Abstract
Objective:
To investigate the relationship between the metabolic syndrome and intraocular pressure (IOP).
Methods:
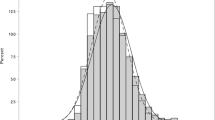
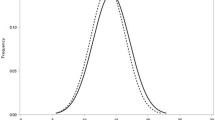
An observational study was conducted in a medical health checkup program at a general hospital. This study involved 14 003 apparently healthy Japanese men and women, 18–83 years of age, with a mean IOP of 14.8 (3.0) mm Hg. IOP was examined by noncontact tonometer. High-ocular tension was defined as IOP >21 mm Hg without optic-disc abnormalities or history of receiving any anti-glaucoma therapy. Modified criteria of the revised National Cholesterol Education Program Adult Treatment Panel III (rATPIII), the new International Diabetes Federation definition, and the Japan Society for The Study of Obesity definition were used to characterize the metabolic syndrome. Air temperature was assessed from the Gifu Meteorological Observatory, Gifu, Japan.
Results:
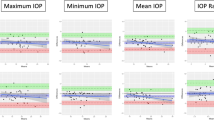
In the male and female subjects, mean IOP and the prevalence of high-ocular tension became high in direct correlation with the increased number of metabolic syndrome components. To analyze by logistic regression, the metabolic syndrome defined by rATPIII was positively and maximum temperature was negatively correlated with high-ocular tension in males (adjusted odds ratio: 2.0 [95% confidence interval, CI, 1.43–2.78] and 0.63 [95% CI, 0.54–0.73], respectively) and in females (adjusted odds ratio: 7.09 [95% CI, 3.74–13.43] and 0.67 [95% CI, 0.53–0.87], respectively). Three of five metabolic syndrome components (fasting plasma glucose, blood pressure, and triglycerides) were related to high-ocular tension.
Conclusion:
The metabolic syndrome is a risk factor for high-ocular tension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Reaven GM . Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
Ford ES, Giles WH, Dietz WH . Prevalence of the metabolic syndrome among US adults: findings from the third national health and nutrition examination survey. JAMA 2002; 287: 356–359.
Oda E, Abe M, Veeraveedu PT, Watanabe K . Considerable disagreement among definitions of metabolic syndrome for Japanese. Circ J 2007; 71: 1239–1243.
Dandona P, Aljada A, Mohanty P . The anti-inflammatory and potential anti-atherogenic effect of insulin: a new paradigm. Diabetologia 2002; 45: 924–930.
Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R . Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation 2005; 111: 1448–1454.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The baltimore eye survey. Arch Ophthalmol 1991; 109: 1090–1095.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713 discussion 829-730.
Oh SW, Lee S, Park C, Kim DJ . Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabetes Metab Res Rev 2005; 21: 434–440.
Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation 2005; 112: 2735–2752.
Alberti KG, Zimmet P, Shaw J . Metabolic syndrome—a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med 2006; 23: 469–480.
Definition and the diagnostic standard for metabolic syndrome—committee to evaluate diagnostic standards for metabolic syndrome. Nippon Naika Gakkai Zasshi 2005; 94: 794–809.
Stone NJ, Bilek S, Rosenbaum S . Recent national cholesterol education program adult treatment panel III update: adjustments and options. Am J Cardiol 2005; 96: 53E–59E.
Matuzawa Y . Metabolic syndrome-definition and diagnostic criteria in Japan. J Jpn Soc Int Med 2005; 94: 188–203.
World Health Organization Western Pacific Region/International Association for the Study of Obesity/International Obesity Task Force . The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia 2000. Melbourne (Australia).
Quigley HA, Langham ME . Comparative intraocular pressure measurements with the pneumatonograph and Goldmann tonometer. Am J Ophthalmol 1975; 80: 266–273.
Klein BE, Klein R, Linton KL . Intraocular pressure in an American community. The beaver dam eye study. Invest Ophthalmol Vis Sci 1992; 33: 2224–2228.
Hennis A, Wu SY, Nemesure B, Leske MC . Hypertension, diabetes, and longitudinal changes in intraocular pressure. Ophthalmology 2003; 110: 908–914.
Uhm KB, Shin DH . Glaucoma risk factors in primary open-angle glaucoma patients compared to ocular hypertensives and control subjects. Korean J Ophthalmol 1992; 6: 91–99.
Armaly MF, Baloglou PJ . Diabetes mellitus and the eye. 11. Intraocular pressure and aqueous outflow facility. Arch Ophthalmol 1967; 77: 493–502.
Bulpitt CJ, Hodes C, Everitt MG . Intraocular pressure and systemic blood pressure in the elderly. Br J Ophthalmol 1975; 59: 717–720.
Mori K, Ando F, Nomura H, Sato Y, Shimokata H . Relationship between intraocular pressure and obesity in Japan. Int J Epidemiol 2000; 29: 661–666.
Shiose Y, Kawase Y . A new approach to stratified normal intraocular pressure in a general population. Am J Ophthalmol 1986; 101: 714–721.
Sechi LA, Bartoli E . Molecular mechanisms of insulin resistance in arterial hypertension. Blood Press 1996; 5 (Suppl 1): 47–54.
Su DH, Wong TY, Wong WL, Saw SM, Tan DT, Shen SY et al. Diabetes, hyperglycemia, and central corneal thickness: the Singapore Malay Eye Study. Ophthalmology 2008; 115: 964–968 e961.
Su DH, Wong TY, Foster PJ, Tay WT, Saw SM, Aung T . Central corneal thickness and its associations with ocular and systemic factors: the Singapore Malay Eye Study. Am J Ophthalmol 2009; 147: 709–716 e701.
Murase H, Sawada A, Mochizuki K, Yamamoto T . Effects of corneal thickness on intraocular pressure measured with three different tonometers. Jpn J Ophthalmol 2009; 53: 1–6.
Blumenthal M, Blumenthal R, Peritz E, Best M . Seasonal variation in intraocular pressure. Am J Ophthalmol 1970; 69: 608–610.
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology 2004; 111: 1641–1648.
Nemesure B, Honkanen R, Hennis A, Wu SY, Leske MC . Incident open-angle glaucoma and intraocular pressure. Ophthalmology 2007; 114: 1810–1815.
Acknowledgements
WE thank John Bush for his excellent assistance in preparing the manuscript. This study was supported by a grant from the Gifu Medical Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Imai, K., Hamaguchi, M., Mori, K. et al. Metabolic syndrome as a risk factor for high-ocular tension. Int J Obes 34, 1209–1217 (2010). https://doi.org/10.1038/ijo.2010.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.32
Keywords
This article is cited by
-
Relationship between blood pressure and intraocular pressure in the JPHC-NEXT eye study
Scientific Reports (2022)
-
The association between intraocular pressure and different combination of metabolic syndrome components
BMC Ophthalmology (2016)