Abstract
Objective:
Recently a genome-wide association analysis from five European populations identified a polymorphism located downstream of the mannosyl-(α-1,3)-glycoprotein-β-1,2-N-acetylglucosaminyltransferase (MGAT1) gene that was associated with body-weight. In the present study, associations between MGAT1 variants combined with obesity and insulin measurements were investigated in three cohorts. Levels of fatty acids and estimated measures of Δ desaturases were also investigated among adult men.
Design:
Six polymorphisms downstream of MGAT1 were genotyped in a cross-sectional cohort of 1152 Swedish men. Three polymorphisms were further analyzed in a case-control study of 1076 Swedish children and in a cross-sectional study of 2249 Greek children.
Results:
Three polymorphisms, rs12186500 (odds ratio (OR): 1.892, 95% confidence interval (CI): 1.237–2.895, P=0.003), rs1021001 (OR: 2.102, 95% CI: 1.280–3.455, P=0.003) and rs4285184 (OR: 1.587, 95% CI: 1.024–2.459, P=0.038) were associated with a higher prevalence of obesity among the adult men and a trend for obesity was observed for rs4285184 among the Swedish (OR: 1.205, 95% CI: 0.987–1.471, P=0.067) and Greek children (OR: 1.192, 95%CI: 0.978–1.454, P=0.081). Association with body weight was observed for rs12186500 (P=0.017) and rs4285184 (P=0.024) among the men. The rs1021001 and rs4285184 were also associated with body mass index (BMI) in the two Swedish cohorts and similar trends were observed among the Greek children. The combined effect size for rs1021001 and rs4285184 on BMI z-score from a meta-analysis was 0.233 (95% CI:0.093–0.373, P=0.001) and 0.147 (95% CI:0.057–0.236, P=0.001), respectively. We further observed associations between the genetic variants and fatty acids (P<0.039) and estimated measures of Δ desaturases (P<0.040), as well as interactions for rs12186500 (P<0.019) with an effect on BMI. No association was found with homeostatic model assessment-insulin resistance in any cohort but increased insulin levels, insulin response and decreased insulin sensitivity were observed among the children (P<0.038).
Conclusion:
Genetic variants downstream MGAT1 seem to influence susceptibility to obesity. Moreover, these genetic variants affect the levels of serum unsaturated fatty acids and Δ desaturase indices, variables previously shown to correlate with obesity.
Similar content being viewed by others
Introduction
The prevalence of obesity increases tremendously in most countries, almost with epidemic proportions. The environmental contribution to obesity is apparent but a genetic component can explain as much as 50–70% of the variation in body weight.1 One approach to identifying genes that are associated with obesity and obesity related phenotypes is genome-wide association studies (GWAs). During the last few years a number of genome-wide association studies have identified novel candidate genes for obesity.2, 3, 4, 5, 6, 7 Recently a genome-wide association analysis was conducted for body weight and body mass index (BMI) in 3448 subjects from five geographically and environmental distinct European populations, included in the EUROSPAN (European Special Population Network) project. This study identified a gender specific single nucleotide polymorphism (SNP), not previously reported, which was significantly associated with body weight among women (7.3 × 10−8).8 This genetic variant, rs12517906, is located 45 kb downstream of the mannosyl (α-1,3)-glycoprotein β-1,2-N-acetylglucosaminyltransferase (MGAT1) gene and is part of one of two partially connected linkage disequilibrium (LD) blocks.
MGAT1 encodes a transmembrane protein located in the medial compartment of the golgi apparatus with its catalytic domain within the lumen.9, 10 MGAT1 is a typical housekeeping gene but there are two MGAT1 transcripts in humans with the larger one being exclusively expressed in the brain.11 MGAT1 catalyzes the first step in the conversion of oligomannose to N-glycans of glycoproteins.12, 13 Proteins on the cell surface that are N-glycosylated by MGAT1 are required for cell–cell interactions and for the binding of cytokines and other factors to the outer cell membrane. N-linked glycosylation is further important for the folding of some eukaryotic proteins.14
Post-translational modification, like glycosylation, can affect the function of a single gene and mutations in these glycosylation proteins may therefore have great effects on the development of normal cells.15 Null mutations of mouse Mgat1 have shown that this gene has a fundamental role in the normal development 16, 17, 18 and mutation or dysregulation of several enzymes dependent on MGAT1 action are associated with human diseases.19, 20, 21
In the present study, we replicated the previously studied rs12517906 in a population of Swedish men and explored the genomic region further by genotyping an additional five neighboring SNPs that might have an effect on metabolic conditions of men. As no study has been carried out among children we further genotyped three SNPs among children and explored a possible gender effect. In order to study ethnical differences, the study on children included one Swedish and one Greek cohort. The association between these SNPs and obesity was investigated in the three cohorts. Furthermore, we examined the association with body weight, BMI, insulin measurements and levels of serum fatty acids as well as whether BMI or insulin sensitivity is modified by the level of these fatty acids.
Subjects and methods
Uppsala Longitudinal Study of Adult Men (ULSAM)
The ULSAM is a population-based cohort initiated in 1970 and, described previously.22 All men born between 1920 and 1924 and residing in Uppsala, Sweden, were invited to participate in a health survey; 82% of the invited men participated (n=2322). The design and selection criteria for the cohort have been described previously.23 At baseline, age 50 years, height was measured to the nearest centimeter and body weight to the nearest kilogram. BMI was calculated as body weight divided by height squared (kg m−2). BMI z-score was calculated by subtracting the mean BMI from individual BMI and then dividing the difference with the standard deviation. Blood glucose, serum insulin concentrations during an intravenous glucose tolerance test, insulin response and homeostatic model assessment-insulin resistance (HOMA-IR) were measured and determined as described previously.24 For analysis of the fatty acid composition of the serum cholesterol esters, serum was extracted with a hexane-isopropanol solution (1+4) The percentage composition of methylated fatty acids 14:0 to 20:5 was determined by gas chromatography (a 25 m NB-351 silica capillary column, i.d. 0.32 mm, phase layer 0.20 mm) with the use of a flame ionization detector and with helium as carrier gas. The ratio between 20:4 (n-6)/20:3 (n-6), 18:3 (n-6)/18:2 (n-6) and 16:1 (n-7)/16:0 was used as indices of Δ-5 desaturase, Δ-6 desaturase and Δ-9 desaturase, respectively. Hypertension prevalence was defined as hypertension treatment and/or a supine diastolic blood pressure of 95 mm Hg or higher. Hyperlipidemia prevalence was defined as serum cholesterol above 6.5 mmol l−1 and/or serum triglycerides above 2.3 mmol l−1 and/or lipid-lowering medication. Diabetes prevalence was defined as fasting blood glucose above or equal to 6.7 mmol l−1 and glucose tolerance (indicated as the K-value from intravenous glucose tolerance test) less or equal to 0.9 or anti-diabetic therapy. Of the initial cohort of 2322 men, DNA was available for 1152 men obtained from examination at 70 years of age. Measurements of serum fatty acids were available for 958 men obtained from examination at 50 years of age. The study was approved by the Ethics committee of Uppsala University, Faculty of Medicine. All participants gave their written informed consent.
Swedish children and adolescents
The cohort of Swedish children and adolescents comprised two groups as described previously.25 One group consisting of 551 severely obese children (286 girls and 265 boys) enrolled at National Childhood Obesity Centre at Karolinska University Hospital, Huddinge and the second group consisting of 525 healthy and normal weight Swedish adolescents (270 girls and 255 boys) recruited from 17 upper secondary schools in the Stockholm area, Sweden. Body weight and height were measured to the nearest 0.1 kg and 1 cm, respectively. BMI z-score was calculated relative to The International Obesity Task Force (IOTF) definitions.26 Genomic DNA from all subjects (n=1076) was extracted from peripheral blood using QiaGen Maxiprep kit (Qiagen, Hilden, Germany). Among the obese subjects, the level of serum insulin was analyzed from blood samples drawn after 12-h overnight fasting. Insulin resistance was assessed through the homeostasis model assessment (HOMA=(insulin (mU l−1) × glucose (mmol l−1))/22.5) and insulin response was calculated using the Bergman minimal model approach.27, 28 The study was approved by the Regional Committee of Ethics, Stockholm.
Greek children and adolescents
The cohort of Greek children comprised 2 658 school children, attending the 5th and 6th grades of primary schools located in municipalities within the prefectures of Attica, Aitoloakarnania, Thessaloniki and Iraklio. This cohort was part of the ‘Healthy Growth Study’, a large-scale cross-sectional epidemiological study initiated in May 2007 and completed in June 2009. An extended letter explaining the aims of the current study and a consent form were provided to each parent who had a child in one of the primary schools participating in the study. Those parents who agreed to participate in the study had to sign the consent form and provide their contact details. Body weight and height were measured in all study participants using standard procedures and equipment. Body weight was measured to the nearest 10 g using a Seca digital scale (Seca Alpha, Model 770, Hamburg, Germany). Subjects were weighed without shoes in the minimum clothing possible. Height was measured to the nearest 0.1 cm using a commercial stadiometer (Leicester Height Measure, Invicta Plastics Ltd, Oadby, UK) in standing position, not wearing shoes, and keeping shoulders in a relaxed position, arms hanging freely and head aligned in Frankfurt plane. BMI z-score was calculated relative to the International Obesity Task Force definitions.26 Blood samples were obtained for biochemical and hematological screening tests after a 12-h overnight fast. Blood was centrifuged for plasma separations at 3000 r.p.m. for 15 min. Aliquots were stored at −80 °C until further analyses. The level of plasma glucose was determined using a commercially available enzymatic colorimetric assay (Roche Diagnostics, Visalia, Switzerland). The level of serum insulin was determined by using a chemiluminescence immunoassay (Kyowa Medex Ltd, Minami-Ishiki, Japan). Insulin resistance was assessed through the homeostasis model assessment (HOMA=(insulin (μU ml−1) × glucose (mmol l−1))/22.5). DNA for genotyping was available for 2249 subjects (1116 girls and 1133 boys). Approval to conduct the study was granted by the Greek Ministry of National Education and the Ethical Committee of Harokopio University of Athens.
Genotyping and (LD) analysis
Six SNPs located downstream of MGAT1, rs17702447, rs12517906, rs12186500, rs6886113, rs1021001 and rs4285184 were genotyped in the ULSAM cohort. Three of these, rs1286500, rs1021001 and rs4285184 were further genotyped in the Swedish and Greek cohort of children and adolescents. The genotyping of MGAT1 SNPs in the ULSAM cohort was carried out at the SNP technology platform at Uppsala University (http://www.genotyping.SE/) using an Illumina GoldenGate Assay (Illumina Inc., San Diego, CA, USA).29 The genotype call rate in the samples was 96.8%. The genotyping in the Swedish and Greek children and adolescents was carried out with pre-designed Taqman single-nucleotide polymorphism genotyping assays (Applied Biosystems, Foster City, CA, USA) and an ABI7900 genetic analyzer with SDS 2.2 software at the Uppsala Genome Center (http://www.genpat.uu.se/node462). The genotype call rate was 94.8 and 98.2%, respectively. Test for deviation from Hardy–Weinberg equilibrium was performed using the Pearson's χ2-test (1 d.f.) and none of the SNPs did deviate from Hardy Weinberg equilibrium in any of the studied groups. Haploview30 was used for LD measurements according to confidence intervals (CIs) by Gabriel et al.31 as well as graphical representation of the LD structure indicated as r2. The LD pattern was generated using HapMap data version 3, release 27 and CEU+TSI as analysis panel and the ULSAM data.
Statistical analyses
Among the Swedish men, subjects were categorized as normal weight (BMI <25 kg m−2), overweight (BMI ⩾25 kg m−2) and obese (⩾30 kg m−2) Among the children and adolescents, subjects were categorized as overweight and obese using International Obesity Task Force BMI cut-off values equivalent to adult BMI of 25 and 30, respectively. Association with overweight and obesity was analyzed with logistic regression and odds ratio (OR) with a 95% (CI). Associations between genotypes and phenotypes were analyzed in each cohort with linear regression, assuming an additive model. Quantitative skewed variables were normalized by transformation before analysis. For the ULSAM cohort, covariates such as BMI, height, age as well as diabetes, hypertension and hyperlipidemia prevalence were tested for dependence on the response variables and included in the model if significant. Interaction between genotype and fatty acids on body weight, BMI levels as well as HOMA-IR was analyzed by introducing an interaction term (genotype × fatty acid) in the model and the subjects were stratified into low and high levels of fatty acids based on the median level in the cohort. Among the children and adolescents, the models were adjusted for age, gender, BMI and height when needed and interaction between genotype and gender was analyzed by introducing an interaction term (genotype × gender). Statistical analyses were performed with PLINK (http://pngu.mgh.harvard.edu/purcell/plink/).32 Combined analysis was performed for BMI z-score using meta-analysis with MIX 1.7 (http://www.meta-analysis-made-easy.com/about/index.html).33 Due to the number of SNPs and phenotypes tested the significant levels in the different cohorts were adjusted with the false discovery rate according to the procedure of Benjamini and Hochberg.34 A P-value less than 0.041, 0.040 and 0.047 was considered statistically significant in the ULSAM cohort, the Swedish cohort of children and in the cohort of Greek children, respectively.
Power calculations
For the case/control analyses, power calculations were carried out for each SNPs with the CaTS power calculator (http://www.sph.umich.edu/csg/abecasis/CaTS/index.html).35 In the ULSAM cohort and for each SNP we had 80% power to detect association with overweight and obesity with a relative risk of 1.34 and 1.70, respectively. Among the Swedish children we had 80% power to detect association with obesity with a relative risk of 1.40 and among the Greek children we had 80% power to detect association with overweight and obesity with a relative risk of 1.20 and 1.40, respectively.
Results
Samples
In this study, three different groups were analyzed and descriptive characteristics are presented in Table 1. The first cohort consists of men from the ULSAM. Of the total number of 1152 subjects, age 50 years, 563 (48.8%) were considered normal weight, 589 (51.1%) had a BMI over 25 kg m−2 and 54 (4.6%) had a BMI over 30 kg m−2 and were considered overweight and obese, respectively. The second study group consisted of 525 Swedish normal weight adolescents (270 girls and 255 boys) and 551 Swedish obese children and adolescents (286 girls and 265 boys). The third study group comprised 2249 Greek children (1140 girls and 1109 boys) from a large-scale cross-sectional epidemiological study initiated in 2007. In all 1305 (58.0%) of the children were normal weight, 944 (41.9%) were overweight and 267 (11.8%) were considered obese.
Genotyping and LD evaluation
Six SNPs were genotyped in the ULSAM cohort, one previously studied by Johansson et al.8
According to the LD structure based on HapMap data these SNPs are parts of two different haplotype blocks downstream MGAT1 (Figure 1a). Based on the ULSAM data, four of the genotyped SNPs, rs17702447, rs12517906, rs12186500 and rs6886113 were tag SNPs located in one block and the remaining two, rs1021001 and rs4285184 were located in the second block (Figure 1b). Pair-wise LD tests between the SNPs revealed an overall weak LD except between rs17702447 and rs12517906 (r2=94) (Figure 1b). Due to this strong LD between rs17702447 and rs12517906, rs17702447 was not further analyzed. Three of the SNPs were furthermore genotyped among children and adolescents and the same LD structure as among the men was observed but the pair-wise LD pattern for the Greek children revealed an overall weaker LD for the three genotyped markers (rs12186500-rs1021001 r2=8%, rs1021001-rs4285184 r2=41%, rs12186500-rs4285184 r2=11%).
(a) Schematic structure of MGAT1 and the LD pattern based on HapMap data (v3, release 27 and CEU+TSI). The black triangles indicates haplotype blocks defined by CI according to Gabriel et al.31 The diamonds represent the pair wise r2 (black r2>0.8, dark gray 0.8–0.5, moderate gray 0.6–0.4, light gray 0.4–0.2 and white r2<0.2). (b) The LD is expressed as r2 between the pairs of five SNPs genotyped in the ULSAM cohort. The haplotype analysis was performed using Haploview 4.1.30
Obesity association analyses
The effect of the studied variants on overweight and obesity was analyzed in the three cohorts (Table 2). None of the variants were associated with overweight among the adult men but carriers of the minor allele of rs1286500 (OR: 1.892, 95% CI: 1.237–2.895, P=0.003), rs1021001 (OR: 2.102, 95% CI: 1.280–3.455, P=0.003) and rs4285184 (OR: 1.587, 95% CI: 1.024–2.459, P=0.038), had higher odds for having obesity than non-carriers. Due to previously reported gender differences for rs125179068 a possible interaction, among the children, between genotype and gender was studied. However, no gender interaction was found for the Swedish or the Greek samples for any of the studied variants (rs1286500 P=0.122/0.125, rs1021001 P=0.103/0.988, rs4285184 P=0.214/0.364). Among the Swedish children, no association with obesity was observed for rs12186500 (OR: 1.028, 95% CI: 0.863–1.223, P=0.759), but both rs1021001 (OR: 1.193, 95% CI: 0.924–1.539, P=0.086) and rs4285184 (OR: 1.205, 95% CI: 0.987–1.471, P=0.067) showed P-values that were close to significant. These findings were replicated in the Greek cohort of children and for rs4285184 there was a difference in allele frequency between obese and normal weight subjects, but this did not reach statistical significance (OR 1.192, 95% CI: 0.978–1.454, P=0.081). No association between overweight or obesity was observed for the other two SNPs.
Anthropometric associations
Associations between the studied genetic variants and anthropometric data, such as body weight and BMI were also investigated in the three cohorts (Table 3). No gender genotype interaction was found among the children in body weight or BMI for any of the studied variants (P>0.05 for all). Among the Swedish men, carriers of the minor allele of rs1021001 (MAF 12.3%) and rs4285184 (MAF 21.4%) had significantly higher BMI levels compared with carriers of the major allele (P=0.014 and P=0.020) and carriers of the minor allele of rs4285184 had also significantly higher body weight (P=0.024) compared with non-carriers. The rs1286500 was associated with higher body weight (P=0.017, MAF 37.0%) and carriers of the minor allele also exhibited increased BMI levels, but did not reach statistical significance (P=0.085). No association with body weight or BMI was found for the previously associated variant, rs12517906 (MAF 13.1%) (body weight P=0.795, BMI P=0.464). Among the Swedish children and adolescents, carriers of the minor allele of rs1021001 (MAF: normal weight 12.0%, obese 15.0%) had higher BMI compared with non-carriers and showed increased body weight (Table 3). This was observed both among the normal weight (body weight P=0.048, BMI P=0.009) and the obese subjects (body weight P=0.041, BMI P=0.004). The rs4285184 (MAF: normal weight 24.0%, obese 27.0%) was associated with body weight (P=0.038) and BMI (P=0.033) among the normal weight subjects and with BMI (P=0.025) among the obese subjects. The genetic variant, rs12186500 (MAF: normal weight 45.1%, obese 45.8%), was not associated with body weight among the Swedish children (normal weight P=0.734, obese P=0.801) as it was among the Swedish adult men. Among the Greek children we observed increased body weight for carriers of the minor allele of rs1021001 (MAF 13.4%), which however did not reached statistical significance (P=0.081) (Table 3).
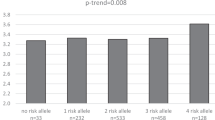
To study the combined effect on BMI a meta-analysis was performed for two of the SNPs, rs1021001 and rs4285184 (Figure 2). The mean BMI z-score for carriers of the common homozygote was compared with carriers of the rare homozygote in the four groups. The rare homozygote had a combined higher mean level of BMI z-score for both SNPs, 0.233 (95% CI 0.093–0.373, P=0.001) for rs1021001 and 0.147 (95% CI 0.057–0.236, P=0.001) for rs4285184. There was no evidence of heterogeneity between risk estimates for the two SNPs (rs1021001: P=0.867, l2=0% and rs4285184: P=0.513, l2=0%).
Fatty acid associations
Serum fatty acids function as biomarkers for long-term dietary fat intake but also reflect the endogenous fatty acid synthesis. As serum fatty acids and desaturase indices have been related to obesity36 we sought to further investigate levels of obesity associated fatty acids among the adult men. Carriers of the minor allele of three of the studied variants, rs12517906 (MAF 13.1%), rs12186500 (MAF 37.0%) and rs4285184 (MAF 21.4%), had decreased levels of linoleic acid (18:2 (n-6)) (Table 4). Increased levels of palmitoleic acid (16:1 (n-7)) were observed for all variants and were significantly different for rs12186500, rs1021001 and rs4285184 (Table 4). Furthermore, carriers of the minor allele of four of the studied variants, rs12186500 (MAF 37.0%), rs6886113 (MAF 20.1%), rs1021001 (MAF 12.3%) and rs4285184 (MAF 21.4%), had increased levels of Δ-6 desaturase and rs1021001 and rs4285184 were also associated with increased Δ-9 desaturase activity (Table 4). In addition, increased levels of γ-linolenic acid (18:3 (n-6)) for the minor allele were observed for rs12186500. To study if the fatty acids and desaturases modulate the observed genetic effects of MGAT1 on body weight and BMI, the interaction between fatty acids and the studied SNPs was analyzed. For BMI, we observed interactions between rs12186500 and arachidonic acid (P=0.0001), γ-linolenic acid (P=0.008), Δ-6 desaturase (P=0.019) and Δ-9 desaturase (P=0.007). When the subjects were stratified into low and high levels of these measurements based on the median levels in the cohort, the association between BMI and rs12186500 was observed among subjects with high levels of γ-linolenic acid (P=0.010), arachidonic acid (P=0.003), Δ-6 desaturase (P=0.042) and Δ-9 desaturase (P=0.026) whereas no association was seen among subjects with low levels (γ-linolenic acid P=0.354, arachidonic acid P=0.853, Δ-6 desaturase P=0.501, Δ-9 desaturase P=0.559). No interactions were observed between the studied SNPs and fatty acids or desaturases on body weight (P>0.05 for all).
Insulin measurements
We also investigated genetic effects on a number of insulin measurements in our subjects (Table 5). Among the obese Swedish children, carriers of the minor allele of rs1021001 (MAF 15.0%), rs12186500 (MAF 45.8%) and rs4285184 (MAF 27.0%) exhibited increased insulin response (rs1021001 P=0.001, rs12186500 P=0.012, rs4285184 P=5.5x10−5) and decreased insulin sensitivity (rs1021001 P=0.030, rs12186500 P=0.015, rs4285184 P=0.007). Among the Greek children, carriers of the minor allele of rs1021001 (P=0.038) and rs4285184 (P=0.009) had increased insulin levels. Increased insulin levels were also observed among the Swedish children that carried the minor allele of rs4285184, which, however, did not reach statistical significance (P=0.046). No main effect was observed on HOMA-IR for any of the studied variants in any of the three cohorts (Table 5). As we found increased levels of palmitoleic acid and decreased levels of linoleic acid among men that were carriers of the minor allele, and as fatty acids are known to affect insulin sensitivity,37 we also investigated the interaction between MGAT1 variants and fatty acids on HOMA-IR. However, no interaction was found for any of the variants among the adult men (P>0.05 for all).
Discussion
In this study, we investigated polymorphisms near the MGAT1 gene and their effect on obesity, in three different cohorts. We first studied six SNPs, one previously reported to be associated with body weight,8 in a cohort of adult men. These six SNPs make up two haplotype blocks covering the 5′ end of MGAT1, four SNPs belonging to one block and two belonging to the second (Figure 1). The rs12186500 in the first block and rs1021001 and rs4285184 in the second haplotype were also genotyped in two cohorts of Swedish and Greek children and adolescents. The rs12517906 did not associate with overweight or obesity or to the other measurements of obesity such as body weight and BMI among the Swedish men, which support the previous finding of an association that is only found among women for this variant.8 We did, however, observe higher odds for obesity for three other SNPs, rs12186500, rs1021001 and rs4285184 among the adult men and a trend for obesity for rs4285184 among both the Swedish and Greek children (Table 2). Carriers of the minor allele of rs1021001 and rs4285184 had furthermore higher body weight and BMI levels compared with carriers of the major allele in both Swedish cohorts (Table 3). This data indicate that the SNPs in the second haplotype block, which are in LD with the coding exon of MGAT1, seem to be more involved in BMI and body weight regulation than the SNPs in the first block.
As we found increased BMI levels and body weight for carriers of the minor allele of rs1021001 and rs4285184 among both Swedish adults and children, these variants seem to affect subjects in all ages (Table 3). Furthermore, these associations were found among both obese and normal weight children, and with no gender effect, which indicate that these variants seem to affect body weight and BMI in younger ages of both sexes regardless of their BMI status. In older ages, however, these genetic variants seem to affect body weight and BMI more among the extremes as we observed higher odds for obesity but not overweight.
The Greek children had an overall lower allele frequency and weaker LD between the markers than the Swedish subjects indicating ethnic differences for these variants and may explain why only trends were observed among the Greek subjects. Ethnical differences were also observed in the previous GWA study of five geographically distinct European populations, rs12517906 was highly significantly associated with weight in their meta-analysis but only reached nominal significance in two of the individual population samples.8 Despite these differences we observed evidence of an association with BMI z-score for rs1021001 and rs4285184 for all cohorts. The combined effect size for the two SNPs on BMI z-score from our meta-analysis was 0.3 and 0.1, respectively.
The mechanism(s) by which these SNPs near the MGAT1 gene may contribute to the observed associations is unclear. Given that the analyzed SNPs map to non-coding regions, the likelihood that any of these SNPs represent the causal variant is low. However, these genetic variants are both in LD with the coding exon in MGAT1, a key enzyme involved in glycosylation of proteins and lipids.38 Changes in MGAT1 expression caused by these variants may lead to altered glycosylation, which may affect proteins and lipids that are dependent on complete glycosylation. An altered glycosylation may cause misdirected sorting of these proteins and alter their function,38 which in turn may be important for body weight regulation.
Serum fatty acid composition is a biomarker for long term dietary fat intake, but also reflects endogenous fatty acid synthesis.39 The latter could also be influenced by genetic variation and hormonal (for example, obesity-related hyperinsulinemia) factors.39 The analyzed fatty acids have all been correlated with obesity markers such as BMI.37 Especially, Δ-6 and Δ-9 desaturases show a strong positive association with obesity.37 Furthermore, we have recently shown that variants in the Δ-9 desaturase gene are associated with obesity in adult men.40 Changed levels of serum palmitoleic acid due to altered Δ-9 desaturase activation have also a significant relation to obesity in children.41 In the present study the MGAT1genetic variants are in addition to obesity and BMI, associated with altered fatty acid composition, for example, linoleic acid and palmitoleic acid, which may be due to disturbance in the activation of Δ-6 desaturase and Δ-9 desaturase, respectively. However, whether these associations are causal remains to be elucidated. In addition, we observed interactions between rs12186500, and γ-linolenic acid, arachidonic acid, Δ-6 and Δ-9 desaturase. Carriers of the minor allele of rs12186500 with high levels of these fatty acids and desaturases had significantly higher BMI than carriers of the major allele. The observed interaction with γ-linolenic acid and arachidonic acid might also be due to altered Δ-6 desaturase activity.
As increased levels of fatty acids are known to be one of the factors inducing insulin resistance37 and that the men in the present study who were carriers of the minor allele also had elevated levels of fatty acids, we hypothesized that these subjects might also have an increased risk of developing insulin resistance. We observed in addition an increased insulin response and decreased insulin sensitivity among the obese children. We found, however, no interaction effect between these SNPs and fatty acids on HOMA-IR among the Swedish men, so the altered fatty acid levels caused by the variants in MGAT1 do not seem to modulate an increased insulin resistance.
In conclusion, we genotyped six SNPs downstream MGAT1 in a cohort of Swedish adult men and observed associations with obesity as well as increased body weight and BMI levels for some of these variants. Two of them also associated with body weight and BMI levels among Swedish children and similar trends were observed among Greek children. The analyzed SNPs were further associated with fatty acids and Δ desaturases, variables that have previously been shown to correlate with obesity markers. Some of these fatty acids may also modulate the observed genetic effect on BMI but not insulin resistance.
References
Allison DB, Kaprio J, Korkeila M, Koskenvuo M, Neale MC, Hayakawa K . The heritability of body mass index among an international sample of monozygotic twins reared apart. Int J Obes Relat Metab Disord 1996; 20: 501–506.
Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU et al. Association analyses of 249 796 individuals reveal 18 new loci associated with body mass index. Nat Genet 2010; 42: 937–948.
Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet 2009; 41: 18–24.
Willer CJ, Speliotes EK, Loos RJ, Li S, Lindgren CM, Heid IM et al. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat Genet 2009; 41: 25–34.
Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 2007; 316: 889–894.
Dina C, Meyre D, Gallina S, Durand E, Körner A, Jacobson P et al. Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet 2007; 39: 724–726.
Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet 2007; 3: e115.
Johansson A, Marroni F, Hayward C, Franklin CS, Kirichenko AV, Jonasson I et al. Linkage and genome-wide association analysis of obesity-related phenotypes: association of weight with the MGAT1 gene. Obesity (Silver Spring) 2010; 18: 803–808.
Kumar R, Yang J, Larsen RD, Stanley P . Cloning and expression of N-acetylglucosaminyltransferase I, the medial golgi transferase that initiates complex N-linked carbohydrate formation. Proc Natl Acad Sci USA 1990; 87: 9948–9952.
Pownall S, Kozak CA, Schappert K, Sarkar M, Hull E, Schachter H et al. Molecular cloning and characterization of the mouse UDP-N-acetylglucosamine:alpha-3-D-mannoside beta-1,2-N-acetylglucosaminyltransferase I gene. Genomics 1992; 12: 699–704.
Yip B, Chen SH, Mulder H, Höppener JW, Schachter H . Organization of the human beta-1,2-N-acetylglucosaminyltransferase I gene (MGAT1), which controls complex and hybrid N-glycan synthesis. Biochem J 1997; 321 (Part 2): 465–474.
Schachter H . Biosynthetic controls that determine the branching and microheterogeneity of protein-bound oligosaccharides. Biochem Cell Biol 1986; 64: 163–181.
Schachter H . The ‘yellow brick road’ to branched complex N-glycans. Glycobiology 1991; 1: 453–461.
Schachter H . Mgat1-dependent N-glycans are essential for the normal development of both vertebrate and invertebrate metazoans. Semin Cell Dev Biol 2010; 21: 609–615.
Lowe JB, Marth JD . A genetic approach to Mammalian glycan function. Annu Rev Biochem 2003; 72: 643–691.
Ioffe E, Stanley P . Mice lacking N-acetylglucosaminyltransferase I activity die at mid-gestation, revealing an essential role for complex or hybrid N-linked carbohydrates. Proc Natl Acad Sci USA 1994; 91: 728–732.
Metzler M, Gertz A, Sarkar M, Schachter H, Schrader JW, Marth JD . Complex asparagine-linked oligosaccharides are required for morphogenic events during post-implantation development. EMBO J 1994; 13: 2056–2065.
Schachter H . The role of the GlcNAc(beta)1,2Man(alpha)- moiety in mammalian development. Null mutations of the genes encoding UDP-N-acetylglucosamine:alpha-3-D-mannoside beta-1,2-N-acetylglucosaminyltransferase I and UDP-N-acetylglucosamine:alpha-D-mannoside beta-1,2-N-acetylglucosaminyltransferase I.2 cause embryonic lethality and congenital muscular dystrophy in mice and men, respectively. Biochim Biophys Acta 2002; 1573: 292–300.
Jaeken J, Carchon H, Stibler H . The carbohydrate-deficient glycoprotein syndromes: pre-golgi and golgi disorders? Glycobiology 1993; 3: 423–428.
Charuk JH, Tan J, Bernardini M, Haddad S, Reithmeier RA, Jaeken J et al. Carbohydrate-deficient glycoprotein syndrome type II An autosomal recessive N-acetylglucosaminyltransferase II. deficiency different from typical hereditary erythroblastic multinuclearity, with a positive acidified-serum lysis test (HEMPAS). Eur J Biochem 1995; 230: 797–805.
Granovsky M, Fata J, Pawling J, Muller WJ, Khokha R, Dennis JW . Suppression of tumor growth and metastasis in Mgat5-deficient mice. Nat Med 2000; 6: 306–312.
Hedstrand H . A study of middle-aged men with particular reference to risk factors for cardiovascular disease. Ups J Med Sci Suppl 1975; 19: 1–61.
Ingelsson E, Arnlöv J, Sundström J, Zethelius B, Vessby B, Lind L . Novel metabolic risk factors for heart failure. J Am Coll Cardiol 2005; 46: 2054–2060.
Zethelius B, Berglund L, Hänni A, Berne C . The interaction between impaired acute insulin response and insulin resistance predict type 2 diabetes and impairment of fasting glucose: report from a 20-year follow-up in the Uppsala longitudinal study of adult men - ULSAM. Ups J Med Sci 2008; 113: 117–130.
Jacobsson JA, Danielsson P, Svensson V, Klovins J, Gyllensten U, Marcus C et al. Major gender difference in association of FTO gene variant among severely obese children with obesity and obesity related phenotypes. Biochem Biophys Res Commun 2008; 368: 476–482.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Bergman RN . Minimal model: perspective from 2005. Horm Res 2005; 64 (Suppl 3): 8–15.
Kamel A, Norgren S, Elimam A, Danielsson P, Marcus C . Effects of growth hormone treatment in obese prepubertal boys. J Clin Endocrinol Metab 2000; 85: 1412–1419.
Fan JB, Oliphant A, Shen R, Kermani BG, Garcia F, Gunderson KL et al. Highly parallel SNP genotyping. Cold Spring Harb Symp Quant Biol 2003; 68: 69–78.
Barrett JC, Fry B, Maller J, Daly MJ . Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 2005; 21: 263–265.
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B et al. The structure of haplotype blocks in the human genome. Science 2002; 296: 2225–2229.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007; 81: 559–575.
Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG . Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol 2006; 6: 50.
Benjamini Y, Hochberg Y . Controlling the False Discovery Rate - a Practical and Powerful Approach to Multiple Testing. J R Stat Soc Series B Stat Methodol 1995; 57: 289–300.
Skol AD, Scott LJ, Abecasis GR, Boehnke M . Joint analysis is more efficient than replication-based analysis for two-stage genome-wide association studies. Nat Genet 2006; 38: 209–213.
Warensjo E, Ohrvall M, Vessby B . Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutr Metab Cardiovasc Dis 2006; 16: 128–136.
Riserus U . Fatty acids and insulin sensitivity. Curr Opin Clin Nutr Metab Care 2008; 11: 100–105.
Koenderman AH, Koppen PL, Koeleman CA, van den Eijnden DH . N-acetylglucosaminyltransferase III IV and V activities in Novikoff ascites tumour cells, mouse lymphoma cells and hen oviduct. Application of a sensitive and specific assay by use of high-performance liquid chromatography. Eur J Biochem 1989; 181: 651–655.
Vessby B . Dietary fat and insulin action in humans. Br J Nutr 2000; 83 (Suppl 1): S91–S96.
Warensjo E, Ingelsson E, Lundmark P, Lannfelt L, Syvänen AC, Vessby B et al. Polymorphisms in the SCD1 gene: associations with body fat distribution and insulin sensitivity. Obesity (Silver Spring) 2007; 15: 1732–1740.
Okada T, Furuhashi N, Kuromori Y, Miyashita M, Iwata F, Harada K . Plasma palmitoleic acid content and obesity in children. Am J Clin Nutr 2005; 82: 747–750.
Acknowledgements
The study was supported by the Swedish Research Council, Novo Nordisk, Tore Nilsons foundation and Åhlens foundation. RF was supported by the Göran Gustafsson foundation. The SNP genotyping was performed by the SNP Technology Platform, Uppsala, Sweden (http://www.genotyping.se) with support from Uppsala University and the Knut and Alice Wallenberg foundation and at the Uppsala Genome Centre. We thank the Healthy Growth Study Group for their contribution in this study. The Healthy Growth Study Group consists of (1) Harokopio University Research Team/ Department of Nutrition and Dietetics: Yannis Manios (Coordinator), George Moschonis (Project manager), Katerina P Skenderi, Evangelia Grammatikaki, Odysseas Androutsos, Sofia Tanagra, Alexandra Koumpitski, Paraskevi-Eirini Siatitsa, Anastasia Vandorou, Aikaterini-Efstathia Kyriakou, Vasiliki Dede, Maria Kantilafti, Aliki-Eleni Farmaki, Aikaterini Siopi, Sofia Micheli, Louiza Damianidi, Panagiota Margiola, Despoina Gakni, Vasiliki Iatridi, Christina Mavrogianni, Kelaidi Michailidou, Aggeliki Giannopoulou, Efstathoula Argyri, Konstantina Maragkopoulou, Maria Spyridonos, Eirini Tsikalaki, Panagiotis Kliasios, Anthi Naoumi, Konstantinos Koutsikas, Katerina Kondaki, Epistimi Aggelou, Zoi Krommyda, Charitini Aga, Manolis Birbilis, Ioanna Kosteria, Amalia Zlatintsi, Elpida Voutsadaki, Eleni-Zouboulia Papadopoulou, Zoi Papazi, Maria Papadogiorgakaki, Fanouria Chlouveraki, Maria Lyberi, Nora Karatsikaki-Vlami, Eva Dionysopoulou and Efstratia Daskalou (2) Aristotle University of Thessaloniki/ School of Physical Education and Sports Sciences: Vassilis Mougios, Anatoli Petridou, Konstantinos Papaioannou, Georgios Tsalis, Ananis Karagkiozidis, Konstantinos Bougioukas, Afroditi Sakellaropoulou and Georgia Skouli. (3) University of Athens/ Medical School: George P Chrousos, Maria Drakopoulou and Evangelia Charmandari. Uppsala University/ Department of Neuroscience, Functional Pharmacology: Helgi B Schiöth, Robert Fredriksson, Markus Sällman-Almén and Josefin Jacobsson.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Jacobsson, J., Rask-Andersen, M., Risérus, U. et al. Genetic variants near the MGAT1 gene are associated with body weight, BMI and fatty acid metabolism among adults and children. Int J Obes 36, 119–129 (2012). https://doi.org/10.1038/ijo.2011.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.11
Keywords
This article is cited by
-
Genome-wide association studies in Samoans give insight into the genetic architecture of fasting serum lipid levels
Journal of Human Genetics (2021)
-
Genome-wide association analyses suggest NELL1 influences adverse metabolic response to HCTZ in African Americans
The Pharmacogenomics Journal (2014)
-
Structural and Compositional Changes in Erythrocyte Membrane of Obese Compared to Normal-Weight Adolescents
The Journal of Membrane Biology (2013)
-
Association of TMEM18 variants with BMI and waist circumference in children and correlation of mRNA expression in the PFC with body weight in rats
European Journal of Human Genetics (2012)