Abstract
Reversible posterior leukoencephalopathy syndrome (RPLS) is a critical maternal complication in some pre-eclampsia (PE) and nearly all eclampsia patients; RPLS is associated with high blood pressure (BP). However, the effect of BP on RPLS and the different characteristics of RPLS in PE or eclampsia are largely unknown. We consecutively collected data from 69 patients who were diagnosed with RPLS in PE or eclampsia between 2013 and 2017. The BP and biochemical indicators at onset and post onset of RPLS were examined to explore their likely correlation with RPLS. We grouped patients into PE (n=40) and eclampsia (n=29) groups according to whether a seizure had occurred. Information regarding BP, clinical symptoms and imaging features was collected retrospectively to explore the differences between groups. BP measurements (moderate and severe hypertension, systolic pressure (SBP), diastolic pressure (DBP) and mean arterial pressure (MAP) levels) and biochemical indicators (uric acid, lactate dehydrogenase (LDH), C-reactive protein and WBC) were higher at the onset of RPLS than post-onset of RPLS (P<0.001), whereas normal BP and serum albumin levels were lower (P<0.001). Moreover, the BP values (SBP, DBP and MAP) and LDH levels were significantly correlated with the degree of edema (Spearman’s correlation, P<0.01). These results suggest that hypertension and LDH are likely factors in the development of RPLS in PE or eclampsia. Moreover, BP and LDH were closely related to the degree of brain edema, However, no significant differences were found between the PE and eclampsia groups with the exception of age and consciousness impairment.
Similar content being viewed by others
Introduction
Reversible posterior leukoencephalopathy syndrome (RPLS) is a clinical-imaging syndrome that was first described by Hinchey et al.1 in 1996 and consists of symptoms such as headaches, visual changes, seizures, consciousness impairment, mental disorders and focal neurologic deficits. RPLS is a critical maternal complication in some pre-eclampsia (PE) patients and nearly all eclampsia patients.2 However, the different characteristics of RPLS in PE or eclampsia are largely unknown, and the mechanism of RPLS is not completely understood. However, the same pathogenic mechanisms are shared;3 vasogenic edema is caused by a breakdown of cerebral autoregulation or cerebral vasoconstriction, disruption of the blood–brain barrier or endothelial dysfunction.1, 4 Cerebral perfusion, cerebral vasoconstriction and endothelial dysfunction have been proposed as possible mechanisms of RPLS.1, 2, 3, 4, 5
The pathophysiology of RPLS has not been elucidated. Among many factors, blood pressure (BP) plays an important role in the pathogenesis of RPLS.5 However, the effect and likely mechanism of BP on RPLS in PE or eclampsia are unclear. Endothelial cells are an important tissue within the wall between the blood stream and blood vessels.6 These cells release agents that regulate vasomotor function, trigger inflammatory processes and respond to physical and chemical signals.6, 7 Endothelial dysfunction could promote vascular inflammation, and vice versa. Endothelial dysfunction is paralleled by vascular inflammation and can be assessed by the soluble forms of intercellular adhesion molecule 1, vascular cell adhesion molecule-1, E-selectin, oxidized LDL receptor-1, C-reactive protein (CRP) and asymmetric dimethylarginine.6, 7, 8, 9 In addition, the serum lactate dehydrogenase (LDH) level represents an index for assessing endothelial dysfunction.10 To the best of our knowledge, the degree of brain edema is associated with LDH, renal function and albumin (ALB).10 In this study, we explored the likely factors in the development of RPLS in PE or eclampsia by comparing BP and biochemical indicators at the onset and post onset of RPLS and explored the effects of BP and laboratory parameters on RPLS by evaluating the correlation among BP, biochemical indicators and the degree of brain edema. Furthermore, we explored the characteristics of RPLS in PE or eclampsia by comparing the differences between the PE and eclampsia groups.
Materials and methods
This retrospective study was approved by the institutional ethics committee of The Third Affiliated Hospital of Guangzhou Medical University. A total of 69 women met the following inclusion criteria for the study: (a) patients diagnosed with PE or eclampsia after 20 weeks of gestation or within 6 weeks postpartum and (b) patients who underwent a magnetic resonance imaging (MRI) examination performed by a clinician after providing informed consent and who were diagnosed with RPLS in Guangzhou Medical Center for Critical Pregnant Women from January 2013 to January 2017. General information, BP, biochemical indicators, clinical symptoms and imaging features were retrospectively collected.
PE was defined as complications with hypertension, proteinuria, and edema between the 20th week of gestation and the 6th postpartum week. Eclampsia was defined as PE plus seizures unrelated to other cerebral conditions.11, 12
All 69 patients were examined using whole-brain MRI (Achieva 3.0 T, Philips, Amsterdam, The Netherlands), including T1-weighted, T2-weighted and T2 fluid-attenuated inversion recovery (FLAIR). The imaging features were described according to their location, including frontal, parietal, occipital, temporal, cerebellum, basal ganglia, brain stem, deep white matter and callosum; 1 point was recorded for each location involved. The extent and severity of vasogenic edema in the lesion area were graded using a scale of 0–5 with FLAIR images as follows:13 0, normal; 1, limited cortex or subcortical white matter edema; 2, white matter edema>cortex edema, white matter edema extends into deep white matter; 3, white matter edema>cortex edema, edema extends to the ventricular surface; 4, involved regions substantially extend to the ventricular surface and are nearly completely confluent; and 5, involved regions are fully confluent and continuous, with ventricular deformity due to the edema. The diagnosis and confirmation were made independently using MRI by two neuroradiologists. The neuroradiologists worked to reach a consensus.
In this study, RPLS was diagnosed based on a combination of clinical symptoms (headache, vision change, seizure, consciousness disorders or hypertension) and the standard radiological criteria (hyperintensities of T2WI and FLAIR in the subcortex and gyrus as evidence of focal vasogenic edema). A regular prenatal examination indicated that the examination times were consistent in terms of the time interval (gestation <28 weeks, 4-week intervals; 28–36 weeks of gestation, 2-week intervals; 36–40 weeks of gestation, 1-week intervals; and gestation >40 weeks, 3-day intervals). An irregular prenatal examination indicated that less than 2/3 of the recommended prenatal examinations were performed.
BP was obtained immediately at the onset of symptoms for the PE group and immediately at the onset of seizure for the eclampsia group. We measured BP again at the sixth postpartum week as the post-onset BP, and the measurements were classified into four categories according to the systolic pressure as follows: normal (<140 mm Hg), mildly elevated (140–159 mm Hg), moderately elevated (160–179 mm Hg), and severely elevated (⩾180 mm Hg). The mean arterial pressure (MAP) was defined as 2/3 of the diastolic pressure (DBP)+1/3 of the systolic pressure (SBP).
The biochemical indicators included serum ALB, serum Crea, urea (UA), blood urea nitrogen (BUN), LDH, CRP and WBC. We collected the biochemical indicators when the disease was most serious as a biochemical index at the time of disease onset, and we recorded the last biochemical indicators during hospitalization as the post-onset laboratory indexes.
Statistical analyses
Descriptive statistics for continuous variables are presented as the mean±s.d. values, and the categorical variables are presented as frequencies and percentages. We used Student’s t-test (normally distributed variables) or the Z test (not normally distributed variables) to examine both groups of patients for continuous variables, and we used the χ2-test or Fisher’s exact test to evaluate patients for the categorized variables. The threshold for significance was set at P<0.05. We analyzed our data using the SPSS 13.0 statistical software package (SPSS, Chicago, IL, USA).
Results
A total of 69 patients met the inclusion criteria. Of these patients, 38 (55.07%) were primiparous patients, 26 (37.68%) did not receive regular prenatal examinations, 4 (5.80%) gravidas had a history of hypertension during pregnancy, 6 (8.70%) had gestational diabetes and 18 (26.09%) had pregnancies that were complicated by HELLP syndrome. The mean age was 29.46±5.31 years, mean body mass index (BMI) was 21.93±2.44 kg m−2 and mean gestational length was 31.38±3.90 weeks.
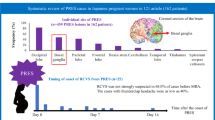
The clinical symptoms and lesion locations are presented in Table 1. Headache was the most common symptom in RPLS patients (53.62%), followed by seizure (42.03%). The occurrence rates of visual changes (33.33%) and consciousness impairment (30.43%) were similar. Dizziness (31.88%) was a common symptom in RPLS patients. The imaging features were notable in RPLS patients (Figure 1). In our study, the occipital lobe was the most frequently affected area (91.30%), followed by the parietal lobe (60.87%), frontal lobe (28.99%), basal ganglia and temporal lobe (both 24.64%); the brainstem, cerebellum, deep white matter and callosum were equally affected (5.88%) (Table 1).
(a) Axial T1W MRI showing low signal predominantly in the parietal lobes; (b) axial T2WI showing hyperintensive signal; (d) Axial DWI showing isointensive signal; (e) Axial ADC showing hyperintensive signal, indicating that the lesion was vascular edema; and (c) and (f) Axial FLAIR MRI showing hyperintensive signal (arrows).
The BP values changed significantly at the onset and post-onset of RPLS. The proportions of patients with moderately elevated pressure and severely elevated pressure at the onset of RPLS were increased markedly compared with the proportions of patients at the post onset of RPLS (P<0.001). Furthermore, SBP, DBP and MAP were increased significantly compared with the post onset of RPLS (P<0.001, Table 2). However, no significant differences were noted in patients with mildly elevated blood pressure, and the proportion of patients with normal BP after RPLS was higher than that at the onset of RPLS (P<0.001).
The biochemical indicators also changed significantly at the onset and post onset of RPLS. The ALB levels at the onset of RPLS were lower than those at the post onset of RPLS (P<0.001), whereas the levels of UA, LDH, CRP and WBC were higher at the onset of RPLS than at the post onset of RPLS (P<0.001) (Table 3). By contrast, the Crea and BUN levels did not significantly differ at the onset and post onset of RPLS.
In all patients, the involved areas scored 2.46±1.09 points, and the degree of edema in the involved areas scored 2.52±0.98 points. The BP values, including the SBP, DBP and MAP, were significantly correlated with the degree of edema (Spearman’s correlation, P<0.05). Furthermore, the LDH level was significantly correlated with the degree of edema (Spearman’s correlation, r=0.4639, P<0.0001) (Figure 2). However, no relationship was observed between the other biochemical indicators and degree of edema. The relationship among the biochemical indicators, BP and involved area points was not closely related.
Relationship between BP, LDH and the degree of brain edema. (a) SBP was significantly correlated with the degree of edema (Spearman’s correlation, r=0.4922, P<0.0001); (b) DBP was significantly correlated with the degree of edema (Spearman’s correlation, r=0.3311, P=0.0054); (c) MAP was significantly correlated with the degree of edema (Spearman’s correlation, r=0.4621, P<0.0001); and (d) LDH was significantly correlated with the degree of edema (Spearman’s correlation, r=0.4639, P<0.0001).
All patients were divided into either the PE group (n=40) or eclampsia group (n=29) according to whether seizures occurred. The general patient information and BP values are presented in Table 4. In the PE group, 29 (72.50%) were primiparous patients and 25 (62.50%) did not receive regular prenatal examinations; the mean age was 32.28±5.51 years; mean gestational length was 30.74±4.66 weeks; and BMI was 21.65±3.35 kg m−2. In the eclampsia group, 25 (86.21%) were primiparous patients and 18 (62.07%) did not receive regular prenatal examinations; the mean age was 25.59±6.54 years; mean gestational length was 32.27±5.06 weeks; and mean BMI was 22.31±2.69 kg m−2. Only age and consciousness impairment significantly differed between the groups (P<0.001). No significant differences were noted in terms of BP, involved area points, degree of edema (Table 4), clinical symptoms and involved locations (Table 1).
Discussion
RPLS is a clinicoradiological syndrome that was first described by Hinchey et al.1 in 1996. RPLS features a combination of symptoms, including headaches, visual changes, seizures, consciousness impairment, mental disorders and focal neurologic deficits. The incidence of RPLS is unclear. In our previous study, we reported that the incidence of RPLS in PE or eclampsia was 0.22%,2 which is higher than that reported in the literature (0.01%).14 As a regional Medical Center for Critical Pregnant Women, the high incidence rate is understandable. RPLS is a critical maternal complication in some PE patients and nearly all eclampsia patients that could endanger maternal and neonatal lives;2 therefore, we focused on RPLS in PE or eclampsia.
The onset of RPLS typically occurs acutely or sub-acutely. Various clinical symptoms are observed and lack specificity, including common symptoms, such as headaches, visual changes, seizures, consciousness impairment, mental disorders, focal neurologic deficits, nausea and vomiting, and rare symptoms, such as tinnitus and vertigo.15, 16, 17 Headache is the most common symptom in RPLS in PE or eclampsia according to several studies.18, 19, 20 In addition, symptoms of visual changes (33%), seizures (73%), consciousness impairment (57%) and vomiting (47%) occur frequently,20 whereas another study indicated that seizure is the most frequent symptom in RPLS patients with PE/eclampsia.21 In our study, the incidence of headache (53.62%), visual changes (33.33%), seizures (42.03%), consciousness impairment (30.43%) and dizziness (31.88%) were similar to the outcomes reported in the literature.17, 18, 19, 20, 21 Imaging is critical for the diagnosis and evaluation of RPLS, and MRI is the gold standard for the diagnosis of RPLS.22 Typically, T1W MRI exhibited low signals, whereas T2WI and FLAIR exhibited high signals. In addition, the DWI sequence exhibited a slightly lower signal, whereas the apparent diffusion coefficient (ADC) maps exhibited a higher signal, indicating that the lesion (subcortical white matter, especially in the occipital and parietal lobes) was vascular edema2 (Figure 1). A recent study indicated that the most frequently affected area in RPLS patients with PE/eclampsia is the occipital lobe (94–98.7%), followed by the frontal lobe (77–78.9%), temporal lobe (64–68%) and cerebellum (53%).23 In our study, the location of RPLS was generally consistent with the results reported in the literature. In addition, there were no significant differences between the PE and eclampsia groups in terms of the involved areas or degree of brain edema (P>0.05). Likely explanations include the involved areas and degree of brain edema, which were counted independently rather than combined in the groups to assess the severity of RPLS.
RPLS exhibits various pathogenies, such as hypertension, PE or eclampsia, transplantation, renal dysfunction, autoimmunity, sepsis and chemotherapy.5, 23, 24 The pathological and physiological changes in RPLS might result from numerous factors attributed to various mechanisms. Although the pathophysiology is unclear, the likely pathogenic mechanisms are shared,4 including vasogenic edema caused by the breakdown of cerebral autoregulation or cerebral vasoconstriction, disruption of the blood–brain barrier or endothelial dysfunction.
The relationship between BP and RPLS has not been elucidated. However, RPLS might be associated with high BP because RPLS could be a consequence of a hypertensive crisis. The supporting theory is that severe hypertension is associated with failed autoregulation, leading to vasogenic edema caused by vasodilatation, breakthrough of the blood–brain barrier, hyperperfusion and increased vascular permeability.25 In our study, the BP condition was classified as normal BP, moderately elevated BP or severely elevated BP. SBP, DBP and MAP were increased considerably at the onset of RPLS compared with the post-onset of RPLS (P<0.001), except in the case of mildly elevated BP. Furthermore, the BP conditions, including SBP, DBP and MAP, at the onset of RPLS were significantly correlated with the degree of edema. These results suggest that BP is an important factor for RPLS. However, 15–20% of RPLS patients exhibited normal or mildly elevated BP, suggesting that hypertension is not essential for brain edema. An earlier study indicated that BP fluctuations and RPLS are not closely correlated.26 Therefore, high BP alone might not be sufficient to cause RPLS, and other factors might play a similar role.
Endothelial dysfunction might also play an important role. The supporting theory indicates that endothelial dysfunction is caused by cytotoxicity that induces cytokine release or direct injury of the endothelial cells, leading to vasoconstriction and edema, with subsequent hypoperfusion.27 Endothelial cells are an important tissue within the wall between the blood stream and blood vessels.6 Endothelial dysfunction is closely related to the severity of inflammation; therefore, we assessed endothelial dysfunction based on biochemical indicators (LDH, CRP and WBC).6, 7, 8, 9, 10 In our study, the LDH, CRP and WBC levels were higher at the onset of RPLS than post onset of RPLS (P<0.001). Furthermore, we examined the relationship between the LDH, CRP and WBC levels at the onset of RPLS and degree of edema; only the LDH level was significantly correlated with the degree of edema. These results suggest that LDH could reflect the severity of inflammation and degree of brain edema, especially in PE or eclampsia during pregnancy.28 To the best of our knowledge, the degree of brain edema is also associated with renal function and ALB.12 ALB is one of the most important plasma antioxidants associated with endothelial function,28 and renal failure is an important factor in the development of RPLS12 that can be evaluated using biochemical indicators (Crea, BUN and UA). Although the ALB and UA significantly differed at the onset of RPLS compared with the post onset of RPLS, Crea and BUN showed no significant differences. These biochemical indicators did not correlate with the degree of brain edema. The relationship between those biochemical indicators and the degree of edema warrants additional studies.
In our study, we retrospectively compared information regarding the BP, clinical symptoms and imaging features between the PE and eclampsia patients and found that there were no significant differences except for age and consciousness impairment. Patients in the PE group were older than those in the eclampsia group (P<0.001); likely explanations for this difference might be that older pregnant women started giving birth because of the national Two-child policy, thus leading to more critical pregnant women. The incidence of consciousness impairment in the eclampsia group was higher than that in the PE group, and a possible explanation for this difference is that the condition of the patients in the eclampsia group was likely more serious.
Several limitations in this study should be acknowledged. First, this was a retrospective study; therefore, the results depend on patients’ medical records and are subject to their availability and accuracy. Second, the last biochemical indicators during hospitalization were collected as post-onset laboratory indexes and might not have represented the baseline level. Third, a follow-up MRI was not performed on some RPLS patients; therefore, imaging features were not evaluated again. In addition, DWI sequences, ADC maps and MRA information were not available for all patients, the type of brain edema was not clearly distinguished, and the cerebral vasoconstriction was not explored. Although we explored the likely factors associated with the development of RPLS in our study, additional prospective studies are still required.
In summary, hypertension and LDH are likely factors in the development of RPLS in PE or eclampsia. In addition, BP and LDH were found to be closely related to the degree of brain edema. However, no significant differences were found between the PE and eclampsia groups with the exception of age and consciousness impairment.
References
Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR . A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996; 334: 494–500.
Fang X, Liang Y, Chen D, He F, Chen J, Huang F . A study on clinicoradiological characteristics and pregnancy outcomes of reversible posterior leukoencephalopathy syndrome in preeclampsia or eclampsia. Hypertens Res (e-pub ahead of print 7 September 2017; doi:10.1038/hr.2017.76.
Hobson EV, Craven I, Blank SC . Posterior reversible encephalopathy syndrome: a truly treatable neurologic illness. Perit Dial Int 2012; 32: 590–594.
Mukherjee P, Mckinstry RC . Reversible posterior leukoencephalopathy syndrome: evaluation with diffusion-tensor MR imaging. Radiology 2001; 219: 756–765.
Fugate JE, Rabinstein AA . Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol 2015; 14: 914–925.
Endemann DH, Schiffrin EL . Endothelial dysfunction. J Am Soc Nephrol 2004; 15: 1983–1992.
Brandes RP . Endothelial dysfunction and hypertension. Hypertension 2014; 64: 924–928.
Landmesser U, Drexler H . The clinical significance of endothelial dysfunction. Curr Opin Cardiol 2005; 20: 547–551.
Liu L, Han X, Huang Q, Zhu X, Yang J, Liu H . Increased neuronal seizure activity correlates with excessive systemic inflammation in a rat model of severe preeclampsia. Hypertens Res 2016; 39: 701–708.
Gao B, Liu FL, Zhao B . Association of degree and type of edema in posterior reversible encephalopathy syndrome with serum lactate dehydrogenase level: Initial experience. Eur J Radiol 2012; 81: 2844–2847.
SMFM Publications Committee. SMFM Statement: benefit of antihypertensive therapy or mild-to-moderate chronic hypertension during pregnancy remains uncertain. Am J Obstet Gynecol 2015; 213: 3–4.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM . The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001; 20: 9–14.
Bartynski WS, Boardman JF, Zeigler ZR, Shadduck RK, Lister J . Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol 2006; 27: 2179–2190.
Daniel S, Thampi B, Viswanathan M, Manoj P . Posterior reversible leukoencephalopathy syndrome: a rare complication with gestational hypertension and pre eclampsia. J Int Med Res 2014; 2: 50–53.
Singh RR, Ozyilmaz N, Waller S, U-King-Im JM, Lim M, Siddiqui A, Sinha MD . A study on clinical and radiological features and outcome in patients with posterior reversible encephalopathy syndrome (PRES). Eur J Pediatr 2014; 173: 1225–1231.
Liman TG, Bohner G, Heuschmann PU, Endres M, Siebert E . The clinical and radiological spectrum of posterior reversible encephalopathy syndrome: the retrospective Berlin PRES study. J Neurol 2012; 259: 155–164.
Granata G, Greco A, Iannella G, Granata M, Manno A, Savastano E, Magliulo G . Posterior reversible encephalopathy syndrome—Insight into pathogenesis, clinical variants and treatment approaches. Autoimmun Rev 2015; 14: 830–836.
Marrone LC, Gadonski G, Diogo LP, Brunelli JP, Martins WA, Laguna Gde O, Bahlis LF, Filho JR, da Costa BE, Poli-de-Figueiredo CE, Marrone AC, da Costa JC . Posterior reversible encephalopathy syndrome: differences between pregnant and non-pregnant patients. Neurol Int 2014; 6: 5376–5388.
Kurdoglu Z, Cetin O, Sayın R, Dirik D, Kurdoglu M, Kolusarı A, Yıldızhan R, Guler Sahin H . Clinical and perinatal outcomes in eclamptic women with posterior reversible encephalopathy syndrome. Arch Gynecol Obstet 2015; 292: 1013–1018.
Wen Y, Yang B, Huang Q, Liu Y . Posterior reversible encephalopathy syndrome in pregnancy: a retrospective series of 36 patients from mainland China. Ir J Med Sci 2017, 1–7.
Roth C, Ferbert A . The posterior reversible encephalopathy syndrome: what's certain, what's new? Pract Neurol 2011; 11: 136–144.
Nielsen LH, Grøn BS, Ovesen PG . Posterior reversible encephalopathy syndrome postpartum. Clin Case Rep 2015; 3: 266–270.
Kutlesič MS, Kutlesič RM, Koratevič GP . Posterior reversible encephalopathy syndrome in eclamptic patients: Neuroradiological manifestation, pathogenesis and management. Med Pregl 2015; 68: 53–58.
Ohno Y, Terauchi M, Tamakoshi K, Shiozaki A, Saito S . The risk factors for labor onset hypertension. Hypertens Res 2016; 39: 260–265.
Bartynski WS . Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol 2008; 29: 1043–1049.
Rabinstein AA, Mandrekar J, Merrell R, Kozak OS, Durosaro O, Fugate JE . Blood pressure fluctuations in posterior reversible encephalopathy syndrome. J Stroke Cerebrovasc Dis 2012; 21: 254–258.
Marra A, Vargas M, Striano P, Del Guercio L, Buonanno P, Servillo G . Posterior reversible encephalopathy syndrome: the endothelial hypotheses. Med Hypotheses 2014; 82: 619–622.
Guler A, Ciftci S, Eraslan C, Celebisoy A, Sirin H . Evaluation of posterior reversible encephalopathy syndrome from different aspects: what is the role of serum LDH and albumin level in pathogenesis? Neurol Asia 2016; 21: 169–176.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (81371260, 81601313); National Key Clinical Department, National Key Discipline, Guangdong Provincial Key Laboratory for Diagnosis and Treatment of Major Neurological Diseases (2014B030301035); Social Development Planning Project of Science and Technology Department of Guangdong Province (2014A020212348); Key Laboratory for Major Obstetric Diseases of Guangdong Province; Natural Science Foundation of Guangdong Province (2017A030313850); Innovative Team for the Major Obstetric Disease Prevention and Control of Education Department of Guangdong Province (2015KCXTD020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiaobo, F., Yanling, L., Dunjin, C. et al. Effect of blood pressure on reversible posterior leukoencephalopathy syndrome in pre-eclampsia or eclampsia. Hypertens Res 41, 112–117 (2018). https://doi.org/10.1038/hr.2017.95
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.95
Keywords
This article is cited by
-
MRI characteristics of brain edema in preeclampsia/eclampsia patients with posterior reversible encephalopathy syndrome
BMC Pregnancy and Childbirth (2021)
-
Serum Neurofilament Light: a Potential Diagnostic and Prognostic Biomarker in Obstetric Posterior Reversible Encephalopathy Syndrome
Molecular Neurobiology (2021)
-
Targeting inflammation to reduce seizure severity in an experimental model of eclampsia
Hypertension Research (2020)
-
Anti-glomerular basement membrane disease complicated with posterior reversible encephalopathy syndrome and subcortical cerebral hemorrhage: a case report and review of the literature
CEN Case Reports (2020)