obesity in the WHO European Region. In: Moreno LA, Pigeot I, Ahrens W (eds). Epidemiology of Obesity in Children and Adolescents—Prevalence and Etiology, vol. 2. Springer Series on Epidemiology and Public Health. Springer: New York, NY, USA, 2011, pp 43–68.
Rodríguez G, Pietrobelli A, Wang Y, Moreno LA . Methodological aspects for childhood and adolescence obesity epidemiology. In: Moreno LA, Pigeot I, Ahrens W (eds). Epidemiology of Obesity in Children and Adolescents—Prevalence and Etiology, vol. 2. Springer Series on Epidemiology and Public Health. Springer: New York, USA, 2011, pp 21–40.
Rolland-Cachera MF . Childhood obesity: current definitions and recommendations for their use. Int J Pediatr Obes 2011; 6: 325–331.
Pigeot I, Barba G, Chadjigeorgiou C, de Henauw S, Kourides Y, Lissner L et al. Prevalence and determinants of childhood overweight and obesity in European countries: pooled analysis of the existing surveys within the IDEFICS Consortium. Int J Obes (Lond) 2009; 33: 1103–1110.
Wijnhoven TM, van Raaij JM, Spinelli A, Rito AI, Hovengen R, Kunesova M et al. WHO European Childhood Obesity Surveillance Initiative 2008: weight, height and body mass index in 6-9-year-old children. Pediatr Obes 2013; 8: 79–97.
Cattaneo A, Monasta L, Stamatakis E, Lioret S, Castetbon K, Frenken F et al. Overweight and obesity in infants and pre-school children in the European Union: a review of existing data. Obes Rev 2010; 11: 389–398.
Ahrens W, Bammann K, De Henauw S, Halford J, Palou A, Pigeot I et al. European Consortium of the IDEFICS Project. Understanding and preventing childhood obesity and related disorders—IDEFICS: a European multilevel epidemiological approach. Nutr Metab Cardiovasc Dis 2006; 16: 302–308.
Ahrens W, Bammann K, Siani A, Buchecker K, De Henauw S, Iacoviello L et al. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes 2011; 35: S3–15.
International Standard Classification of Education (ISCED). UNESCO 1997 http://www.unesco.org/education/information/nfsunesco/doc/isced_1997.htm (last accessed January 2014).
Marfell-Jones M, Olds T, Stewart A, Carter L . International Standards for Anthropometric Assessment. International Society for the Advancement of Kinanthropometry: Potchefstroom, South Africa, 2006.
Nagy P, Kovacs E, Moreno LA, Veidebaum T, Tornaritis M, Kourides Y et al. Percentile reference values for anthropometric body composition indices in European children from the IDEFICS study. Int J Obes (Lond) 2014; 38 (Suppl 2): S15–S25.
Suling M, Hebestreit A, Peplies J, Bammann K, Nappo A, Eiben G et al. Design and results of the pretest of the IDEFICS study. Int J Obes 2011; 35: S30–S44.
Stomfai S, Bammann K, De Henauw S, Kovács É, Marild S, Moreno LA et al. Intra- and inter-observer reliability in anthropometric measurements in children. Int J Obes 2011; 35: S45–S51.
Lanfer A, Hebestreit A, Ahrens W, Krogh V, Sieri S, Lissner L et al. Reproducibility of food consumption frequencies derived from the Children's Eating Habits Questionnaire used in the IDEFICS study. Int J Obes 2011; 35: S61–S68.
Herrmann D, Suling M, Reisch L, Siani A, De Bourdeaudhuij I, Maes L et al. Repeatability of maternal report on prenatal, perinatal and early postnatal factors: findings from the IDEFICS parental questionnaire. Int J Obes 2011; 35: S52–S60.
Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB . Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatr 1998; 132: 204–210.
Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH . Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr 2002; 75: 978–985.
Ahrens W, Moreno LA, Pigeot I . Childhood obesity: prevalence worldwide—synthesis part I. In: Moreno LA, Pigeot I, Ahrens W (eds). Epidemiology of Obesity in Children and Adolescents—Prevalence and Etiology, vol. 2. Springer Series on Epidemiology and Public Health Springer: New York, USA, 2011, pp 219–235.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J 2000; 320: 1240–1243.
Cole TJ, Lobstein T . Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012; 7: 284–294.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 2006; 450: 76–85.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660–667.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 2002; 246: 1–190.
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V et al. Perzentile für den Body-Mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschrift Kinderheilkunde 2001; 149: 807–818.
Bammann K, Gwozdz W, Lanfer A, Barba G, De Henauw S, Eiben G et al. IDEFICS Consortium. Socioeconomic factors and childhood overweight in Europe: results from the multi-centre IDEFICS study. Pediatr Obes 2013; 8: 1–12.
Konstabel K, Veidebaum T, Verbestel V, Moreno LA, Bammann K, Tornaritis M et al. Objectively measured physical activity in European children: the IDEFICS study. Int J Obes (Lond) 2014; 38 (Suppl 2): S135–S143.
Hense S, Pohlabeln H, De Henauw S, Eiben G, Molnar D, Moreno LA et al. Sleep duration and overweight in European children: is the association modified by geographic region? Sleep 2011; 34: 885–890.
Tognon G, Hebestreit A, Lanfer A, Moreno LA, Pala V, Siani A et al. Mediterranean diet, overweight and body composition in children from eight European countries: Cross-sectional and prospective results from the IDEFICS study. Nutr Metab Cardiovasc Dis 2013; 24: 205–213.
Tognon G, Moreno LA, Mouratidou T, Veidebaum T, Molnár D, Russo P et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int J Obes (Lond) 2014; 38 (Suppl 2): S108–S114.
Santaliestra-Pasías AM, Mouratidou T, Verbestel V, Bammann K, Molnar D, Sieri S et al. Physical activity and sedentary behaviour in European children: the IDEFICS study. Public Health Nutr 2013; doi:10.1017/S1368980013002486.
Lissner L, Lanfer A, Gwozdz W, Olafsdottir S, Eiben G, Moreno LA et al. Television habits in relation to overweight, diet and taste preferences in European children: the IDEFICS study. Eur J Epidemiol 2012; 27: 705–715.
McLaren L . Socioeconomic status and obesity. Epidemiol Rev 2007; 29: 29–48.
Shrewsbury V, Wardle J . Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990-2005. Obesity (Silver Spring) 2008; 16: 275–284.
Johnson F, Pratt M, Wardle W Socio-economic status and obesity in childhood. In: Moreno LA, Pigeot I, Ahrens W (eds). Epidemiology of Obesity in Children and Adolescents—Prevalence and Etiology, vol. 2. Springer Series on Epidemiology and Public Health. Springer: New York, USA, 2011, pp 377–390.
Monasta L, Lobstein T, Cole TJ, Vignerová J, Cattaneo A . Defining overweight and obesity in pre-school children: IOTF reference or WHO standard? Obesity Rev 2011; 12: 295–300.
Reilly JJ, Kelly J, Wilson DC . Accuracy of simple clinical and epidemiological definitions of childhood obesity: systematic review and evidence appraisal. Obesity Rev 2010; 11: 645–655.
Shields M, Tremblay MS . Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes 2010; 5: 265–273.
I.Family.I.Family Consortium 2014. www.ifamilystudy.eu (last accessed January 2014).
Acknowledgements
This work was done as part of the IDEFICS Study (www.idefics.eu). We gratefully acknowledge the financial support of the European Community within the Sixth RTD Framework Programme Contract No. 016181 (FOOD). The authors wish to thank the IDEFICS children and their parents for participating in the extensive examination procedures involved in this study. We are grateful for the support by school boards, headmasters and communities. We are also grateful to the Volkswagen Foundation that financially supported the production of this supplement. The information in this document reflects the authors’ view and is provided as is. LL has received grant support from VR, FORTE and FORMAS (research councils in Sweden).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Approval by the appropriate Ethics Committees was obtained by each of the 8 centres doing the fieldwork. Study children did not undergo any procedures unless both they and their parents had given consent for examinations, collection of samples, subsequent analysis and storage of personal data and collected samples. Study subjects and their parents could consent to single components of the study while abstaining from others.
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Ahrens, W., Pigeot, I., Pohlabeln, H. et al. Prevalence of overweight and obesity in European children below the age of 10. Int J Obes 38 (Suppl 2), S99–S107 (2014). https://doi.org/10.1038/ijo.2014.140
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.140
This article is cited by
-
Early sex-dependent differences in metabolic profiles of overweight and adiposity in young children: a cross-sectional analysis
BMC Medicine (2023)
-
Could interventions on physical activity mitigate genomic liability for obesity? Applying the health disparity framework in genetically informed studies
European Journal of Epidemiology (2023)
-
Body surface area-based kidney length percentiles misdiagnose small kidneys in children with overweight/obesity
Pediatric Nephrology (2023)
-
Association between maternal and paternal employment and their children’s weight status and unhealthy behaviours: does it matter who the working parent is?
BMC Public Health (2022)
-
Characteristics of paediatric foot arches according to body mass among primary school students in Wrocław, Poland
BMC Pediatrics (2022)