Abstract
Hypertension aggravates macrovascular and microvascular diseases and mortality in patients with type 2 diabetes mellitus (T2DM). The current Japanese Society of Hypertension Guidelines of the Management of Hypertension (JSH 2014) recommends that antihypertensive medication should be initiated concomitantly with lifestyle modification when blood pressure (BP) is ⩾130/80 mm Hg and that target levels of office and home BP should be <130/80 mm Hg and <125/75 mm Hg, respectively, in T2DM patients. Considering more favorable metabolic profiles and renoprotective effects than other classes of antihypertensive agents, angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are recommended as the first-line therapy for patients with hypertension and T2DM in JSH 2014. However, the target BP and the first-line therapy remain controversial because of the paucity of high-quality evidence with consistency. It is suggested that BP management should be tailored for each patient with T2DM, based on tolerability and considerations of comorbidity.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease, which includes angina pectoris, acute coronary syndromes, myocardial infarction (MI), stroke, transient ischemic attack, peripheral artery disease and coronary or other arterial revascularization, is the leading cause of morbidity and mortality among diabetic patients. Hypertension and type 2 diabetes mellitus (T2DM) develop and progress based on common lifestyle-related background factors such as obesity, metabolic syndromes and insulin resistance. The age-adjusted prevalence of hypertension in adults with T2DM is 57.3% as compared with 28.6% in those without diabetes.1 On the other hand, patients with hypertension are ∼2.5 times more likely to have impaired glucose metabolism.2 Blood pressure (BP) elevation increases the risk of not only macrovascular diseases, namely atherosclerotic cardiovascular disease, but also microvascular diseases (for example, retinopathy and nephropathy) in T2DM.3 In addition, BP control reduces the risk of mortality and both macro- and microvascular diseases in T2DM.4, 5 Therefore, the strict control of blood glucose and BP has been long emphasized for the prevention and treatment of micro- and macrovascular diseases. Recently, however, the Action to Control Cardiovascular Risks in Diabetes trial (ACCORD), as well as a subanalysis of the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation trial (ADVANCE), have raised the concern that tight glycemic control may be harmful for T2DM patients at high risk of cardiovascular disease, leading to an increase in the frequency of severe hypoglycemic episodes.6, 7 In addition, BP targets and the selection of antihypertensive agents as the first-line therapy remain controversial in patients with hypertension and T2DM.8, 9 This article briefly addresses the current concepts of BP management in patients with T2DM.
Blood pressure targets
Previous guideline recommendations
In the UK Prospective Diabetes Study (UKPDS) 36, a prospective randomized observational study, the risks of microvascular diseases, macrovascular diseases (MI and stroke) and heart failure were increased in T2DM patients with systolic BP (SBP) >120 mm Hg, and each 10 mm Hg reduction in SBP was associated with a 12%, 10% and 13% risk reduction in MI, stroke and microvascular disease, respectively.3 UKPDS 38 demonstrated that, in T2DM patients (baseline BP, 160/94 mm Hg), tight BP control targeting 150/85 mm Hg (achieved 144/82 mm Hg) resulted in lower incidences of stroke, diabetes-related death and microvascular disease than modest BP control targeting 180/105 mm Hg (achieved 154/87 mm Hg).4 In a post hoc analysis of the Hypertension Optimal Treatment study (HOT) comprising hypertensive patients with T2DM (baseline BP, 170/105 mm Hg), the intensive BP-lowering group targeting a diastolic BP (DBP) <80 mm Hg (achieved 81.1 mm Hg) showed decreased cardiovascular events and all-cause mortality compared with the BP-lowering groups targeting DBP <85 mm Hg and DBP <90 mm Hg (achieved 83.2 mm Hg and 85.2 mm Hg, respectively).5 The Appropriate Blood Pressure Control in Diabetes trial (ABCD) demonstrated that among hypertensive T2DM patients (baseline BP, 155/98 mm Hg), all-cause mortality was reduced in the intensive BP control group (targeted DBP of 75 mm Hg; achieved 132/78 mm Hg) as compared with the moderate control group (targeted DBP of 80–90 mm Hg; achieved 138/86 mm Hg).10 In the ABCD normotensive trial enrolling T2DM patients with high-normal BP (baseline BP, 136/84 mm Hg), the intensive BP control group targeting DBP<75 mm Hg (achieved 128/75 mm Hg) showed a lower incidence of diabetic nephropathy and stroke than the moderate BP control group (achieved 137/81 mm Hg).11 Although no randomized controlled trials (RCTs) have directly investigated whether targeting BP <130/80 mm Hg or 130–140 mm Hg improves clinical outcomes more effectively and safely, the previous guidelines for the management of hypertension, including the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2009 (JSH 2009), the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) and the 2007 Guidelines for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology (ESH/ESC 2007), recommend <130/80 mm Hg as a target level of BP control in diabetic patients.12, 13, 14
Recent guideline recommendations
In 2010, the ACCORD-BP trial demonstrated that in T2DM patients with hypertension (baseline BP, 139/76 mm Hg), the incidence of major adverse cardiovascular events, including cardiovascular death, non-fatal MI and nonfatal stroke, did not differ between the intensive BP control group targeting SBP <120 mm Hg (achieved 119/64 mm Hg) and the standard BP control group targeting SBP <140 mm Hg (achieved 133/71 mm Hg), whereas serious adverse effects, such as hypotension, arrhythmia and bradycardia, were significantly increased in the intensive BP control group.15 However, a significant risk reduction for stroke was observed in the strict BP control group.15 A subgroup analysis of the International Verapamil SR-Trandolapril Study (INVEST) involving T2DM patients with hypertension and coronary artery disease (CAD) (baseline BP, 151/68 mm Hg) showed that the incidence of cardiovascular events in patients with an achieved SBP of <130 mm Hg was lower than that in those with SBP of ⩾140 mm Hg, but no differences were observed compared with those with SBP of 130–139 mm Hg.16 In a subgroup analysis of the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) with T2DM patients at high risk of cardiovascular disease (baseline BP, 143/82 mm Hg), the risk of the composite of cardiovascular death, nonfatal MI nonfatal stroke and hospitalized heart failure was lowest at an achieved SBP of 130 mm Hg, and no benefit was seen in cardiovascular outcomes by reducing SBP below 130 mm Hg.17 In contrast, a progressive reduction was observed in the incidence of stroke down to SBP of 115 mm Hg.17 A meta-analysis by Reboldi et al.18 of 73 913 T2DM patients in 31 RCTs demonstrated that BP-lowering therapy reduced the risk of stroke and MI by 9% and 11%, respectively, and that tighter BP control decreased the risk of stroke by 31% compared with lenient control; however, the risk reduction for MI did not reach statistical significance. On meta-regression analysis, the risk of stroke decreased by 13% for each 5 mm Hg reduction in SBP and 11.5% for each 2 mm Hg reduction in DBP. In contrast, the risk of MI did not show significant association with the extent of BP reduction.18 A meta-analysis by Bangalore et al.19 of 13 randomized trials enrolling 37 736 participants with T2DM or impaired glucose tolerance showed that the intensive BP control was associated with a 10% reduction in all-cause mortality, a 17% reduction in stroke and a 20% increase in serious adverse effects compared with standard BP control, whereas no differences were seen in other macrovascular and microvascular events. On a Bayesian random-effects model, more intensive BP control targeting SBP ⩽130 mm Hg was associated with a greater reduction in stroke, but not other events.19 Meta-regression analysis showed continued risk reduction for stroke to SBP of <120 mm Hg; however, at SBP <130 mm Hg, there was a 40% increase in serious adverse events with no benefit for other outcomes.19 Accordingly, based on the paucity of high-quality evidence for the benefit of intensive BP control targeting BP <130/80 mm Hg with regard to cardiovascular events, particularly MI, recent guidelines for the management of hypertension in Europe and the United States revised the BP target in patients with T2DM as follows: <140/85 mm Hg in ESH/ESC 2013,20 <140/90 mm Hg in JNC 8,21 and <140/80 mm Hg in the American Diabetic Association Clinical Practice Recommendation 2014 (ADA 2014) (Table 1).22
Current Japanese guideline recommendations
With regard to hypertensive organ damage, the disease structure differs between Japan and Europe or the United States. In Japan, the incidence of stroke is relatively higher than that of MI, whereas MI is the major consequence of hypertension in Europe and the United States. As shown in the Hisayama Study and the Suita Study, the incidence of cerebral infarction is 1.5–2.5 times higher than that of MI in the Japanese general population.23, 24 The Japan Diabetes Complications Study (JDCS) reported that in Japanese patients with T2DM, the incidence of cerebral infarction and MI was 6.29 and 3.84 per 1000 person-year, respectively,25 whereas the ACCORD-BP trial showed that the incidence of cerebral infarction and MI was 3.2 and 11.03 per 1000 person-year, respectively, in the intensive control group and 5.3 and 12.8 per 1000 person-year, respectively, in the standard control group.15 In the Tanno-Sobetsu Cho study, borderline diabetic/diabetic Japanese subjects with BP ⩾140/85 mm Hg had significantly higher cardiovascular mortality than those with BP <130/85 mm Hg.26 On the other hand, the ACCORD-BP diabetes meta-analysis of Reboldi et al.18 and the diabetes/impaired glucose tolerance meta-analysis of Bangalore et al.19 provided evidence suggesting a benefit of lowering SBP down to 130 mm Hg for stroke prevention that differed from other cardiovascular events.15, 18, 19 Taken together, it appears plausible to set the target level of BP control in Japan to <130/80 mm Hg in T2DM patients.
Accordingly, JSH 2014 recommends <130/80 mm Hg as the target of office BP of T2DM patients.27 In addition, according to a subanalysis of the Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) study,28 JSH 2014 establishes <125/75 mm Hg as the target home BP in T2DM patients.27 In elderly patients with T2DM, as the first step, BP should be targeted at <140/90 mm Hg in those aged 65–74 years and at <150/90 mm Hg in those aged over 75 years. Thereafter, if treatment is tolerated, BP <130/80 mm Hg should be carefully targeted.27
Therapeutic strategy
Lifestyle modifications
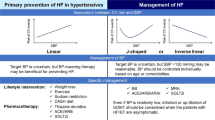
Life-style modifications, including weight loss, physical exercise, smoking cessation and reduced intake of alcohol and salt, are essential in reducing cardiovascular risk in patients with T2DM, irrespective of combined hypertension.29 Such nonpharmacological approaches improve not only glycemic but also BP control by ameliorating insulin sensitivity. JSH 2014 recommends that antihypertensive medication should be initiated concomitantly with lifestyle modifications when BP is ⩾130/80 mm Hg (Figure 1).27 In patients with BP of 130–139/80–89 mm Hg, lifestyle modifications alone may be attempted for at most 3 months if the target BP goal is expected to be achievable.
Treatment plan for hypertension associated with type 2 diabetes mellitus (T2DM) indicated by the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2014. Cited from Shimamoto et al.27.
Pharmaceutical treatment
Monotherapy. Regarding the selection of antihypertensive drugs for T2DM patients, consideration should be given to the effects of each drug on insulin sensitivity, glucose/lipid metabolism and diabetic nephropathy, in addition to the benefit for cardiovascular mortality and morbidity. High-dose thiazide-type diuretics and conventional β-blockers are known to reduce insulin sensitivity and increase serum triglycerides levels.27 Renin–angiotensin system (RAS) inhibitors, that is, angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs), and long-acting dihydropyridine calcium channel blockers (CCBs) improve insulin sensitivity and exert no adverse effects on lipid metabolism.30 ARBs and ACEIs seem more effective than CCBs in preventing the new occurrence of T2DM.31, 32, 33
It has also been shown that major classes of antihypertensive agents, such as ACEIs,34 ARBs,35, 36, 37, 38, 39 thiazide-type diuretics40, 41 and β-blockers,42 prevent diabetic nephropathy (renal function reduction and albuminuria/proteinuria). Among the CCBs, N-type and N/T-type calcium channel blockers, such as cilnidipine, efonidipine, benidipine and azelnidipine, reduce proteinuria in hypertensive patients with chronic kidney disease.43, 44, 45, 46 A meta-analysis by Casas et al.47 of placebo-controlled trials demonstrated that RAS inhibitors were superior to other antihypertensive agents in improving renal outcomes, including the doubling of serum creatinine, the progression of end-stage renal disease and the deterioration of the glomerular filtration rate.
The usefulness of antihypertensive agents in the prevention of cardiovascular disease in patients with hypertension and T2DM has been demonstrated in a subanalysis of the Captopril Prevention Project (CAPPP) using ACEIs,48 in the HOT study and a diabetes subanalysis of the Systolic Hypertension in Europe trial (Syst-Eur) using CCBs,5, 49 in the UKPDS 39 using an ACEI or a β-blocker42 and in a diabetes subanalysis of the Losartan Intervention For Endpoint Reduction in Hypertension study (LIFE) using an ARB.50 The LIFE subanalysis demonstrated that an ARB was superior to a β-blocker in reducing all-cause mortality and cardiovascular mortality and morbidity in T2DM patients with hypertension.50 Taken together with more favorable metabolic profiles and renoprotective effects than other classes of antihypertensive agents, ACEIs and ARBs are recommended as the first-line therapy for patients with hypertension and T2DM in JSH 2014 (Table 1 and Figure 1).27
Combination therapy. Most T2DM patients are not well controlled with a single antihypertensive drug, in many cases with ACEI or ARB monotherapy. Although the evidence regarding combination therapy is limited, the current guidelines recommend the addition of a CCB or a low dose of a thiazide-type diuretic as add-on therapy (Figure 1).20, 21, 27 In the Gauging Albuminuria Reduction with Lotrel in Diabetic Patients with Hypertension study (GURD), a combination of an ACEI with a thiazide-type diuretic was more effective for reducing proteinuria, whereas a combination of an ACEI and a CCB was superior in maintaining the estimated glomerular filtration rate.51 A RCT comprising 150 patients with hypertension and T2DM showed that a combination of an ARB and a CCB induced a greater BP reduction and larger improvement of insulin resistance compared with a combination of an ARB and a thiazide-type diuretic.52 The diabetes subanalysis of the Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension study (ACCOMPLISH) demonstrated that a combination therapy with an ACEI and a CCB was more effective than a combination therapy with an ACEI and a thiazide-type diuretic for preventing cardiovascular events in hypertensive T2DM patients with CAD, left ventricular hypertrophy, peripheral artery disease or renal dysfunction.53 However, it remains unclear whether CCBs or thiazide-type diuretics should be appropriated as the second-line drug in T2DM patients already being treated with a RAS inhibitor. When further BP reduction is necessary after a combination of a RAS inhibitor and either a CCB or a thiazide-type diuretic, triple therapy with the three classes of antihypertensive agents is recommended as the next step.
Aldosterone antagonists (that is, spironolactone and eplerenone) would be recommended as the fourth-line drugs when hypertension is not well controlled after triple therapy with a RAS inhibitor, a CCB and a thiazide-type diuretic.54 It was demonstrated that an addition of an aldosterone antagonist on a RAS inhibitor not only improved insulin resistance and prevented clinical progression of nephropathy in T2DM patients without overt nephropathy but also maintained long-term antiproteinuric and antialbuminuric effects in chronic kidney disease patients with proteinuria.55 However, it should be noted that, in Japan, the use of eplerenone is not approved for diabetic hypertensive patients with albuminuria or proteinuria.
In the ONTARGET, a combination of an ACEI and an ARB provided no additional benefit and showed a higher incidence of adverse events such as hypotension, syncope and renal dysfunction.56 Similarly, the Veteran Affairs Nephropathy in Diabetes trial (VA NEPHRON-D) showed no benefits from a combination of an ACEI and an ARB and an increase in the adverse events in patients with diabetic nephropathy.57 Accordingly, the combined use of an ACEI and an ARB is not recommended. Based on the results of the Aliskiren Trial in Type 2 Diabetes Using Cardiorenal End-points (ALTITUDE), the direct renin inhibitor aliskiren should not be used in combination with RAS inhibitors in T2DM patients who are at high risk for cardiovascular and renal events.58
Specific considerations
Diabetic neuropathy
Patients with diabetic neuropathy are often associated with BP autoregulation dysfunction because of the impairment of the peripheral sympathetic nervous system and/or baroreflex system that results in orthostatic hypotension and postprandial hypotension, as well as exaggerated BP variability and fluctuation.29 To avoid falls, bone fracture, major organ ischemia, cardiovascular/cerebrovascular events and cardiovascular morbidity, the attention should be paid to screening for excessive BP decreases induced by diabetic neuropathy; in diabetic patients, BP should be measured in both the recumbent and standing positions, as well as the sitting position.27 In addition, close BP monitoring in a nonclinical setting using home BP assessment and 24 h ambulatory BP monitoring is recommended.
Elderly diabetic patients
JSH 2014 recommends a target BP of <140/90 mm Hg in general hypertensive patients aged 65–74 years and <150/90 mm Hg in those aged ⩾75 years.27 If treatment is well tolerated, stricter BP control targeting <140/90 or <130/80 mm Hg may improve outcomes in T2DM patients aged ⩾75 years but otherwise healthy. It is plausible that lower BP target levels can be maintained if lower BP has been achieved with few drugs without any side effects at younger ages.
J-curve phenomenon
There is a concern that the excessive BP lowering below a level at which organ perfusion is impaired (for example, SBP <120 or 130 mm Hg or DBP <70 mm Hg) would increase cardiovascular mortality and morbidity in diabetic patients.15, 16 The patient group with low BP was older and had a higher incidence of comorbidities such as CAD and peripheral artery disease. Recently, a community-based large-scale cohort study showed that low BP was associated with an increased risk of cardiovascular events in T2DM patients, independently of antihypertensive therapy.59 A post hoc analysis of the INVEST showed that although cardiovascular events increased in CAD patients with low DBP (that is, <70 mm Hg), but not low SBP, coronary revascularization (percutaneous coronary intervention and coronary artery bypass surgery) reduced the risk by half or more in hypertensive CAD patients.60 Moreover, a subanalysis of the CREDO-KYOTO Registry Cohort-1 revealed that low DBP was associated with an increased risk of cardiovascular death, but not MI and stroke, in CAD patients after revascularization, whereas low SBP had no effect on cardiovascular outcomes.61 It is noteworthy that low DBP and T2DM were not significant factors predicting cardiovascular death in CAD patients after revascularization, even in those aged ⩾75 years.61, 62 In T2DM patients, it remains unclear whether antihypertensive treatment increases cardiovascular risk with the causal relationship or whether these adverse effects were simply the results of comorbidities, such as preexisting arteriosclerosis, atherosclerotic cardiovascular disease, symptomatic or asymptomatic left ventricular dysfunction, chronic kidney disease and other systemic illness, that is, reverse causality. Taken together, these findings suggest that the screening and treatment of myocardial ischemia and the management of cardiovascular and noncardiovascular comorbidities are important in treating T2DM patients with low BP.
Proper use of β-blockers
It has been established that β-blockers reduce all-cause mortality in T2DM patients with heart failure with reduced ejection fraction as well as in nondiabetic ones.63 The use of β-blockers has also been shown to ameliorate the survival rate after acute MI in both diabetic and nondiabetic patients, with the beneficial effect being more evident in diabetic patients.64 Although there is concern about the possibility that β-blockers may mask the symptom of hypoglycemia and delay the recovery from hypoglycemia,27 a post hoc analysis of the ACCORD showed that treatment with β-blockers reduced all-cause and cardiovascular mortality in T2DM patients receiving intensive glycemic therapy, but not in those receiving standard therapy, probably by decreasing hypoglycemia-associated lethal arrhythmia and death.65 Among the β-blockers, carvedilol, an αβ-blocker, and bisoprolol, a highly β1-selective blocker, are considered useful as adjunctive therapy in hypertension treatment as opposed to monotherapy based on their favorable or neutral effects on metabolic profiles that differ from conventional β-blockers.66 Accordingly, carvedilol and bisoprolol should be used properly to improve unfavorable cardiovascular outcomes in T2DM patients, particularly those with CAD and/or heart failure patients with reduced ejection fraction.
Areas in need of future research
Target BP levels
Recently, the Systolic Blood Pressure Intervention Trial (SPRINT), which used automated office BP measurement, showed that a target SBP of <120 mm Hg (achieved 121.4 mm Hg) reduced composite end points (MI, other acute coronary syndromes, stroke, acute decompensated heart failure and cardiovascular death) by 25% and all-cause death by 27% in individuals with baseline SBP ⩾130 mm Hg at high cardiovascular risk, but those with diabetes or prior cerebrovascular disease were excluded.67 These results have had great impact on the issue regarding the ideal target BP in hypertensive patients. A meta-analysis by Brunström and Carlberg68 of 49 RCTs comprising 73 738 individuals (mostly diabetes) demonstrated that BP lowering was associated with reductions in all-cause mortality, MI and stroke in individuals with SBP >140 mm Hg at baseline, whereas further BP reduction was related to increased cardiovascular mortality in individuals with SBP <140 mm Hg at baseline (Figure 2a). In addition, an achieved SBP of 130–139 mm Hg was shown to reduce all-cause mortality and MI, whereas an achieved SBP <130 mm Hg minimized the risk of stroke and showed a trend of increased all-cause mortality and cardiovascular mortality (Figure 2b).68 A recent meta-analysis by Emdin et al.69 of 40 RCTs comprising 100 354 patients demonstrated that each 10 mm Hg SBP reduction was associated with a significant reduction in all-cause mortality, cardiovascular events, CAD, stroke, retinopathy and albuminuria in patients with baseline SBP ⩾140 mm Hg or an achieved SBP ⩾130 mm Hg (Figure 3). It is noteworthy that an achieved SBP <130 mm Hg was associated with a lower risk of stroke and albuminuria, regardless of baseline SBP.69 According to recent real-world large-scale data from the Swedish national diabetes register comprising 187 106 diabetic patients aged ⩽75 years without previous cardiovascular or other major diseases, the patient group with the lowest SBP (110–119 mm Hg) had a significantly lower risk of total and nonfatal acute MI, total and nonfatal cardiovascular disease and nonfatal CAD than the group with SBP of 130–139 mm Hg.70 In addition, there was no indication of a J-shaped relationship between SBP and end points other than heart failure and all-cause mortality.70 Accordingly, it is plausible that most patients with hypertension and T2DM should be treated to the first BP target of <140/80 mm Hg. Lower BP targets, such as 130/80 mm Hg, may be appropriate for T2DM patients at high risk of cardiovascular diseases, particularly stroke, if they can be achieved without undue treatment burden.71 RCTs are needed to determine which T2DM patients, especially those with a greater risk of stroke than CAD such as Japanese and East Asian individuals, receive the greatest benefit from lower BP targets.
Effects of baseline and achieved systolic blood pressure (SBP) on mortality and cardiovascular morbidity in patients with type 2 diabetes mellitus (T2DM). Results from meta-analyses stratified according to baseline SBP (a) and achieved SBP (b), reported separately for each outcome. Adopted from Brunström and Carlberg.68
(a) Standardized associations of 10 mm Hg systolic blood pressure (SBP) reduction with all-cause mortality and macro- and microvascular outcomes in type 2 diabetes mellitus (T2DM) patients. (b) Standardized associations of 10 mm Hg SBP reduction with all-cause mortality and macro- and microvascular outcomes, stratified by mean achieved SBP in the active drug group of each trial. Cited from Emdin et al.69
First-line therapy
The superiority of ACEIs and ARBs over other antihypertensive drugs in preventing cardiovascular outcomes has not been shown to be consistent for all patients with T2DM.69, 72 A meta-analysis by Emdin et al.69 suggested that CCBs or thiazide-type diuretics provided cardiovascular benefits similar to those of ACEIs and ARBs in T2DM patients. Another meta-analysis by Bangalore et al.72 of 19 RCTs comprising 25 414 diabetic patients, which excluded cohorts with a history of heart failure, showed that ACEIs and ARBs are both associated with a risk of all-cause mortality, cardiovascular mortality, MI, angina, stroke, heart failure, revascularization and end-stage renal failure, similar to CCBs, thiazide-like diuretics and β-blockers (Figure 4). These findings support the recommendations of the ESC/ESH 2013 and JNC 8 to use other antihypertensive drugs in T2DM patients without kidney disease.20, 21 The efficacy of various antihypertensive drugs and their combinations need to be investigated in future RCTs.
Mortality and cardiovascular outcomes with renin–angiotensin system (RAS) inhibitors compared with calcium channel blockers (CCBs; top), diuretics (middle) and β-blockers (bottom) in patients with type 2 diabetes mellitus (T2DM). Cited from Bangalore et al.72
Beneficial effects of new antidiabetic medications on the control of hypertension
In the past few decades, the use of new antidiabetic medications, such as glucagon-like-polypeptide 1 (GLP1) analogs, dipeptidyl peptidase-4 (DDP4) inhibitors and sodium-glucose co-transporter 2 (SGLT2) inhibitors, has been widespread in clinical practice. GLP1 analogs have a neutral effect on BP, or may even result in a mild BP decrease, whereas DDP4 inhibitors do not significantly affect BP control.73 SGLT2 inhibitors have been shown to significantly reduce SBP by 3–5 mm Hg and DBP by 2–3 mm Hg.74 Moreover, the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG) OUTCOME trial enrolling 7020 T2DM patients at very high risk for cardiovascular events demonstrated that the addition of empagliflozin, a SGLT2 inhibitor, to the standard therapy reduced cardiovascular mortality, nonfatal MI, and nonfatal stroke, as well as all-cause mortality.75 Apparently, the beneficial effects of empagliflozin on cardiovascular events are primarily related to the reduction in all-cause mortality, cardiovascular mortality and hospitalization for heart failure, but not to the reduction in atherosclerotic cardiovascular disease, including MI and stroke. Currently, although several possible mechanisms have been suggested including SBP reduction, the intravascular/extracellular fluid volume reduction through natriuresis, osmotic diuresis and loop diuretics-mimic effect without sympathetic nervous system activation, cardiac afterload reduction and so on, the mechanism whereby empagliflozin improves cardiovascular outcomes remain unclear.76, 77 Future studies are needed to determine the precise mechanism of the action on cardiovascular events and to clarify whether the beneficial effects are the class effects of SGLT2 inhibitors or the specific drug effects of empagliflozin.
The target BP and the first-line therapy for patients with hypertension and T2DM remain controversial because of the paucity of high-quality evidence with consistency. It is suggested that BP management should be tailored for each individual patient with T2DM based on tolerability and considerations of comorbidity.
References
Gillespie CD, Hurvitz KA . Prevalence of hypertension and controlled hypertension in the United States, 2007-2010. MMWR Suppl 2013; 62: 144–148.
Gress TW, Nieto FJ, Shahar E, Wofford MR, Brancati FL . Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis Risk in Communities Study. N Engl J Med 2000; 342: 905–912.
Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR . Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000; 321: 412–419.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317: 703–713.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S . Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998; 351: 1755–1762.
ACCORD Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008; 358: 2545–2559.
Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S . Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010; 363: 1410–1418.
Horr S, Nissen S . Managing hypertension in type 2 diabetes mellitus. Best Pract Res Clin Endocrinol Metab 2016; 30: 445–454.
Brunström M, Eliasson M, Nilsson PM, Carlberg B . Blood pressure treatment levels and choice of antihypertensive agent in people with diabetes mellitus: an overview of systematic reviews. J Hypertens 2017; 35: 453–462.
Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW . The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med 1998; 338: 645–652.
Schrier RW, Estacio RO, Esler A, Mehler P . Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int 2002; 61: 1086–1097.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362: 1575–1585.
Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ . Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010; 304: 61–68.
Redon J, Mancia G, Sleight P, Schumacher H, Gao P, Pogue J, Fagard R, Verdecchia P, Weber M, Böhm M, Williams B, Yusoff K, Teo K, Yusuf S . Safety and efficacy of low blood pressures among patients with diabetes: subgroup analyses from the ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial). J Am Coll Cardiol 2012; 59: 74–83.
Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P . Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73 913 patients. J Hypertens 2011; 29: 1253–1269.
Bangalore S, Kumar S, Lobach I, Messerli FH . Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation 2011; 123: 2799–2810.
Mancia G, Fagard R, Narkiewicz K, Redo'n J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F . 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E . 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311: 507–520.
American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care 2014; 37 (Suppl 1): S14–S80.
Doi Y, Ninomiya T, Hata J, Fukuhara M, Yonemoto K, Iwase M, Iida M, Kiyohara Y . Impact of glucose tolerance status on development of ischemic stroke and coronary heart disease in a general Japanese population: the Hisayama study. Stroke 2010; 41: 203–209.
Watanabe M, Kokubo Y, Higashiyama A, Ono Y, Okayama A, Okamura T . New diagnosis criteria for diabetes with hemoglobin A1c and risks of macro-vascular complications in an urban Japanese cohort: the Suita study. Diabetes Res Clin Pract 2010; 88: e20–e23.
Sone H, Tanaka S, Tanaka S, Iimuro S, Oida K, Yamasaki Y, Oikawa S, Ishibashi S, Katayama S, Ohashi Y, Akanuma Y, Yamada N . Serum level of triglycerides is a potent risk factor comparable to LDL cholesterol for coronary heart disease in Japanese patients with type 2 diabetes: subanalysis of the Japan Diabetes Complications Study (JDCS). Clin Endocrinol Metab 2011; 96: 3448–3456.
Onishi H, Saito S, Shimamoto K . Tanno-Sobetsu Study review in 2007. Ther Res 2007; 28: 513–525 (in Japanese).
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–392.
Noguchi Y, Asayama K, Staessen JA, Inaba M, Ohkubo T, Hosaka M, Satoh M, Kamide K, Awata T, Katayama S, Imai Y . Predictive power of home blood pressure and clinic blood pressure in hypertensive patients with impaired glucose metabolism and diabetes. J Hypertens 2013; 31: 1593–1602.
American Diabetes Association. Cariovascular disease and risk manegement. Diabetes Care 2015; 38: S49–S57.
Xiao WY, Ning N, Tan MH, Jiang XS, Zhou L, Liu L, Yi D, Wei P . Effects of antihypertensive drugs losartan and levamlodipine besylate on insulin resistance in patients with essential hypertension combined with isolated impaired fasting glucose. Hypertens Res 2016; 39: 321–326.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua T, Laragh J, McInnes GT, Mitchell L, Plat F, Schork A, Smith B, Zanchetti A . Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004; 363: 2022–2031.
Ogihara T, Nakao K, Fukui T, Fukiyama K, Ueshima K, Oba K, Sato T, Saruta T . Effects of candesartan compared with amlodipine in hypertensive patients with high cardiovascular risks: candesartan antihypertensive survival evaluation in Japan trial. Hypertension 2008; 51: 393–398.
Ruggenenti P, Fassi A, Ilieva AP, Bruno S, Iliev IP, Brusegan V, Rubis N, Gherardi G, Arnoldi F, Ganeva M, Ene-Iordache B, Gaspari F, Perna A, Bossi A, Trevisan R, Dodesini AR, Remuzzi G . Preventing microalbuminuria in type 2 diabetes. N Engl J Med 2004; 351: 1941–1951.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S . Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–869.
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I . Renoprotective effect of the angiotensinreceptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–860.
Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P . The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001; 345: 870–878.
Viberti G, Wheeldon NM . Microalbuminuria reduction with valsartan in patients with type 2 diabetes mellitus: a blood pressure-independent effect. Circulation 2002; 106: 672–678.
Makino H, Haneda M, Babazono T, Moriya T, Ito S, Iwamoto Y, Kawamori R, Takeuchi M, Katayama S . Prevention of transition from incipient to overt nephropathy with telmisartan in patients with type 2 diabetes. Diabetes Care 2007; 30: 1577–1578.
Marre M, Puig JG, Kokot F, Fernandez M, Jermendy G, Opie L, Moyseev V, Scheen A, Ionescu-Tirgoviste C, Saldanha MH, Halabe A, Williams B, Mion Júnior D, Ruiz M, Hermansen K, Tuomilehto J, Finizola B, Gallois Y, Amouyel P, Ollivier JP, Asmar R . Equivalence of indapamide SR and enalapril on microalbuminuria reduction in hypertensive patients with type 2 diabetes: the NESTOR Study. J Hypertens 2004; 22: 1613–1622.
Schram MT, van Ittersum FJ, Spoelstra-de Man A, van Dijk RA, Schalkwijk CG, Ijzerman RG, Twisk JW, Stehouwer CD . Aggressive antihypertensive therapy based on hydrochlorothiazide, candesartan or lisinopril as initial choice in hypertensive type II diabetic individuals: effects on albumin excretion, endothelial function and inflammation in a double-blind, randomized clinical trial. J Hum Hypertens 2005; 19: 429–437.
UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 1998; 317: 713–720.
Fujita T, Ando K, Nishimura H, Ideura T, Yasuda G, Isshiki M, Takahashi K . Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin-angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int 2007; 72: 1543–1549.
Ishimitsu T, Kameda T, Akashiba A, Takahashi T, Ohta S, Yoshii M, Minami J, Ono H, Numabe A, Matsuoka H . Efonidipine reduces proteinuria and plasma aldosterone in patients with chronic glomerulonephritis. Hypertens Res 2007; 30: 621–626.
Nakamura T, Sugaya T, Kawagoe Y, Suzuki T, Ueda Y, Koide H, Inoue T, Node K . Azelnidipine reduces urinary protein excretion and urinary liver-type fatty acid binding protein in patients with hypertensive chronic kidney disease. Am J Med Sci 2007; 333: 321–326.
Ohishi M, Takagi T, Ito N, Terai M, Tatara Y, Hayashi N, Shiota A, Katsuya T, Rakugi H, Ogihara T . Renal-protective effect of T- and L-type calcium channel blockers in hypertensive patients: an Amlodipine-to-Benidipine Changeover (ABC) study. Hypertens Res 2007; 30: 797–806.
Casas JP, Chua W, Loukogeorgakis S, Vallance P, Smeeth L, Hingorani AD, MacAllister RJ . Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes. Lancet 2005; 366: 2026–2033.
Niskanen L, Hedner T, Hansson L, Lanke J, Niklason A . Reduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/β-blocker-based treatment regimen: a subanalysis of the Captopril Prevention Project. Diabetes Care 2001; 24: 2091–2096.
Tuomilehto J, Rastenyte D, Birkenhäger WH, Thijs L, Antikainen R, Bulpitt CJ, Fletcher AE, Forette F, Goldhaber A, Palatini P, Sarti C, Fagard R . Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. N Engl J Med 1999; 340: 677–684.
Lindholm LH, Ibsen H, Dahlöf B, Devereux RB, Beevers G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristiansson K, Lederballe-Pedersen O, Nieminen MS, Omvik P, Oparil S, Wedel H, Aurup P, Edelman J, Snapinn S . Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359: 1004–1010.
Bakris GL, Toto RD, McCullough PA, Rocha R, Purkayastha D, Davis P . Effects of different ACE inhibitor combinations on albuminuria: results of the GUARD study. Kidney Int 2008; 73: 1303–1309.
Derosa G, Querci F, Franzetti I, Dario Ragonesi P, D'Angelo A, Maffioli P . Comparison of the effects of barnidipine+losartan compared with telmisartan+hydrochlorothiazide on several parameters of insulin sensitivity in patients with hypertension and type 2 diabetes mellitus. Hypertens Res 2015; 38: 690–694.
Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, Velazquez EJ, Dahlöf B, Kelly RY, Hua TA, Hester A, Pitt B . Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010; 56: 77–85.
Oxlund CS, Henriksen JE, Tarnow L, Schousboe K, Gram J, Jacobsen IA . Low dose spironolactone reduces blood pressure in patients with resistant hypertension and type 2 diabetes mellitus: a double blind randomized clinical trial. J Hypertens 2013; 31: 2094–2102.
Saito A . The necessity and effectiveness of mineralocorticoid receptor antagonist in the treatment of diabetic nephropathy. Hypertens Res 2015; 38: 367–374.
Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P, Anderson C . Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
Fried LF, Emanuelle N, Zhang JH, Brophy M, Conner TA, Duckworth W, Leehey DJ, McCullough PA, O'Connor T, Palevsky PM, Reilly RF, Seliger SL, Warren SR, Watnick S, Peduzzi P, Guarino P . Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 2013; 369: 1892–1903.
Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, Chaturvedi N, Persson F, Desai AS, Nicolaides M, Richard A, Xiang Z, Brunel P, Pfeffer MA . Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med 2012; 367: 2204–2213.
Wu Z, Jin C, Vaidya A, Jin W, Huang Z, Wu S, Gao X . Longitudinal patterns of blood pressure, incident cardiovascular events, and all-cause mortality in normotensive diabetic people. Hypertension 2016; 68: 71–77.
Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, Kolloch R, Benetos A, Pepine CJ . Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med 2006; 144: 884–893.
Kai H, Ueno T, Kimura T, Adachi H, Furukawa Y, Kita T, Imaizumi T . Low DBP may not be an independent risk for cardiovascular death in revascularized coronary artery disease patients. J Hypertens 2011; 29: 1889–1896.
Kai H, Kimura T, Fukuda K, Fukumoto Y, Kakuma T, Furukawa Y . Impact of low diastolic blood pressure on risk of cardiovascular death in elderly patients with coronary artery disease after revascularization - The CREDO-Kyoto Registry Cohort-1. Circ J 2016; 80: 1232–1241.
Nesto RW, Bell D, Bonow RO, Fonseca V, Grundy SM, Horton ES, Le Winter M, Porte D, Semenkovich CF, Smith S, Young LH, Kahn R . Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care 2004; 27: 256–263.
Kjekshus J, Gilpin E, Cali G, Blackey AR, Henning H, Ross J Jr . Diabetic patients and beta-blockers after acute myocardial infarction. Eur Heart J 1990; 11: 43–50.
Tsujimoto T, Sugiyama T, Noda M, Kajio H . Intensive glycemic therapy in type 2 diabetes patients on β-blockers. Diabetes Care 2016; 39: 1818–1826.
Giugliano D, Acampora R, Marfella R, De Rosa N, Ziccardi P, Ragone R, De Angelis L, D'Onofrio F . Metabolic and cardiovascular effects of carvedilol and atenolol in non-insulin-dependent diabetes mellitus and hypertension: a randomized, controlled trial. Ann Intern Med 1997; 126: 955–959.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT . A randomized trial of intensive vs. standard blood-pressure control. N Engl J Med 2015; 373: 2103–2116.
Brunström M, Carlberg B . Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ 2016; 352: i717.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A . Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 2015; 313: 603–615.
Adamsson Eryd S, Gudbjörnsdottir S, Manhem K, Rosengren A, Svensson AM, Miftaraj M, Franzén S, Björck S . Blood pressure and complications in individuals with type 2 diabetes and no previous cardiovascular disease: national population based cohort study. BMJ 2016; 354: i4070.
American Diabetes Association. Cardiovascular disease and risk management. Diabetes Care 2017; 40 (Suppl 1): S75–S87.
Bangalore S, Fakheri R, Toklu B, Messerli FH . Diabetes mellitus as a compelling indication for use of renin angiotensin system blockers: systematic review and meta-analysis of randomized trials. BMJ 2016; 352: i438.
Grossman A, Grossman E . Blood pressure control in type 2 diabetic patients. Cardiovasc Diabetol 2017; 16: 3.
Tikkanen I, Chilton R, Johansen OE . Potential role of sodium glucose cotransporter 2 inhibitors in the treatment of hypertension. Curr Opin Nephrol Hypertens 2016; 25: 81–86.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015; 373: 2117–2128.
Sattar N, McLaren J, Kristensen SL, Preiss D, McMurray JJ . SGLT2 inhibition and cardiovascular events: why did EMPA-REG Outcomes surprise and what were the likely mechanisms? Diabetologia 2016; 59: 1333–1339.
Kimura G . Diuretic action of sodium-glucose cotransporter 2 inhibitors and its importance in the management of heart failure. Circ J 2016; 80: 2277–2281.
Acknowledgements
This work was supported by JSPS KAKENHI Grant number 16K09468.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
HK has received lecture fees from Daiichi Sankyo, Mitsubishi Tanabe Pharma, MSD KK, Sumitomo Dainippon Pharma, Takeda Pharmaceutical and Toa Eiyo.
Rights and permissions
About this article
Cite this article
Kai, H. Blood pressure management in patients with type 2 diabetes mellitus. Hypertens Res 40, 721–729 (2017). https://doi.org/10.1038/hr.2017.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.55
Keywords
This article is cited by
-
Low blood pressure and cardiovascular events in diabetic patients with coronary artery disease after revascularization: the CREDO-Kyoto registry cohort-1
Hypertension Research (2020)
-
Nationwide Survey on Actual Interventions for Type 2 Diabetes by Japanese Practitioners (NSAID Study-1): Glycemic, Weight, and Blood Pressure Management
Diabetes Therapy (2020)
-
The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019)
Hypertension Research (2019)