Abstract
This longitudinal cohort study investigated whether peripheral WBC counts could predict peripheral arterial disease (PAD) incidence after a 2.3-year follow-up in a Chinese community-based population without PAD at baseline. A total of 3555 Chinese subjects without fever and PAD at baseline from an atherosclerosis cohort were included in our analysis. The ankle brachial index (ABI) was measured, and PAD was defined as an ABI <0.9. Multivariate regression models were used to evaluate the association of WBC count and new-onset PAD. The mean (±s.d.) baseline WBC count was 6.11±1.54 × 109 l−1, the mean (±s.d.) ABI was 1.11±0.08 at baseline and the incidence of PAD was 2.7% over 2.3 years. WBC counts were significantly associated with PAD incidence (odds ratio (OR)=1.27, 95% confidence interval (CI): 1.14–1.41, P<0.0001) with every 1 × 109 l−1 increase in WBC count. This relationship remained significant (OR=1.21, 95% CI: 1.08–1.36, P=0.0014) even after adjusting for other variables. The highest WBC quartile group had increased risk when compared with the lowest quartile group (OR=2.14, 95% CI: 1.09–4.22, P=0.027) in a multivariate logistic model. Furthermore, we did not find significant heterogeneity among the analyzed subgroups based on sex (male or female), age (<60 or ⩾60 years old), body mass index (BMI, <25 or ⩾25 kg m−2), current smoking, current drinking, hypertension, diabetes mellitus, dyslipidemia or cardiovascular disease. In conclusion, elevated WBC counts independently predict the risk of new-onset PAD in a Chinese community-based population, supporting the hypothesis that systemic inflammation plays an important role in PAD development.
Similar content being viewed by others
Introduction
According to the Global Burden of Disease Study, although age-standardized mortality for cardiovascular and circulatory diseases has decreased by 22%, significant increases in mortality have occurred for peripheral arterial disease (PAD) from 1990 to 2013.1 PAD is a surrogate of systemic atherosclerosis, and patients with PAD have a significantly increased risk for premature mortality and cardiovascular events.2, 3, 4, 5 There is evidence that markers of inflammation including WBC count and C-reactive protein are associated with higher mortality in patients with known atherosclerotic vascular disease6, 7, 8 and also associated with increased risk of myocardial infarction and stroke,9, 10, 11, 12 which shows that atherogenesis is a chronic inflammatory process and inflammation potentially plays a central role in the development and progression of systemic atherosclerosis.13 Little attention has been paid to the association of inflammatory markers with new-onset PAD,14 especially in the Chinese population. Therefore, we performed this longitudinal cohort study to investigate whether peripheral WBC count could predict PAD incidence after a 2.3-year follow-up in a Chinese community-based population without PAD at baseline.
Methods
Study population
Participants were from an atherosclerosis cohort survey, including 9540 community residents, that was conducted between December 2011 and April 2012 in Beijing, China. Initially, the prespecified age range for cohort inclusion was ⩾40 years old at baseline. In 2014, 5962 of the participants with gene chip data were invited for a follow-up visit from May 2014 to July 2014. Among these 5962 patients, both WBC and ankle brachial index (ABI) data were available for 5662 participants. Finally, 3823 participants (64.1% of 5962) responded and came onsite, and both baseline WBC and ABI data were available for 3658 participants. Except for age, current smoking and the usage of hypoglycemic drugs, the nonresponders did not differ substantially from the responders regarding baseline characteristics; in particular, a significant difference was not observed in the two groups regarding WBC nor ABI (data not shown) that was described in detail in our previous study.15
Among these 3823 subjects, patients who had an ABI <0.9 at baseline or lacked either baseline ABI, follow-up ABI or baseline WBC count were excluded; we also excluded the subjects with an ABI >1.4 as higher values of ABI are attributed, in part, to medial artery calcification and are a marker of PAD. Before a venous blood sample was obtained during the study, patients with fever (>37.5 °C) were excluded. Furthermore, based on the questionnaire, we excluded patients with hematological diseases or tumors that may influence the WBC count. A total of 3555 Chinese subjects from this atherosclerosis cohort were included in our analysis. This study was approved by the ethics committee of Peking University First Hospital, and each participant provided written informed consent.
Data collection
Other variables
As described previously,15 baseline data were collected according to a standard operating procedure by trained research coordinators. A standardized questionnaire was used to assess basic information including social demographic status, education, occupation, diet, lifestyle, health behavior and medical history. Body mass index (BMI) was calculated as the weight (kg) divided by height (m) squared. After a 5 min rest, seated peripheral (brachial) blood pressure (BP) was obtained for each participant using an Omron (Kyoto, Japan) HEM-7117 electronic sphygmomanometer with the standard method of calibration and appropriately sized cuffs. Triplicate measurements on the right arm were taken with ⩾1 min between successive readings. Each patient’s systolic BP (SBP) and diastolic BP that were used in the analysis were calculated as the mean of three consecutive measurements.
After an overnight fast of at least 12 h, a venous blood sample was obtained from the forearm of each participant. Serum samples were used for the measurement of fasting blood glucose, the standard 75 g oral glucose tolerance test, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides and creatinine. All laboratory variables at baseline were measured on the Roche (Basel, Switzerland) C8000 Automatic Analyzer.
Current smoking was defined as smoking one cigarette or more per day for at least half a year. Current drinking was defined as drinking once per week for at least half a year. Hypertension was defined as any self-reported history of hypertension, SBP ⩾140 mm Hg, a diastolic BP ⩾90 mm Hg or usage of any antihypertensive drugs. Diabetes mellitus was defined as any self-reported history of diabetes, fasting blood glucose ⩾7.0 mmol l−1 and a 2 h plasma glucose value in oral glucose tolerance test ⩾11.1 mmol l−1 or usage of any hypoglycemic drugs. Dyslipidemia was defined as any self-reported history of dyslipidemia, triglyceride >1.7 mmol l−1 (150 mg dl−1), total cholesterol >5.18 mmol l−1 (200 mg dl−1), low-density lipoprotein cholesterol >3.3 mmol l−1 (130 mg dl−1), high-density lipoprotein cholesterol <1.0 mmol l−1 (40 mg dl−1) or usage of any lipid-lowering drugs. Cardiovascular disease (CVD) was defined as any self-reported history of coronary heart disease or stroke.
WBC counts
The WBCs (× 109 l−1) were measured in blood samples obtained by venipuncture after an overnight fast. The baseline WBC count was determined in a BC-3000 auto hematology analyzer (Mindray Medical International, Shenzhen, China) in the laboratory of the Peking University Shougang Hospital.
Ankle brachial index
The subject’s SBP was measured on two arms (brachial artery) and two ankles (posterior tibial arteries) simultaneously using a BP-203RPE III machine (Omron Healthcare) after the subject remained in a supine position for at least 5 min. The machine automatically calculated the ABI results, and the left and right ABI values were defined as ankle SBP for each side, respectively, by dividing by the highest brachial SBP. ABI was measured twice during the study: once at baseline and once at the follow-up in 2014. New-onset PAD was defined as at least one ABI value <0.9 at the follow-up survey in 2014.
Statistical analysis
Continuous variables were reported as the mean±s.d., and categorical variables were reported as percentages (%) for all participants. Normally distributed continuous variables were compared using one-way analysis of variance. Logistic regression models were used to investigate the association among WBC count (as a continuous variable and quartiles) and the other variables with the occurrence of new-onset PAD in both univariate and multivariate analyses. Covariables that showed a relation to PAD or atherosclerosis disease were selected based on previous studies.6, 7, 8, 13, 16
Three sets of multivariable models were used to examine the association of WBC count in a hierarchical manner. Model 1 did not adjust for other variables, model 2 adjusted for age and sex and model 3 further adjusted for traditional risk factors, including BMI, current smoking and drinking, hypertension, diabetes mellitus, dyslipidemia, CVD, antihypertensive agents, lipid-lowering agents and hypoglycemic agents.
All analyses were performed using Empower(R) (www.empowerstats.com, X&Y solutions Boston, MA, USA) and R (http://www.R-project.org). A P-value of <0.05 (two-sided) was considered statistically significant for all tests.
Results
Patient characteristics
Baseline characteristics of all participants, overall and stratified by quartiles of WBC count, are shown in Table 1. Participants were 56.71±8.57 years old; 35.9% were male; and the mean (s.d.) BMI was 26.03±3.35 kg m−2. Hypertension was present in 49.1% (n=1746) of the participants, diabetes in 23.8% (n=847), dyslipidemia in 71.8% (n=2552) and tobacco use in 18.5% (n=658). At the time of enrollment, 12.4% (n=441) of participants had CVD. Participants with higher WBC count had a significantly higher BMI; prevalence of hypertension, diabetes mellitus and CVD; and usage of antihypertensive drugs, hypoglycemic drugs and lipid-lowering drugs.
Predictors of new-onset PAD
After a mean 2.3-year (median: 2.34; 25th percentile–75th percentile: 2.28–2.39) follow-up, the incidence of PAD was 2.7% over 2.3 years. Table 2 displays the results of multivariate regression for the association of WBC count with new-onset PAD. WBC count was significantly associated with PAD incidence (odds ratio (OR)=1.27, 95% confidence interval (CI): 1.14–1.41, P<0.0001) with every 1 × 109 l−1 increase in WBC count in model 1. This relationship remained significant (OR=1.21, 95% CI: 1.08–1.36, P=0.0014) even after adjusting for sex, age, BMI, current smoking and drinking, hypertension, diabetes mellitus, dyslipidemia, CVD, antihypertensive agents, lipid-lowering agents and hypoglycemic agents.
Consistently, the risks of new-onset PAD were also dose-dependently related to the quartiles of WBC count in the multivariate regression models. The relationship between WBC count and the risk of new-onset PAD in model 3 was less significant after adjusting for various confounders, although a WBC count in the top quartile (⩾7.0 × 109 l−1) was associated with an OR of 2.14 (95% CI: 1.09–4.22, P=0.027) for PAD compared with the bottom quartile (⩽5.0 × 109 l−1). Furthermore, even after adjusting for baseline ABI, the trend was still the same (a WBC count in the top quartile was associated with an OR of 2.17 (95% CI: 1.08–4.36, P=0.029) for PAD compared with the bottom quartile).
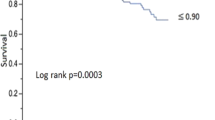
Subgroup analyses are presented in Figure 1. We did not find significant heterogeneity among the analyzed subgroups based on sex (male or female), age (<60 or ⩾60 years old), BMI (<25 or ⩾25 kg m−2), current smoking, current drinking, hypertension, diabetes mellitus, dyslipidemia or CVD.
Subgroup analyses and interaction among variables. We used model 3 that adjusted for sex, age, BMI, current smoking and drinking, hypertension, diabetes mellitus, dyslipidemia, cardiovascular disease, antihypertensive agents, lipid-lowering agents and hypoglycemic agents for the subgroup analyses. BMI, body mass index; CI, confidence interval; CVD, cardiovascular disease; OR, odds ratio; PAD, peripheral arterial disease.
Discussion
Multiple lines of evidence indicate that inflammation markers such as WBC count are strongly associated with higher atherosclerotic risk.5, 6, 16, 17, 18, 19, 20, 21 The main finding of our study is that higher WBC counts were associated with a higher incidence of PAD in a community-based population in China. Therefore, based on these findings, we can use WBC counts to predict new-onset PAD in the future.
We have previously noted several studies that investigated WBC count and PAD in different cohorts; most of the studies were cross-sectional. In the National Health and Nutrition Examination Survey (NHANES) (1999–2002), a white blood cell count in the top quartile (>7.3 × 103 per mm3) was associated with an OR of 1.67 for peripheral arterial disease (ABI <0.9) compared with that in the bottom quartile (⩽4.9 × 103 per mm3).16 A nested case–control study of an American population showed that the total cholesterol/high-density lipoprotein C ratio was the strongest lipid predictor of PAD incidence (relative risk for those in the highest vs. lowest quartile, 3.9; 95% CI: 1.7–8.6) after an average 9-year follow-up period, whereas C-reactive protein was the strongest nonlipid predictor (relative risk for the highest vs. lowest quartile, 2.8; 95% CI: 1.3–5.9); however, they did not study WBC counts.14
Moreover, WBC count is also a strong independent risk factor for other cardiovascular events and for the prevalence as well as progression of subclinical atherosclerosis. Friedman et al.22 demonstrated that WBC count was a predictor of myocardial infarction in 1974. Another analysis of the NHANES database found that systemic inflammation may contribute to an increased risk of death from coronary heart disease. Compared with subjects with a WBC count (× 109 l−1) <6.1, subjects with a WBC count >7.6 were at increased risk of death from coronary heart disease (relative risk=1.4, 95% CI: 1.1–1.8) after adjusting for smoking status and other CVD risk factors.20 Arain et al.23 found that WBC count provides incremental information about the risk of death in a small group of patients with PAD; patients in the top tertile of WBC count had a relative risk of mortality of 3.37 (95% CI: 1.56–7.27).
However, our study is the first to demonstrate that WBC count is a significant predictor of PAD incidence in a community-based Chinese population cohort after a median 2.3-year follow-up rather than from a cross-sectional study. Meanwhile, we did not find significant heterogeneity among other atherosclerosis risk factors, such as sex, age, BMI, current smoking, current drinking, hypertension, diabetes mellitus, dyslipidemia or CVD in the subgroup analyses.
Our study has several limitations. First, our study participants were from a Chinese community-based population with normal ABI at baseline, and the generalizability of the data to other populations remains to be verified. Second, the incidence of new-onset PAD was calculated from data from only two timepoints, and a progression based on multiple time points would enhance the accuracy of PAD diagnosis. Third, a previous study demonstrated that monocyte count, a subtype of WBC count, was independently associated with PAD in a large population-based study.19 However, our study lacked this variable because of funding limitations. Finally, the rate of new-onset PAD in our studied population was relatively low because of short-term follow-up that may affect the association between WBC count and new-onset PAD and also the results of the subgroup analyses. However, there are still positive findings to be observed in this study.
Conclusion
Elevated WBC counts independently predict the risk of new-onset PAD in a Chinese community-based population, supporting the hypothesis that systemic inflammation plays an important role in PAD development.
References
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 385: 117–171.
Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, Browner D . Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 1992; 326: 381–386.
Steg PG, Bhatt DL, Wilson PW, D'Agostino R Sr, Ohman EM, Röther J, Liau CS, Hirsch AT, Mas JL, Ikeda Y, Pencina MJ, Goto S, REACH Registry Investigators. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007; 297: 1197–1206.
Selvin E, Erlinger TP . Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation 2004; 110: 738–743.
Suzuki J, Shimamura M, Suda H, Wakayama K, Kumagai H, Ikeda Y, Akazawa H, Isobe M, Komuro I, Morishita R . Current therapies and investigational drugs for peripheral arterial disease. Hypertens Res 2016; 39: 183–191.
Wildman RP, Muntner P, Chen J, Sutton-Tyrrell K, He J . Relation of inflammation to peripheral arterial disease in the national health and nutrition examination survey, 1999-2002. Am J Cardiol 2005; 96: 1579–1583.
Haumer M, Amighi J, Exner M, Mlekusch W, Sabeti S, Schlager O, Schwarzinger I, Wagner O, Minar E, Schillinger M . Association of neutrophils and future cardiovascular events in patients with peripheral artery disease. J Vasc Surg 2005; 41: 610–617.
Vidula H, Tian L, Liu K, Criqui MH, Ferrucci L, Pearce WH, Greenland P, Green D, Tan J, Garside DB, Guralnik J, Ridker PM, Rifai N, McDermott MM . Biomarkers of inflammation and thrombosis as predictors of near-term mortality in patients with peripheral arterial disease: a cohort study. Ann Intern Med 2008; 148: 85–93.
Sabatine MS, Morrow DA, Cannon CP, Murphy SA, Demopoulos LA, DiBattiste PM, McCabe CH, Braunwald E, Gibson CM . Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservati. J Am Coll Cardiol 2002; 40: 1761–1768.
Rossi E, Biasucci LM, Citterio F, Pelliccioni S, Monaco C, Ginnetti F, Angiolillo DJ, Grieco G, Liuzzo G, Maseri A . Risk of myocardial infarction and angina in patients with severe peripheral vascular disease: predictive role of C-reactive protein. Circulation 2002; 105: 800–803.
Haim M, Boyko V, Goldbourt U, Battler A, Behar S . Predictive value of elevated white blood cell count in patients with preexisting coronary heart disease: the Bezafibrate Infarction Prevention Study. Arch Intern Med 2004; 164: 433–439.
Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T, Hacke W, CAPRIE Investigators. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke 2004; 35: 1147–1152.
Libby P . Inflammation in atherosclerosis. Nature 420: 868–874.
Ridker PM, Stampfer MJ, Rifai N . Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA 2001; 285: 2481–2485.
Fan F, Qi L, Jia J, Xu X, Liu Y, Yang Y, Qin X, Li J, Li H, Zhang Y, Huo Y . Noninvasive central systolic blood pressure is more strongly related to kidney function decline than peripheral systolic blood pressure in a Chinese community-based population. Hypertension 2016; 67: 1166–1172.
Chen JJ, Lin LY, Lee HH, Lai LP, Lin JL, Huang JJ, Tseng CD . Association of white blood cell count and peripheral arterial disease in patients with and without traditional risk factors. Angiology 2010; 61: 382–387.
Rein P, Saely CH, Silbernagel G, Vonbank A, Mathies R, Drexel H, Baumgartner I . Systemic inflammation is higher in peripheral artery disease than in stable coronary artery disease. Atherosclerosis 2015; 239: 299–303.
Weijenberg MP, Feskens EJM, Kromhout D . White blood cell count and the risk of coronary heart disease and all-cause mortality in elderly men. Arterioscler Thromb Vasc Biol 1996; 16: 499–503.
Nasir K . Relationship of monocyte count and peripheral arterial disease: results From the National Health and Nutrition Examination Survey 1999-2002. Arterioscler Thromb Vasc Biol 2005; 25: 1966–1971.
Brown DW, Giles WH, Croft JB . White blood cell count: an independent predictor of coronary heart disease mortality among a national cohort. J Clin Epidemiol 2001; 54: 316–322.
Gang L, Yanyan Z . Increased neutrophil to lymphocyte ratio in persons suffering from hypertension with hyperhomocysteinemia. Hypertens Res 2016; 39: 606–611.
Friedman GD, Klatsky AL, Siegelaub AB . The leukocyte count as a predictor of myocardial infarction. N Engl J Med 1974; 290: 1275–1278.
Arain FA, Khaleghi M, Bailey KR, Lahr BD, Rooke TW, Kullo IJ . White blood cell count predicts all-cause mortality in patients with suspected peripheral arterial disease. Am J Med 2009; 122: e1–e7.
Acknowledgements
We thank the staff of the Gucheng and Pingguoyuan Community Health Centers as well as the research coordinators who participated in this cohort study. This study was supported by a grant from the UM-PUHSC Joint Institute for Translational and Clinical Research (Grant No. BMU20110177).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Li, Y., Fan, F., Jia, J. et al. WBC count predicts the risk of new-onset peripheral arterial disease in a Chinese community-based population. Hypertens Res 40, 932–936 (2017). https://doi.org/10.1038/hr.2017.64
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.64
Keywords
This article is cited by
-
Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study
Journal of Human Hypertension (2020)
-
Longitudinal changes of cardiac troponin and inflammation reflect progressive myocyte stretch and likelihood for hypertension in a Black male cohort: The SABPA study
Hypertension Research (2019)