Abstract
Arterial pulse wave velocity (PWV) depends on blood pressure (BP). Correction of PWV for BP is commonly performed using a statistical approach, requiring a patient cohort. We recently developed a mechanistic, model-predictive approach to assess BP-independent changes in carotid PWV (cPWV) at the level of the individual. The goal of the present study is to compare our novel technique to conventional statistical correction, in the context of anti-cancer therapy using anti-angiogenic drugs (AADs). AADs frequently lead to a PWV increase, but also to hypertension, underlining the need for BP correction of PWV measurements. We obtained carotid artery systolic and diastolic cross-sectional areas (echotracking) and corresponding BPs (tonometry) in 48 patients before starting AAD treatment (sorafenib/sunitinib), and at four follow-up visits spaced 2 weeks apart. For each patient, we derived cPWV and a baseline single-exponential BP cross-sectional area curve. Based on these baseline curves and follow-up BPs, we predicted cPWV at follow-up due to BP. By comparing predicted and measured cPWVs at follow-up, we assessed the BP-independent cPWV increase. In the same way, we assessed whether diastolic cross-sectional area (Ad) changed beyond the BP-induced amount. The AAD-induced BP-independent increase in cPWV was 0.43(0.09,0.77) m s–1 (mean (95%CI), P=0.014, mechanistic approach) and 0.48(0.14,0.82) m s–1 (P=0.006, statistical approach). Ad increased with 1.92(0.93,2.92) mm2 (P<0.001) and 2.14(1.06,3.23) mm2 (P<0.001), respectively. In conclusion, the present study demonstrates the feasibility and potential of our mechanistic, model-predictive approach to quantify BP-independent effects on arterial stiffness at the level of the individual, in a clinically relevant setting of AAD therapy.
Similar content being viewed by others
Introduction
Anti-angiogenic drugs (AADs) are increasingly used in anti-cancer therapy.1 We recently showed that AADs lead to an increase in local carotid pulse wave velocity (cPWV),2 a measure of large artery stiffening. Furthermore, AAD treatment frequently leads to hypertension.3 Since PWV is known to depend on blood pressure (BP),4, 5, 6, 7 the increased cPWV does not directly reflect intrinsic large artery stiffening. Therefore, using PWV to assess intrinsic arterial stiffness requires consideration of BP.
In a recent study, we demonstrated that by using distensibility measurements at carotid level and a mechanistic approach, it is possible to assess the BP effect on cPWV in the individual patient, rather than adjusting for BP at the group level.8 This approach is based on a single-exponential relationship that is fitted to arterial pressure–area measurements, and allows estimation of any changes in stiffness due to changes in wall material and not due to BP.
In the present study, we will use our novel mechanistic approach to quantify the BP-independent effect of AADs on large artery stiffness. We will compare this novel mechanistic approach to the conventional, exclusively statistical correction for BP effects, and discuss the differences between these two methods.
Methods
Study population and measurements
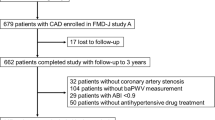
The population and measurements used in this study were elaborately described previously.2 Briefly, patients in whom treatment with AADs (sorafenib or sunitinib) was indicated were recruited at a secondary unit dedicated to care of metastatic cancer patients (Figure 1 in Alivon et al.2). Patients were investigated during day hospitalisation for chemotherapy administration, at baseline, after 7–10 days of AADs (follow-up 1) and then every 2 weeks for 6 weeks (follow-ups 2–4). At each visit, brachial diastolic (DBP), mean (MAP) and systolic (SBP) BPs were recorded in triplicate using an oscillometric device (Dinamap, GE Medical, Tampa, Florida, USA). If AADs induced hypertension, the consulting physician put patients on anti-hypertensive drugs. Systolic, mean and diastolic pressures were averaged over the three acquired measurements by calculating the average. In addition, carotid artery ultrasonic wall tracking was performed (Artlab; Esaote Pie-Medical, Maastricht, the Netherlands).2 Local carotid artery pulse pressure was calculated using the carotid applanation tonometry waveform recorded with a SphygmoCor device (Atcor Medical, Sydney, Australia).2 This approach assumes carotid DBP and MAP to equal brachial DBP and MAP.9 Patients provided written informed consent before baseline testing. The study protocol was performed within the Angiogenesis Inhibitors Study and Research Centre (CERIA) and was approved by the Cochin Ethics committee (approval number 12804766).
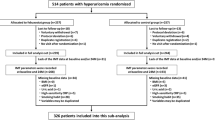
Study set-up. At baseline (top row), subjects were measured before onset of anti-angiogenic drugs (AADs). Directly after the baseline measurement, and before follow-up visits (bottom row) subjects were put on AADs. During both baseline and follow-up visits, measurements (left column) were performed which included carotid artery tonometry and ultrasound wall tracking. These yielded diastolic (DBP, Ad) and systolic (SBP, As) pressure–area points (left column). At baseline, an exponential pressure–area curve was modelled through these points (top right) for each subject individually. At follow-up, this (unchanged) curve, together with follow-up pressures, was used to predict diastolic and systolic cross-sectional areas (Adpred and Aspred, bottom right). Measured carotid pulse wave velocity (cPWV) was calculated using measured A's, whereas predicted cPWV (cPWVpred) was calculated using predicted A's (legend). In both cases the Bramwell–Hill equation is used.17 The difference between measured and predicted cPWVs (ΔcPWV) was calculated by subtracting cPWVpred from cPWV. Similarly, ΔAd was calculated by subtracting Adpred from Ad. ρ refers to blood mass density; ‘area’ refers to the artery lumen cross-sectional area.
Data quality
Ultrasonic wall tracking as well as tonometry measurements were performed by researchers who had been trained by a highly experienced investigator (PB) for ⩾2 weeks. This training period was concluded if in a reproducibility study in ⩾15 patients the short-term coefficient of variation (between investigators) was <3% for diameter, <6% for distension and <4% for PWV. Furthermore, in the present study, quality of the applanation tonometry measurements was assessed using the operator index, only keeping measurements with an operator index >80. In two exceptional conditions, measurements with a lower operator index were retained: (1) if the wave shape appeared regular but only the end-diastolic pressure curve showed beat-to-beat variability; or (2) if the low operator index was caused by one outlying beat (an extrasystole).
Data processing
Data processing was performed using the software R, version 3.2.3.10
Carotid stiffness calculation
Cross-sectional areas of the carotid artery lumen were calculated from the media-adventitia echo diameter using A=π × (diameter/2)2 at diastole (Ad) and systole (As). cPWV was calculated using the Bramwell–Hill relationship:11

with ρ=1.050 kg l–1 the blood mass density, and SBP and DBP the systolic and diastolic brachial BPs, respectively.
Uncorrected effect of AADs on BPs, cPWV and Ad
The uncorrected effect of AADs on BPs, cPWV and Ad was assessed using mixed-effects models (R nlme package version 3.1–125)12 of the form:

where par is brachial SBP, carotid SBP, MAP, DBP, cPWV or Ad, respectively. AAD is a Boolean variable indicating the use of AADs, and is therefore coded 0 for the baseline visit and 1 for all follow-up visits. Therefore, β0 represents the average value of par at baseline, and β1 represents the average AAD-induced change in par over all follow-up visits.
Mixed-effects modelling has the distinct advantage over, for example, repeated-measures analysis of variance that it can handle missing data points, maximising the use of all available data. Furthermore, mixed-effects modelling has proven to be very robust against non-normality of residuals.13 The most appropriate covariance structure was determined for each model by likelihood-ratio comparison of 8 models with different covariance structures.14 Likelihood-ratio tests were used to compare the different covariance structures.14, 15 After the most suitable covariance structure was found, significance of fixed model terms was assessed by likelihood-ratio comparison of successively more complicated models.
Mechanistic approach
Pressure–area curve description. The diastolic and systolic pressure–area (P–A) points obtained at baseline (before anti-angiogenic treatment) were used to fit an established mathematical description of the P–A relation, that is, a single-exponential model:16


where Pref and Aref indicate reference diastolic BP and cross-sectional area, respectively. In this study, Pref=100 mm Hg was chosen
Model predictions of cPWV and Ad at follow-up. For each individual patient, we predicted Ad (Ad,pred) and As (As,pred) at follow-up based on the baseline P–A curves (Equation (4) and follow-up BPs (Figure 1). Subsequently, predicted cPWV (cPWVpred) was obtained from Equation (1), using follow-up BPs and predicted cross-sectional areas (Ad,pred and As,pred). This was done under the explicit assumption that between baseline and follow-up the P–A relationship had remained unaltered. Therefore, any difference between measured and predicted cPWV or Ad signifies a change in intrinsic wall properties and is not a BP effect
Mixed-effects modelling to assess statistical significance of cPWV and Ad predictions. The BP-independent effect of AADs on carotid artery stiffness was analysed by calculating the difference between predicted (cPWVpred) and measured cPWV at each follow-up visit, which was termed ΔcPWV. An initial mixed-effects model with ΔcPWV as dependent variable was fitted to the data:

containing:
-
1
An intercept (parameter β0).
-
2
The visit number as a categorical variable (parameters β1–β3), which was added by means of three dummy variables (
 ), for which deviation coding was used. As there are four follow-up visits, there are three dummy variables.
), for which deviation coding was used. As there are four follow-up visits, there are three dummy variables. -
3
Use of anti-hypertensive drugs (parameter β4), as a Boolean variable (AHD), which was also deviation-coded.
Baseline data points were not used in fitting the models, since these per definition only contain zeroes (ΔcPWV=0 at baseline) and lead to numerical problems in model fitting. Notably, the use of deviation coding for the categorical and Boolean variables ensures that the model's intercept term corresponds to the grand mean of the model. Therefore, in the current formulation, a (positive) significant intercept term indicates that ΔcPWV is significantly larger than 0. The latter implies that measured cPWV is significantly larger than predicted cPWV, indicating a BP-independent increase in cPWV at follow-up. Using the fixed model terms as described in Equation (5), the most appropriate covariance structure was determined.14, 15
Difference between Ad prediction and measurement. The BP-independent effect of AAD treatment on carotid diastolic cross-sectional area (ΔAd=Ad–Adpred) was analysed using the same scheme as for the ΔcPWV analysis (see above).
Conventional, entirely statistical approach
Correcting for the BP dependency of cPWV. Conventionally, PWV is corrected for BP using a statistical model. In the present study, we replicated such an approach. We fitted the following initial mixed-effects model to the data:

In contrast to the mixed-effects models used in our mechanistic approach, cPWV (Equation (6)is fitted to all five visits, including the baseline visit. Note that the dependent parameter is now cPWV instead of ΔcPWV as in Equation (5). AAD is a Boolean variable indicating the use of AADs, and is therefore coded 0 for the baseline visit and 1 for all follow-up visits. Note that while each patient has five visits, there are only three visit dummy parameters present. This is necessary, as AAD also functions as a visit dummy variable, effectively distinguishing between baseline and follow-up visits. For the coding of AAD and  , see Supplementary Table S4. The most suitable covariance structure was again estimated from eight potential candidates.14
, see Supplementary Table S4. The most suitable covariance structure was again estimated from eight potential candidates.14
Correcting for the BP dependency of Ad. Exactly the same, entirely statistical approach that was used to estimate the BP-independent effect of AADs on cPWV (see previous paragraph) was used to estimate the BP-independent effect of AADs on Ad.
Results
Patient population
The same patient data as in Alivon et al.2 were used. In the present study, only subjects with complete baseline measurements (echotracking, carotid tonometry and BP; see below) were included (n=48). General characteristics of this group are outlined in Table 1. At the follow-up visits, n=39 (follow-up 1), n=30 (follow-up 2), n=31 (follow-up 3), and n=23 (follow-up 4) measurements were included.
Uncorrected effects of AADs on BPs, cPWV and Ad
Table 2 shows the estimated, uncorrected effects of AADs on BPs, cPWV, and Ad. AADs increased cPWV and Ad by 0.75 m s–1 and 2.7 mm2 on average, respectively (both P<0.001). However, all BP measures also significantly increased (P⩽0.006). This could potentially explain the increased cPWV and Ad that were measured, and emphasises the need for a method to correct for BP. Heart rate was not influenced by AADs (P=0.602).
Main findings of mechanistic and conventional, statistical BP correction approaches
Using our mechanistic approach, for each subject, the difference between measured and predicted cPWV (ΔcPWV) was calculated. For the predicted cPWV values, strictly no change in wall behaviour is assumed, that is, the P–A relationship remains unaltered. All differences between measured and predicted cPWVs are therefore assumed to be caused by intrinsic wall changes. Mixed-effects modelling was used to investigate the statistical significance of ΔcPWV. We found that AADs lead to a BP-independent increase in ΔcPWV of 0.43(0.09,0.77) m s–1 (P=0.014, Table 3). The change in cPWV was also assessed by an exclusively statistical approach, which resulted in a cPWV change of 0.48(0.14,0.82) m s–1 (P=0.006, Table 3).
Our mechanistic approach was also used to investigate the BP-independent effect of AADs on diastolic cross-sectional area (Ad). We found that AADs lead to an increase in ΔAd of 1.92(0.93,2.92) mm2 (P<0.001, Table 3). Using the exclusively statistical approach, this change was estimated at 2.14(1.06,3.23) mm2 (P<0.001, Table 3).
Mechanistic approach: changes in intrinsic carotid artery stiffness with the use of anti-angiogenic medication
Supplementary Table S1 contains the full analysis results discussed in this section. Mixed-effects modelling was used to investigate the effect of AADs on ΔcPWV, as well as the potential effects of anti-hypertensive medication and the potential difference in ΔcPWV between follow-up visits. Model 1 in Supplementary Table S1 (of which β0 is reproduced in Table 3) represents the mixed-effects model with the simplest fixed-effects structure, that is, only an intercept. The magnitude of the intercept term indicates that measured cPWVs are on average 0.43 m s–1 higher than predicted cPWVs, at P=0.014. Addition of other model terms (distinguishing between follow-up visits and/or between the use of anti-hypertensive medication) did not significantly improve the statistical model (Supplementary Table S1, right column: likelihood-ratio tests are all non-significant).
Mechanistic approach: changes in intrinsic carotid artery diameter with the use of anti-angiogenic medication
Supplementary Table S2 contains the full analysis results discussed in this section. Again, for the predicted Ad values, strictly no change in wall behaviour is assumed. The same mixed-effects modelling approach as for cPWV was used. Model 1 in Supplementary Table S2 (of which β0 is reproduced in Table 3) represents the mixed-effects model with the simplest fixed-effects structure, that is, only an intercept. The magnitude of the intercept term indicates that measured Ads are on average 1.9 mm2 higher than predicted from the BP increase, at P<0.001. Addition of other model terms (distinguishing between follow-up visits and/or between the use of anti-hypertensive medication) again did not significantly improve the statistical model.
Changes in diastolic BP with the use of anti-angiogenic medication
Supplementary Table S3 contains the full analysis results discussed in this section. As an internal check, we assessed whether DBP did indeed increase with AAD, and whether this increase differed between follow-up visits and between people that did or did not use anti-hypertensive drugs. Supplementary Table S3 shows mixed-effects models comparing DBP at each of the follow-up visits to baseline. Model #1 shows that at the follow-up visits, DBP was 6.0 mm Hg higher than at baseline (P<0.001). Addition of other model terms (distinguishing between follow-up visits and/or between the use of anti-hypertensive medication) did not significantly improve the statistical model.
Conventional, entirely statistical approach: correcting for the BP dependency of cPWV
Supplementary Table S5 contains the full analysis results discussed in this section. In addition to our novel mechanistic methodology, we assessed the effects of AADs on cPWV by means of a statistical approach, without prediction of follow-up cPWVs. Supplementary Table S5 shows the results of a series of mixed-effects model fits. As expected, DBP had a significant influence on cPWV (addition of a DBP term improved the model, P=0.010, model #2vs. #1). Additional inclusion of a quadratic DBP term did not statistically significantly improve the model (P=0.288, model #3vs. #2). Nevertheless, we chose to continue statistical modelling with (models #5 and #7) and without (models #4 and #6) a quadratic DBP term. Distinguishing between visits improved the model (P=0.002, model #4vs. #2 and P=0.003, model #5vs. 3). Addition of a term accounting for the presence of anti-hypertensive medication did not improve the model, whether it was to a model without a quadratic DBP term (P=0.468, models #6vs. #4), or to a model with a quadratic DBP term (P=0.568, models #7vs. #5).
From a strictly statistical point of view (only keeping model terms that significantly improve the statistical model), model #4 (Supplementary Table S5) best describes our results. This model indicates an AAD-induced increase in cPWV of 0.52 m s–1. However, as there is a known nonlinear dependence of cPWV on DBP, using a model that corrects for DBP quadratically provides additional BP correction (model #5, of which β1 is reproduced in Table 3). This model indicates an AAD-induced increase in cPWV of 0.48 m s–1.
Conventional, entirely statistical approach: correcting for the BP dependency of Ad
Supplementary Table S6 contains the full analysis results discussed in this section. Supplementary Table S6 shows the results of a series of mixed-effects model fits that assess the AAD-induced change in Ad on a statistical basis. The influence of DBP on Ad is statistically non-significant (P=0.105, model #2vs. #1). However, there is a clear, direct, mechanical relationship between pressure and lumen cross-sectional area. Addition of a quadratic term is again statistically non-significant (P=0.168, model #3vs. #2), albeit that physiologically, the relationship between Ad and pressure is known to be nonlinear (see, for example, Equation (3). We have chosen to continue our statistical modelling again on ‘physiological grounds’, keeping in both the DBP and DBP2 terms (models #5 and #7), as well as performing parameter inclusion strictly statistically, omitting DBP terms altogether (models #4 and #6). Neither distinguishing between visits (P=0.553, model #4vs. #1 and P=0.673, model #5vs. #3) nor accounting for the presence of anti-hypertensive medication (P=0.584, model #6vs. #1 and P=0.584, model #7vs. #3) improved our models.
From a strictly statistical point of view (only keeping model terms that significantly improve it), model #1 (Supplementary Table S6) best describes our results. This model indicates an AAD-induced, BP-corrected increase in Ad of 2.67 mm2. However, to obtain a physically warranted BP correction, a model should be used that corrects for the nonlinear dependence of Ad on DBP (model #3, of which β1 is reproduced in Table 3). The latter model indicated an AAD-induced, BP-corrected increase in Ad of 2.14 mm2.
Discussion
In the present study, we investigated the effect of AADs on arterial stiffness as quantified by cPWV. As cPWV is known to vary heavily with BP,5, 6, 7, 17 one has to correct cPWV for this potential confounder. Recently, we published a study in which we quantified the BP effect on cPWV on a mechanistic basis, and proposed a way of correcting for this effect.8 We applied this mechanistic correction approach to the data in the present study, and found that AAD treatment leads to a BP-independent increase in cPWV of 0.43 m s–1. With AAD treatment, arterial lumen cross-sectional area showed a BP-independent increase of 1.9 mm2. We compared these findings obtained using our mechanistic approach to the results of the conventional approach of statistical correction. When correcting for a quadratic dependence of cPWV and Ad on DBP, we found an AAD-induced increase of 0.48 m s–1 in cPWV and 2.1 mm2 in Ad. These numbers are similar to those obtained using our mechanistic approach, confirming that our mechanistic, model-driven methodology yields BP-corrected estimates of cPWV and Ad that are very similar to their statistically predicted counterparts. The advantage of our mechanistic methodology, however, is that it provides a pressure-independent estimation of cPWV and Ad at the level of the individual, which is crucial for clinical management.
In our previous paper,8 we used three pressure–area points (diastolic, dicrotic notch and systolic) to fit the curvilinear relationship between pressure and area. In the present study, dicrotic notch detection in the pressure and diameter signals was unavailable due to technical limitations, and therefore we resorted to a two-point approach. Our results show that the pressure dependence of cPWV can also be reasonably captured using a two-point approach, although we could not establish the possible quantitative consequences in the present study.
While mean arterial pressure is often used in correcting for BP, from a physical point of view, diastolic BP may be the actual parameter that is the main determinant of the velocity of the BP wave.4, 18 We therefore chose to present findings based on statistical correction using diastolic BP in the main text of this paper. As the choice between diastolic and mean pressure for correcting PWV is subject of ongoing discussion, we have also performed statistical BP corrections based on mean arterial pressures. Results from these analyses are presented in Supplemental Digital Content 1, Supplementary Tables S7 and S8, and lead to an AAD effect on cPWV and Ad of 0.46 m s–1 and 2.3 mm2, respectively. These results differ only minimally from statistical results obtained using DBP as correction variable.
In our approach, predictions of cPWV and Ad at all follow-up visits are based on the baseline P–A curve. This renders subsequent measurements dependent on the baseline value. P–A curves were based on one diastolic and one systolic P–A point. Therefore, any noise in the baseline measurements will have direct effects on the calculated predictions. We also established an averageP–A curve for each subject along all visits, and performed predictions using these average curves instead of baseline curves. This approach is elaborated in Supplemental Digital Content 2. Estimated, BP-independent changes in cPWV and Ad were 0.25 m s–1 and 1.92 mm2, respectively. These numbers are lower than those from our baseline curve-based method. This difference is caused by the statistical modelling approach that was chosen to estimate the most appropriate covariance structure (for details, see 14). In the method based on averageP–A curves, the baseline visit is also included in the model. This led to a more complicated covariance structure than in the original method, which reduced the magnitude of the estimated fixed effect of anti-angiogenic treatment.
Instead of calculating differences between measured and predicted cPWVs and Ads, one can also directly assess the parameters γ and Aref of the P–A curves. Results of these analyses are presented in Supplemental Digital Content 2. The increase in γ with anti-angiogenic treatment confirms the increase in pressure-independent stiffness as quantified by ΔcPWV; while the increase in Aref confirms the pressure-independent increase in diameter. The advantage of this method is that γ and Aref are directly pressure-independent, and no calculation of a difference between prediction and measurement is necessary. However, ΔcPWV gives the user a direct estimate of the stiffness change in cPWV units (that is, in metres per second), enabling direct comparison of the magnitude of ΔcPWV to absolute cPWV.
The structural changes underlying the increased stiffness and cross-sectional area of the carotid artery wall with AAD use are largely unknown. Several potential causes are discussed in our previous paper,2 which include potential vasoactive properties of sorafenib and sunitinib19 or their interaction with integrins, but also a potential effect of the AADs on the vasa vasorum, the microscopic arterial network that supply the artery wall with nutrients.20 It is beyond the scope of the present study to structurally explain the observed changes in carotid artery stiffness and diameter.
The carotid BP measurements used in this study are obtained by scaling the carotid artery applanation tonometry waveform, assuming that carotid diastolic and mean pressures are equal to brachial diastolic and mean pressures.9 This scaling method has two potential disadvantages: (1) it introduces additional measurement noise, and (2) it requires additional tonometry measurements by an experienced research nurse,21 complicating the measurement protocol. In addition to the present analyses, we additionally re-performed our mechanistic correction technique using brachial systolic and diastolic pressures. All results were essentially the same, except for the observation that the pressure-independent increase in ΔcPWV with AAD got smaller and lost statistical significance (β0=0.314 m s–1, P=0.075). This suggests that using brachial pressures instead of carotid yields an under-estimation of ΔcPWV.
The technique presented in this study can not only be applied to local cPWV, but also to carotid-femoral transit time PWV (cfPWV). Although with cfPWV the pressure–area relationship is not directly measured, the exponent of this relationship can be directly calculated from cfPWV and BP measurements. Using this exponent, cfPWV predictions based on BP changes can be made in the same was as for cPWV, and ΔcfPWV (the difference between measured and predicted cfPWV) can also be calculated, underlining the potential of our mechanistic method.
From the clinical perspective, cPWV as commonly obtained depends on BP, and can therefore not be used as an independent measure of intrinsic arterial stiffness. This BP dependence cannot be corrected for in a straightforward manner. In population studies, correction can be performed statistically. However, this requires a patient cohort for the statistical model to be quantified. Our study demonstrates that cPWV can also be corrected for BP in a mechanistic way. This method is applicable in individual patients, and can be used to assess an individual’s change in intrinsic arterial stiffness over time, independent of BP, and without the subject being part of a study cohort.
In conclusion, the present study demonstrates the feasibility and potential of our mechanistic, model-predictive approach to quantify BP-independent effects on arterial stiffness at the level of the individual, in a clinically relevant setting of AAD therapy.
References
Cao Y, Langer R . Optimizing the delivery of cancer drugs that block angiogenesis. Sci Transl Med 2010; 2: 15ps13.
Alivon M, Giroux J, Briet M, Goldwasser F, Laurent S, Boutouyrie P . Large artery stiffness and hypertension after antiangiogenic drugs: influence on cancer progression. J Hypertens 2015; 33: 1310–1317.
Wu S, Chen JJ, Kudelka A, Lu J, Zhu X . Incidence and risk of hypertension with sorafenib in patients with cancer: a systematic review and meta-analysis. Lancet Oncol 2008; 9: 117–123.
Bramwell JC, McDowall RJS, McSwiney B . The variation of arterial elasticity with blood pressure in man (part I). Proc R Soc Lond B 1923; 94: 450–454.
Steppan J, Sikka G, Hori D, Nyhan D, Berkowitz DE, Gottschalk A, Barodka V . Seeking a blood pressure-independent measure of vascular properties. Hypertens Res 2016; 39: 27–38.
Schillaci G, Battista F, Settimi L, Anastasio F, Pucci G . Cardio-ankle vascular index and subclinical heart disease. Hypertens Res 2015; 38: 68–73.
Spronck B, Avolio AP, Tan I, Butlin M, Reesink KD, Delhaas T . Arterial stiffness index beta and cardio-ankle vascular index inherently depend on blood pressure but can be readily corrected. J Hypertens 2017; 35: 98–104.
Spronck B, Heusinkveld MH, Vanmolkot FH, Roodt JO, Hermeling E, Delhaas T, Kroon AA, Reesink KD . Pressure-dependence of arterial stiffness: potential clinical implications. J Hypertens 2015; 33: 330–338.
Van Bortel LM, Balkestein EJ, van der Heijden-Spek JJ, Vanmolkot FH, Staessen JA, Kragten JA, Vredeveld JW, Safar ME, Struijker Boudier HA, Hoeks AP . Non-invasive assessment of local arterial pulse pressure: comparison of applanation tonometry and echo-tracking. J Hypertens 2001; 19: 1037–1044.
R Core TeamR: A language and Environment for Statistical Computing. Available at http://www.R-project.org/. Accessed on 11 March 2016.
Bramwell JC, Hill AV . The velocity of the pulse wave in man. Proc R Soc B 1922; 93: 298–306.
Pinheiro J, Bates D, DebRoy S, Sarkar D,, R Core Team.Nlme: Linear and Nonlinear Mixed Effects Models.Available at http://cran.r-project.org/package=nlme. Accessed on 11 March 2016.
Gelman A, Hill J . Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge University Press: Cambridge, UK. 2007.
Walavalkar V, Evers E, Pujar S, Viralam K, Maiya S, Frerich S, John C, Rao S, Reddy C, Spronck B, Prinzen FW, Delhaas T, Vanagt WY . Preoperative sildenafil administration in children undergoing cardiac surgery: a randomized controlled preconditioning study. Eur J Cardiothorac Surg 2015; 49: 1403–1410.
Zuur AF . Mixed Effects Models and Extensions in Ecology with R. Springer: New York, NY, USA. 2009.
Meinders JM, Hoeks AP . Simultaneous assessment of diameter and pressure waveforms in the carotid artery. Ultrasound Med Biol 2004; 30: 147–154.
Bramwell JC, Hill AV . The velocity of the pulse wave in man. Proc R Soc Lond B 1922; 93: 298–306.
Nichols WW, Nichols WW, McDonald DA . Mcdonald's Blood Flow in Arteries: Theoretic, Experimental, and Clinical Principles. CRC Press : London, UK. 2011.
Papadopoulou DN, Mendrinos E, Mangioris G, Donati G, Pournaras CJ . Intravitreal ranibizumab may induce retinal arteriolar vasoconstriction in patients with neovascular age-related macular degeneration. Ophthalmology 2009; 116: 1755–1761.
Stefanadis C, Vlachopoulos C, Karayannacos P, Boudoulas H, Stratos C, Filippides T, Agapitos M, Toutouzas P . Effect of vasa vasorum flow on structure and function of the aorta in experimental animals. Circulation 1995; 91: 2669–2678.
Spronck B, Delhaas T, Op 't Roodt J, Reesink KD . Carotid artery applanation tonometry does not cause significant baroreceptor activation. Am J Hypertens 2016; 29: 299–302.
Acknowledgements
BS was supported by a Kootstra Talent Fellowship awarded by Maastricht University and by an Endeavour Research Fellowship awarded by the Australian Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Spronck, B., Delhaas, T., De Lepper, A. et al. Patient-specific blood pressure correction technique for arterial stiffness: evaluation in a cohort on anti-angiogenic medication. Hypertens Res 40, 752–757 (2017). https://doi.org/10.1038/hr.2017.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.32
Keywords
This article is cited by
-
Model-based analysis of arterial pulse signals for tracking changes in arterial wall parameters: a pilot study
Biomechanics and Modeling in Mechanobiology (2019)
-
New approach to arterial stiffness: BP-independent local carotid stiffness
Hypertension Research (2017)



 ), for which deviation coding was used. As there are four follow-up visits, there are three dummy variables.
), for which deviation coding was used. As there are four follow-up visits, there are three dummy variables.